A lethal combination. simultaneous inferior and anterior STEMI with aborted sudden cardiac death and cardiogenic shock
#CardioTwitterCase originally published on Twitter
View this case of a 60-year-old male with hypertension as a modifiable cardiovascular risk factor. A history of thoracic surgery for a gunshot wound 40 years ago and no cardiovascular history.
This case was originally published on Twitter by @JuanGuzmnOlea2
Case description
Acute myocardial infarction involving two or more culprit lesions at the same time, known as double or combined infarction, is an extremely rare event with a grave prognosis. Here, we describe a case of a patient with acute myocardial infarction due to simultaneous occlusion of the RCA and LAD who presented with SCD and cardiogenic shock.
- A 60-year-old male with hypertension as a modifiable cardiovascular risk factor.
- A history of thoracic surgery for a gunshot wound 40 years ago and no cardiovascular history.
- He presented oppressive chest pain with irradiation to the left arm and dyspnea of more than 3 hours span.
However, the patient went to a non-PCI centre 9 hours later where an electrocardiogram was taken documenting ST-segment elevation in II, III, aVF and ST-segment depression in precordial leads (Figure 1).
Fibrinolytic therapy with tenecteplase was decided and the electrocardiogram at 60 minutes showed normalized ST-segment in inferior leads but now ST-segment elevation in V3, V4, V5, V6 (Figure 2).
Sudden cardiac death and cardiogenic shock
The patient was sent to the interventional cardiology department of our Hospital; nevertheless, during the transfer he presented sudden cardiac death that required resuscitation maneuvers and mechanic ventilation leading to sinus tachycardia and cardiogenic shock. He was admitted to the cathlab with blood pressure 80/40mmhg and norepinephrine vasopressor support. We do not have an Impella or other ventricular assist device, only IABP, so it was placed through the left femoral artery.
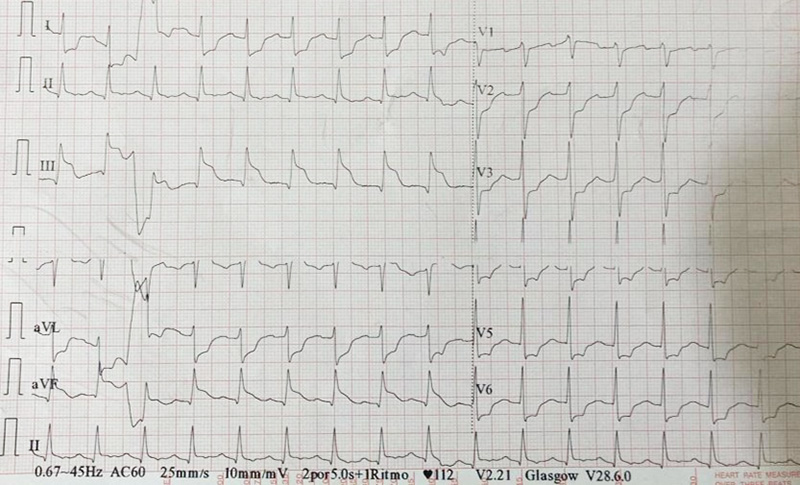
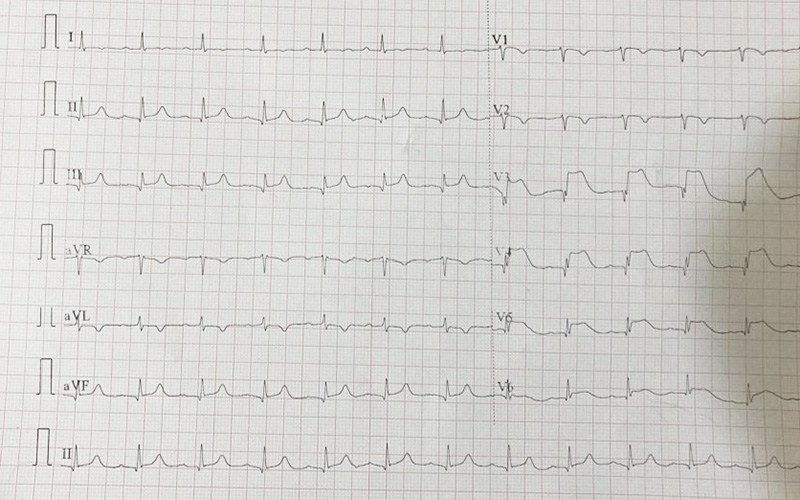
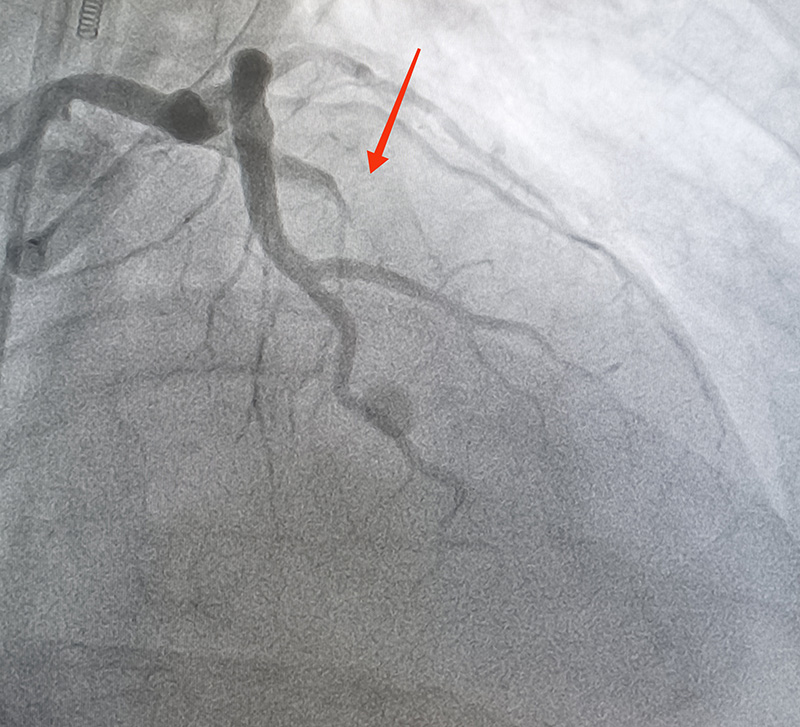
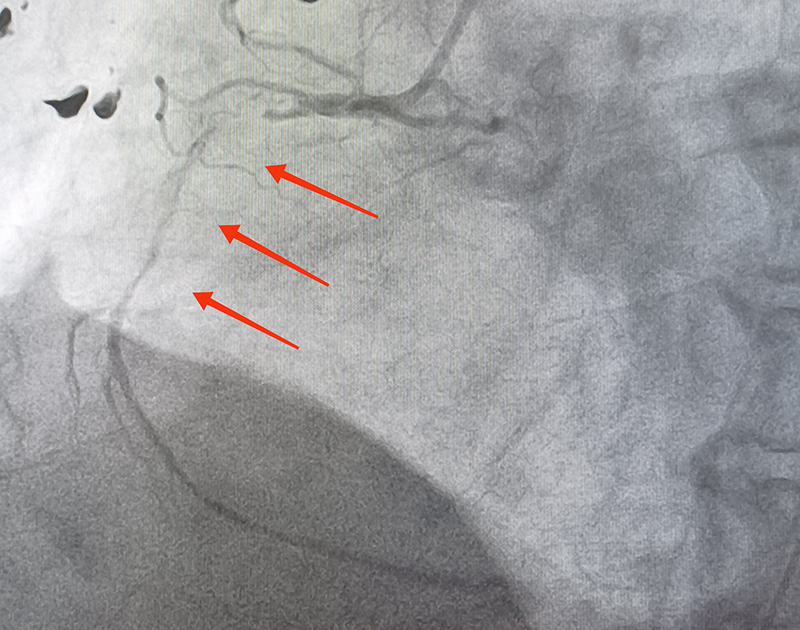
A 6Fr introducer sheath was placed in right common femoral artery and the coronary angiography revealed LAD with acute total occlusion and grade 5 thrombus in middle segment, normal LMCA and Circumflex. The RCA with 99% lesion in proximal segment and grade 4 thrombus with diffuse distal disease and TIMI 1 flow (Figures 3,4).
