Pulmonary artery perforation after percutaneous left atrial appendage closure: possible mechanisms and red flags
Supported by the EuroIntervention Journal
Authors
Gabriele Tumminello1, Lucia Barbieri1, Andrea D'Errico1, Francesca Nespoli1,Stefano Carugo1
Case summary
The occlusion of the left atrial appendage (LAA) is an interventional technique for stroke prevention in patients affected by atrial fibrillation (AF). The LAA occlusion (LAAO) is a safe and effective procedure with a low incidence of intra and peri-procedural complications which however exist1.
The present clinical case involves a 66-year-old patient in sinus rhythm with paroxysmal AF and contraindication to anticoagulant therapy due to multiple episodes of intracranial bleeding.
A preoperative transoesophageal echocardiogram showed an aneurysm of the pulmonary artery (PA) trunk, with a close contiguity with the LAA (Figure 1A) found also in a previous chest computed tomography (CT) scan performed in 2019 (Figure 1B).
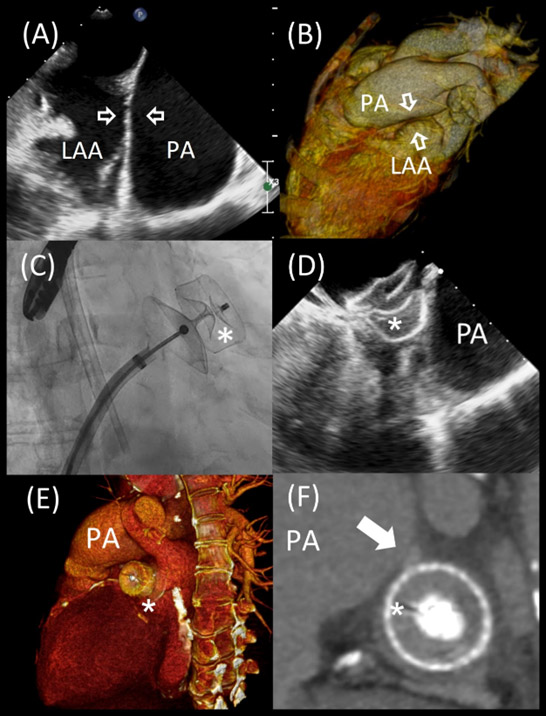
Figure 1: the monolobe left atrial appendage (LAA) and its close relationship with the dilated pulmonary artery (PA) trunk (blank white arrows) at echocardiogram (A) and CT-scan (B) before the procedure; the device (white * ) inside the LAA and its close relationship with the dilated PA trunk on X-ray (C) and echocardiogram (D) and CT scan reconstruction (E); a micro-aneurysm in the posterior PA wall (solid white arrows) compatible with the recent bleeding (F).
The non-invasively estimated PA systolic pressure (PAPs) was 45 mmHg. LAAO was performed implanting an Amulet LAA Occluder (Figure 1C). The device appeared well compressed and positioned (Figure 1D) in the absence of pericardial effusion.
Twenty-four hours after surgery, the patient was symptomatic for pericardial tamponade, treated with evacuative pericardiocentesis of haematic fluid. In the following hours, the effusion was persistently re-supplied, so the patient was transferred to the Cardiac Surgical Operating Room. The surgeoun found a continuous solution of the posterior PA, a point in anatomical contiguity with LAA that was repaired. No active LAA laceration or bleeding was evident (Video 1).
On transoesophageal echocardiographic control performed on postoperative 13th day, the device was shown to be well-positioned and stable within the LAA, as well as absence of pericardial effusion. A CT-scan confirmed the strict spatial relationship between the LAA/Device and the PA (Figure 1E), and a micro-aneurysm in the posterior PA wall, compatible with the recent bleeding, was identifiable (Figure 1F).
Risk factor for this kind of complication may be divided into: PA factors, LAA factors and Devices features. The strict contiguity between PA and the landing zone of the device inside the LAA is the first condition needed for this complication. This anatomical risk factor is present approximately in 33 % of the patients in a CT scan-based study2. Other PA risk factors include dimension, where a dilated PA may indicate a weakened vessel wall more susceptible to external injuries; PA elevated pressure may lead to an increased friction between the PA wall and the device. The elevated systolic PAPs is associated with postprocedural pericardial effusion3 after LAAO.
LAA risk factors include its anatomy and relative contiguity with PA; the sinus rhythm, and the relative contraction of LAA, should facilitate the hook penetration into LAA wall and the consequent PA erosion. Devices features include radial force and hooks shape. Amulet device respect to other devices demonstrated the highest radial outwards force4. The strength of the device may amplify the friction effect of the LAA on PA wall. Devices use hooks to anchor inside the LAA, which may hurts surrounding structures: new versions of devices, like Watchman Flex, have rounded hooks to minimizes the effect.
The perforation of PA after LAAO is a rare but possible complication with a high mortality rate up to 40 %5. The present clinical case highlights some anatomical, functional, and devices-related features which may be used as red flag in the LAAO procedure planning due to prevent this rare but serious complication.
References
- Glikson M, Wolff R, Hindricks G, Mandrola J, Camm AJ, Lip GYH, Fauchier L, Betts TR, Lewalter T, Saw J, Tzikas A, Sternik L, Nietlispach F, Berti S, Sievert H, Bertog S, Meier B. EHRA/EAPCI expert consensus statement on catheter-based left atrial appendage occlusion - An update. EuroIntervention. 2020 Jan 1;15(13):1133–80.
- Halkin A, Cohen C, Rosso R, Chorin E, Schnapper M, Biner S, Topilsky Y, Shiran A, Shmilovich H, Cohen D, Keren G, Banai S, Aviram G. Left atrial appendage and pulmonary artery anatomic relationship by cardiac-gated computed tomography: Implications for late pulmonary artery perforation by left atrial appendage closure devices. Heart Rhythm. 2016 Oct 1;13(10):2064–9.
- Zou T, Chen Q, Zhang L, Chen C, Ling Y, Liu G, Wang S, Pang Y, Xu Y, Cheng K, Zhou D, Zhu W, Ge J. Pulmonary artery pressure is associated with mid-term major adverse cardiovascular events and postprocedure pericardial effusion in atrial fibrillation patients undergoing left atrial appendage occlusion. Ann Transl Med 2021 Aug; 9(16):1324–1324.
- Menne MF, Schrickel JW, Nickenig G, Al-Kassou B, Nelles D, Schmitz-Rode T, Steinseifer U, De Backer O, Sedaghat A. Mechanical properties of currently available left atrial appendage occlusion devices: A bench-testing analysis. Artif Organs. 2019 Jul 1;43(7):656–65.
- Demkow M, Konka M, Witkowski A, Pracoń R, Ścisło P, Huczek Z, Burysz M, Ogorzeja W, Suwalski G, Kurowski A, Kępka C, Klisiewicz A, Michałowska I, Dzielińska Z, Nikodem Rudziński P, Kuśmierczyk M. How to Prevent Pulmonary Artery Wall Perforation Following Transcatheter Occlusion of Left Atrial Appendage. Journal of the American Society of Echocardiography. 2021 Feb 1;34(2):195-197.e2.
Affiliations
- Department of Cardio-Toracic-Vascular Diseases, Foundation IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Via Francesco Sforza, 35, 20122 Milano, Italy
- Department of Clinical Sciences and Community Health, University of Milan, 20122 Milan, Italy
Conflict of interest statement
None of the authors has any conflicts of interest to declare




No comments yet!