Double barrel in CTO PCI
Supported by the EuroIntervention Journal
Authors*
Yvemarie B.O. Somsen1, Alexander Nap1, José P. Henriques2, Paul Knaapen1
Case summary
A 67-year-old male patient with stable angina was scheduled for elective percutaneous coronary intervention (PCI) of a chronic total coronary occlusion (CTO) of the right coronary artery (RCA).
A primary retrograde attempt in 2015 was unsuccessful; eight drug-eluting stents had been deployed from the neo-ostium to the posterolateral artery (PLA) without distal re-entry into true lumen, resulting in thrombolysis in myocardial infarction (TIMI) flow grade 0 (Panel A, moving image of panel A).
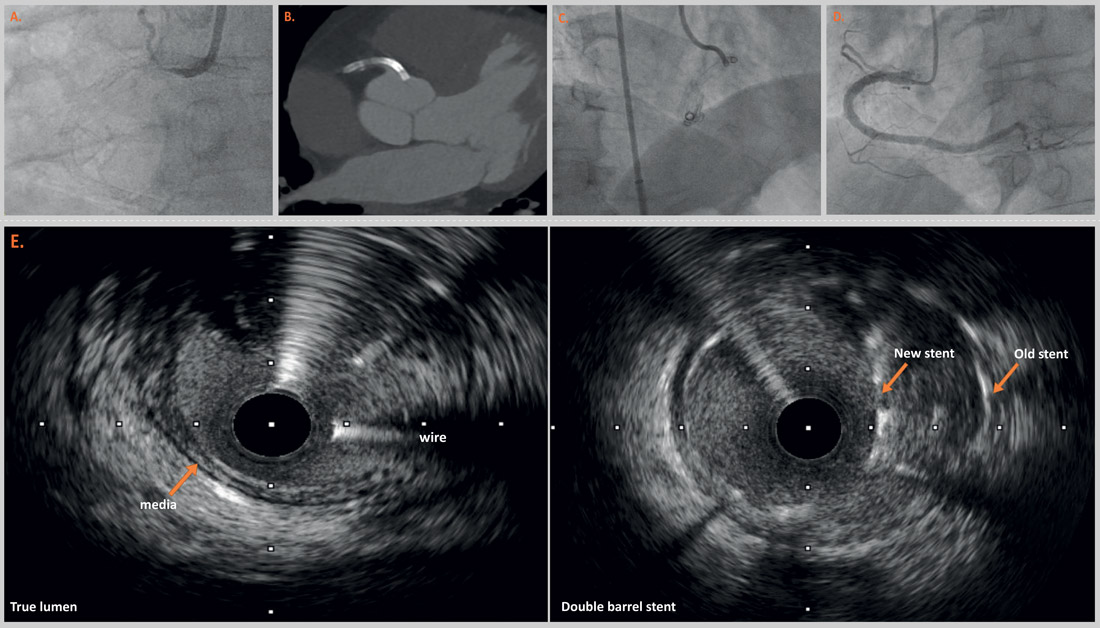
Figure 1: Double barrel in CTO PCI
Coronary computed tomography angiography (CCTA) confirmed that:
- the stents were not inside the lumen,
- all stents were occluded,
- the ostial stent protruded 5 mm into the aorta (Panel B).
In 2022, the patient was referred for a second PCI attempt due to invalidating angina. Reverse controlled antegrade and retrograde tracking technique was successfully performed by an experienced operator (Alex Nap) adjacent to the old stents. Intravascular ultrasound (IVUS) confirmed re-entry into the distal true lumen (Panel E), and guided stent sizing from the proximal RCA to the crux.
The final result showed two adjacent stents, which formed a distinct double barrel shape (Panel C, moving image of panel C). Additionally, the PLA branch was treated with antegrade dissection and re-entry technique (subintimal tracking and re-entry), without additional stenting due to the small caliber of the vessel. No complications occurred, and the patient was discharged the same day.
Angiographic follow-up at 4 months due to recurring angina showed good patency of the stents in the RCA (Panel D, moving image of panel D) with re-occlusion of the PLA branch, which was treated conservatively.