Full metal jacket
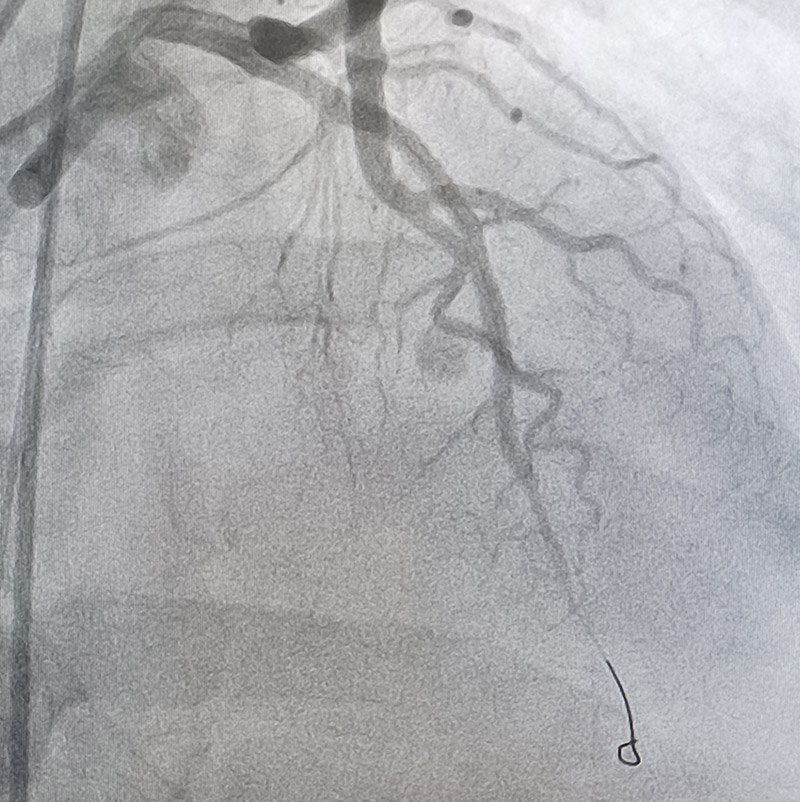
We proceeded to intervention, first used JL 3.5 6Fr guide catheter and advanced distally to LAD a 0.014” Runthrough floppy guidewire, then advanced a 2.0x15mm balloon, Dotter maneuver was done and predilated with luminal gain and distal flow, then advanced a 3.0x23 everolimus stent and was deployed at 20 atm. Due to the slow flow, we used intracoronary bolus of adenosine and GPIIb IIIa inhibitors with TIMI2 final flow.
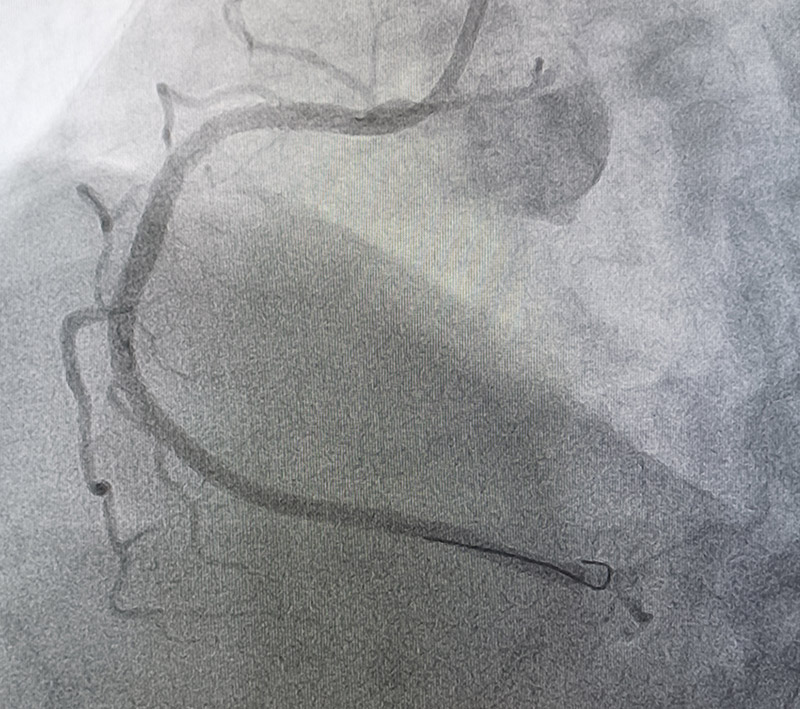
After that, the RCA was engaged with a JR4 6Fr guide catheter and advanced distally a 0.014” Runthrough floppy guidewire, then the occlusion site was predilated from distal to proximal with 2.0x15mm balloon and advanced 3.0x48mm everolimus stent from proximal segment and was deployed at 14 atm, however significant lesions were observed in the distal segment, so we decided to advance a 2.5x48mm everolimus stent and was deployed in distal segment at 13 atm and splice a third 2.75x24mm everolimus stent at 13 atm with TIMI3 final flow (“Full metal jacket”) (Figure 5,6) (Video 1).
