02 Mar 2022
How to perform a pericardial effusion puncture
Since increasing numbers of interventional procedures are performed, the incidence for a cardiologist to be faced with a PE has increased. This Toolkit displays a technique for a safe and controlled puncture of a PE/tamponade.
Frequency of the problem:
Expert level:
Summary
Pericardial effusion (PE) or pericardial tamponade can be punctured for diagnostic or hemodynamic reasons. This so-called pericardiocentesis can be performed under local anaesthesia using echocardiographic or fluoroscopic guidance. Different techniques exist for a pericardial puncture. There are three approaches for pericardial punctures; the subxiphoid approach, which is applied primarily, and the apical and parasternal approaches, which have higher risk for pneumothorax or ventricular puncture.
Since increasing numbers of interventional procedures are performed, the incidence for a cardiologist to be faced with a PE increases. Echocardiographic finding of the PE is still the key element for diagnostic of a PE. This article will display a technique for a safe and controlled puncture of a PE/tamponade.
In this article the angiographic guided pericardial puncture should be described with no preference for the angiographic guided puncture in comparison to the echocardiographic guided puncture.
The problem
The pericardium is a double-layer strong fibrous structure covering the heart and containing a physiological fluid volume of approximately 50ml. Accumulation of additional fluids in the pericardial space leads to a compression of the heart. Patients often present with sinus tachycardia, elevated jugular venous pressure and low blood pressure in a critical hemodynamic situation. This pericardial tamponade is a life-threatening situation, which can be diagnosed anywhere. This problem of the tamponade needs to be identified and a puncture of the tamponade needs to be performed without delay. Therefore, a technique to handle this situation should exist.
Principal idea
Puncture and drainage of pericardial fluid can be performed for hemodynamic and diagnostic reasons. Seldinger's technique to access the pericardial space and insert a 6 French sheath over a standard J-guidewire to reassure the position in the pericardial space is of routine use. Inserting a 5 French pigtail catheter offers a possibility to remove pericardial fluid without losing access to the pericardium. The strategy described here is simple and puncture techniques are known, thus this technique should be easy to adapt.
Material needed
Description is for pericardial puncture in the cath lab (or situation with available x-ray machine) under sterile conditions with ECG monitoring.
- Local anaesthesia with needle
- puncture needle for 0.035 wire
- syringe (10 or 20 ml)
- 0.035 J-guidewire
- 6 French sheath
- 5 French pigtail
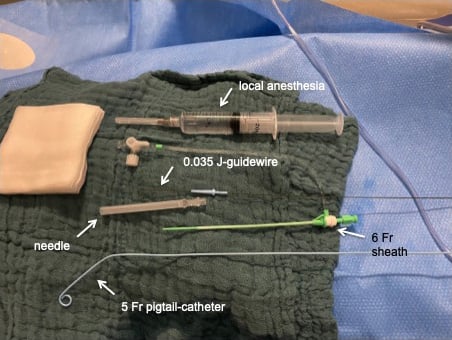
Material needed
Method step-by-step
Step by step approach for a subxiphoid pericardial puncture. This puncture should be performed under fluoroscopy guidance.
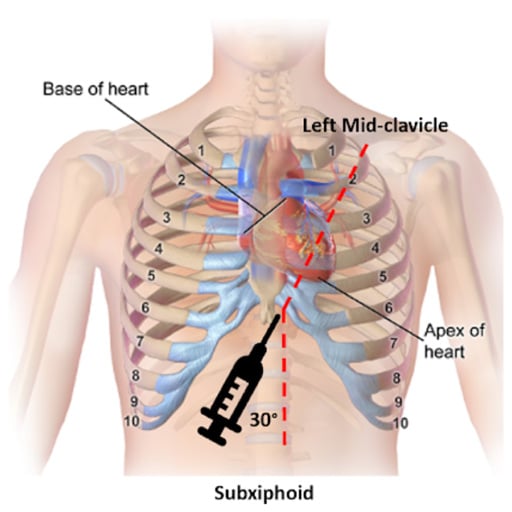
Subxiphoidal puncture. Image Courtesy of David Feiger - Northwestern Memorial Hospital, Chicago, USA
1 - Local anaesthesia
Local anaesthesia must be given slightly left subxiphoidal where puncture should be performed.