To the best of our knowledge, this case is the first description of a double barrel stent in CTO PCI. Previous studies reported the formation of a new lumen adjacent to stents in the subintimal space, forming a double barrel1-3. Our case differs from these reports, as two adjacent stents (one with re-entry, the other without) resulted in the unique double barrel shape. Our case highlights that confirmation of wire position in the true lumen following dissection and re-entry techniques is paramount in CTO PCI.
Both preprocedural and intracoronary imaging may guide the interventionalist in choosing the right strategy and material. CCTA may improve the operator’s understanding of complex anatomy4. Equally, intracoronary imaging (i.e. IVUS) may enhance CTO PCI by aiding adequate stent sizing, providing visual proof of re-entry into the true lumen, and recording stent malapposition or undersizing5,6.
Supplementary materials
References
- Roy J, Rees D, Ramsay D, Weaver J. Late Double-Barrel Lumen Following Successful CTO-PCI Using the Crossboss Stingray System. J Invasive Cardiol. 2017;29(2):E28-e9.
- Watanabe Y, Fujino Y, Ishiguro H, Nakamura S. Double-barrel coronary artery after subintimal stenting for chronic total occlusion. Cardiovascular Revascularization Medicine. 2017;18(5):361-3.
- Opolski MP, Wolny R, Dębski A, Witkowski A. Intravascular ultrasound-guided reconstruction of chronic total occlusion true lumen after failed subintimal tracking and re-entry. Kardiol Pol. 2023;81(1):70-1.
- Andreini D, Collet C, Leipsic J, Nieman K, Bittencurt M, De Mey J, Buls N, Onuma Y, Mushtaq S, Conte E, Bartorelli AL, Stefanini G, Sonck J, Knaapen P, Ghoshhajra B, Serruys P. Pre-procedural planning of coronary revascularization by cardiac computed tomography: An expert consensus document of the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr. 2022 Nov-Dec;16(6):558-572.
- Brilakis ES, Mashayekhi K, Tsuchikane E, Abi Rafeh N, Alaswad K, Araya M, Avran A, Azzalini L, Babunashvili AM, Bayani B, Bhindi R, Boudou N, Boukhris M, Božinović NŽ, Bryniarski L, Bufe A, Buller CE, Burke MN, Büttner HJ, Cardoso P, Carlino M, Christiansen EH, Colombo A, Croce K, Damas de Los Santos F, De Martini T, Dens J, Di Mario C, Dou K, Egred M, ElGuindy AM, Escaned J, Furkalo S, Gagnor A, Galassi AR, Garbo R, Ge J, Goel PK, Goktekin O, Grancini L, Grantham JA, Hanratty C, Harb S, Harding SA, Henriques JPS, Hill JM, Jaffer FA, Jang Y, Jussila R, Kalnins A, Kalyanasundaram A, Kandzari DE, Kao HL, Karmpaliotis D, Kassem HH, Knaapen P, Kornowski R, Krestyaninov O, Kumar AVG, Laanmets P, Lamelas P, Lee SW, Lefevre T, Li Y, Lim ST, Lo S, Lombardi W, McEntegart M, Munawar M, Navarro Lecaro JA, Ngo HM, Nicholson W, Olivecrona GK, Padilla L, Postu M, Quadros A, Quesada FH, Prakasa Rao VS, Reifart N, Saghatelyan M, Santiago R, Sianos G, Smith E, C Spratt J, Stone GW, Strange JW, Tammam K, Ungi I, Vo M, Vu VH, Walsh S, Werner GS, Wollmuth JR, Wu EB, Wyman RM, Xu B, Yamane M, Ybarra LF, Yeh RW, Zhang Q, Rinfret S. Guiding Principles for Chronic Total Occlusion Percutaneous Coronary Intervention. Circulation. 2019 Jul 30;140(5):420-433.
- Darmoch F, Alraies MC, Al-Khadra Y, Moussa Pacha H, Pinto DS, Osborn EA. Intravascular Ultrasound Imaging-Guided Versus Coronary Angiography-Guided Percutaneous Coronary Intervention: A Systematic Review and Meta-Analysis. J Am Heart Assoc. 2020;9(5):e013678.
*Affiliations
- Department of Cardiology, Amsterdam UMC, Vrije Universiteit Amsterdam, Amsterdam, the Netherlands.
- Department of Cardiology Amsterdam UMC, AMC, Amsterdam, the Netherlands.
Conflicts of interest
Nothing to disclose for all authors




No comments yet!