He was sent to ICU, wherein, despite treatment, he continued with persistent cardiogenic shock and, unfortunately, died a few days later.
Images/Videos
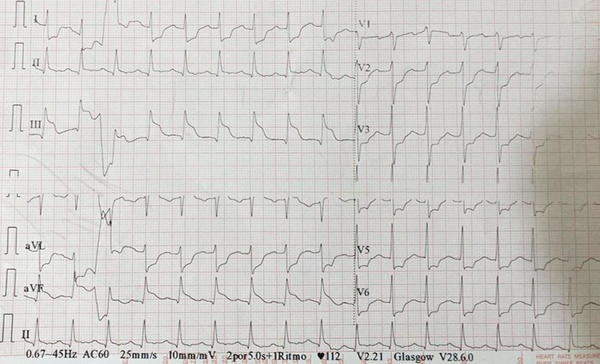
Figure 1: ST-segment elevation in II, III, aVF and ST-segment depression in precordial leads
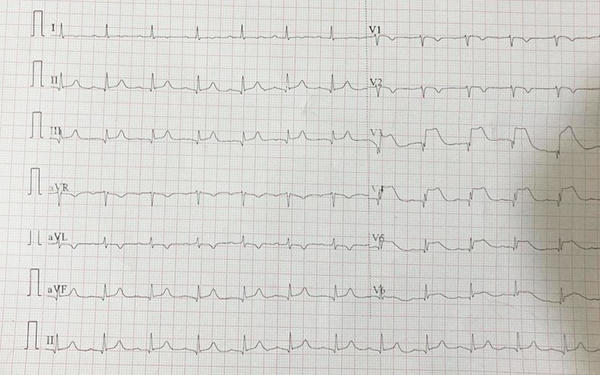
Figure 2: Electrocardiogram at 60 minutes showed normalized ST-segment in inferior leads but now ST-segment elevation in V3, V4, V5, V6
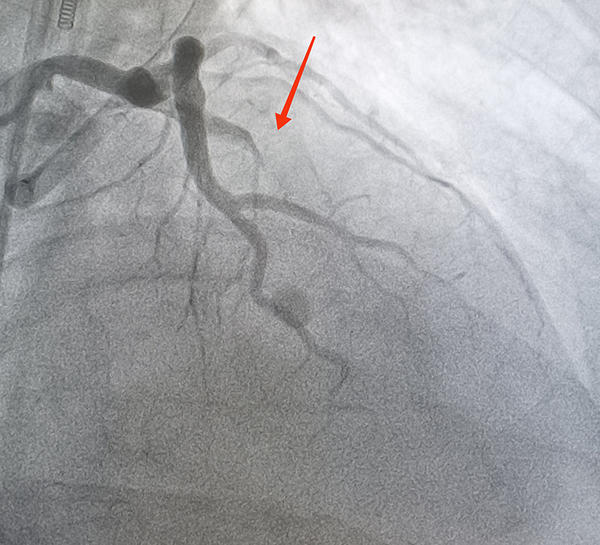
Figure 3: LAD with acute total occlusion and grade 5 thrombus in middle segment
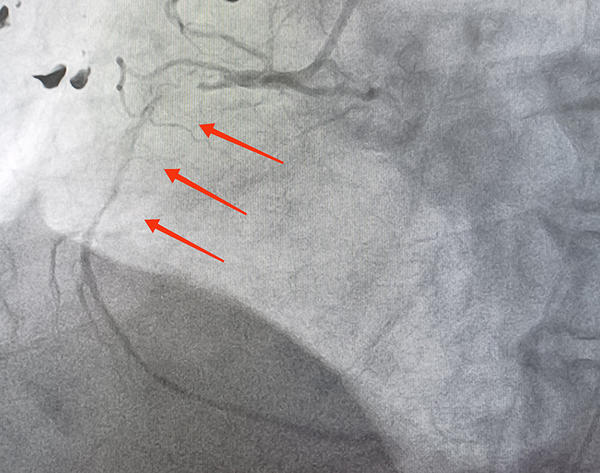
Figure 4:RCA with 99% lesion in proximal segment and grade 4 thrombus with diffuse distal disease and TIMI 1 flow
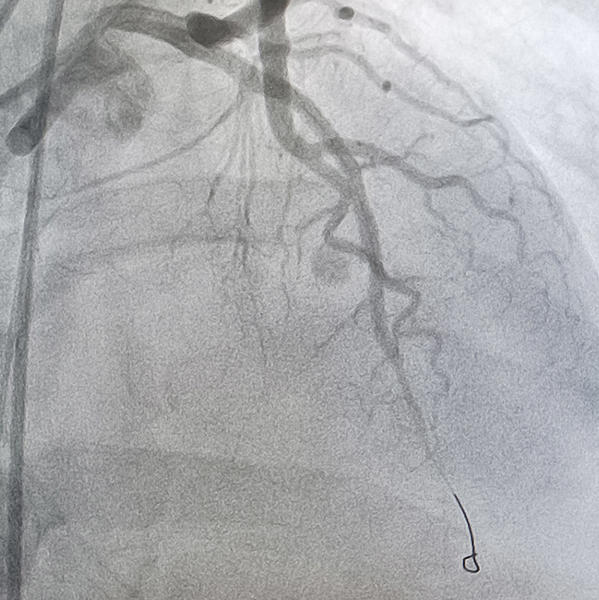
Figure 5: LAD with 3.0x23 everolimus stent with TIMI2 final flow
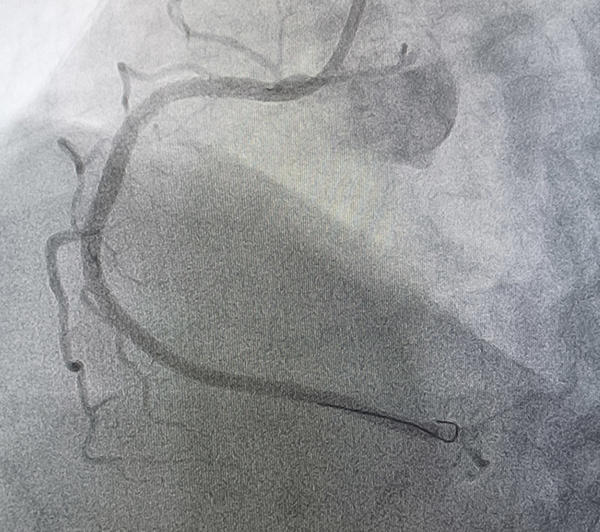
Figure 6: "Full metal jacket" in RCA with TIMI3 final flow
Final remarks
In the literature, the actual incidence of simultaneous or combined infarction is not known and studies are limited. Such a low incidence may be related to the fact that acute myocardial infarction with multiple vessel obstruction often causes extensive myocardial injury and death occurs before the patient arrives at the hospital. It is speculated that double infarction results from