2 - Needle puncture
Needle puncture with continuous aspiration at a flat angle (approximately 30°) to the skin pointing in the direction of the transition of the clavicula and left shoulder (humeral head). If no fluid can be aspirated, retractation of the needle is necessary and another puncture with an increased angle to the skin of about 45-60° should be performed.
3 - Wire introduction
After aspiration of fluid, the syringe should be removed and the J-wireshould be deeply introduced with no insertion against any resistance.
Check three checkpoints for correct position of the needle and wire in the pericardial space:
- Analyse colour of fluid:
- light amber-coloured serous fluid – probably pericardial effusion (alternatively pleural effusion)
- bloody coloured fluid – do a blood gas analysis and check haemoglobin value (compare with haemoglobin in blood check), lactate, saturation of O2 (pO2) and CO2 (pCO2)
- Fluoroscopy in straight anterior-posterior projection will help to identify wire enhancement and position – big curve around the heart is anatomically correct and probably in pericardial space
- Check ECG monitoring for extra beats during wire protrusion – if no extra beats (ventricular or atrial) occur, pericardial position should be correct (when extra beats occur in ECG monitoring, probably ventricular puncture)
4 - Access sheath
Remove needle and emerge to the 6 French sheath. Keep the J-wire inserted.
5 - Pigtail insertion
Insert 5 French pigtail-catheter over the J-wire and check position under fluoroscopy again.
6 - Aspirate pericardial effusion
Start to aspirate pericardial effusion and check continuously blood pressure. After release of approximately 300ml fluid, check by echocardiography the reduction of the pericardial effusion.
7 - Sewing access sheath and bandage
Points of specific attention
- The correct position of the needle after the puncture is key in this process. See the three key checkpoints. If there is any doubt do not continue with the 6 French sheath. Retracting the needle and/or the J-wire will mostly not cause any problems even when punctured the left or right ventricle.
- Make sure the pigtail catheter is at least one French smaller than the access sheath. In case of acute bloody tamponade, blood might clot over time. By using the access sheath, small volume of saline can be infused to dilute the clotted blood and this mixture can be aspirated.





6 comments
Ultrasound guidance is a must for a safe PE puncture. Bubble test may be used to ensure the correct location especially if there is also pleural effusion and the apical approach is used. I personally use the apical approach for non-iathrogenic effusion such as cancer-induced. Emergency puncture is usually better be done via the subxiphoidal approach using at least 7F pigtal to ensure getting even clotted blood aspirated.
Micropuncture technique is also safer with 0.018 wire. If Echo is not available, and there is doubt about the position of the needle, injection of a small amount of contrast can verify pericardial space vs intracardiac position.
A decisive detail for a successful pericardial puncture was not mentioned by the T. Schmidt: the lateral (90 degree) view during flouroscopy when approaching the pericardial sac with the puncturing needle. It shows the pericardial "halo phenomenon", which depicts the epicardial border. This phenomenon has been described in detail by Maisch B, Ristic A, Seferovic P, Tsang T, Interventional Pericardiology, Springer (Heidelberg), 2011, p. 44.
fluoroscopy guided puncture is unsafe, outdated and should only be performed when no ultrasound is available. To check blood gas hb is meaningless in a tamponade caused by bleeding. A 5 F pigtail is too small for hemopericard. Every cathlab should aim to perform ultrasound guided pericardiocentesis with needle guidance and microbubble contrast.
What is the advantage of using an access sheath? Is it necessary?
Echo guided aspiration is good . To conform sac or chamber do small amount contrast injection .