- heightened inflammatory response and catecholamine surge caused by acute occlusion of one vessel, leading to occlusion of another vessel;
- hemodynamic instability and hypotension due to occlusion of one coronary artery, resulting in blood stasis and acute occlusion of another artery with a severe underlying lesion;
- prolonged coronary vasospasm (due to Prinzmetal angina or cocaine use
- hypercoagulable states including malignancy, hyperhomocysteinemia and thrombocytosis;
- coronary embolism and coronary arteritis.
The optimal management strategy in this type of patient is challenging and in spite of successful thrombolysis or PCI, a large percentage of patients die, and therefore they should be aggressively treated and extremely good supportive care is also needed.
Original tweet and Twitter discussion
A lethal combination. Simultaneous inferior and anterior STEMI with aborted sudden cardiac death and cardiogenic shock. @PCRonlinepic.twitter.com/NA9TcSBIfp
— Juan Guzmán Olea (@JuanGuzmnOlea2) August 10, 2022
Authors
Juan Guzmán Olea, Miguel Ángel Gómez Pluma, Gabriel Guzmán Olea, Juan Francisco Rodríguez Alvarado, Leticia Arizbeth Hernández Castro, Gonzalo Tolosa Dzul, Carlos Javier González Álvarez, Héctor Hugo Escutia Cuevas, Daniel Iván Pérez Vásquez



No comments yet!