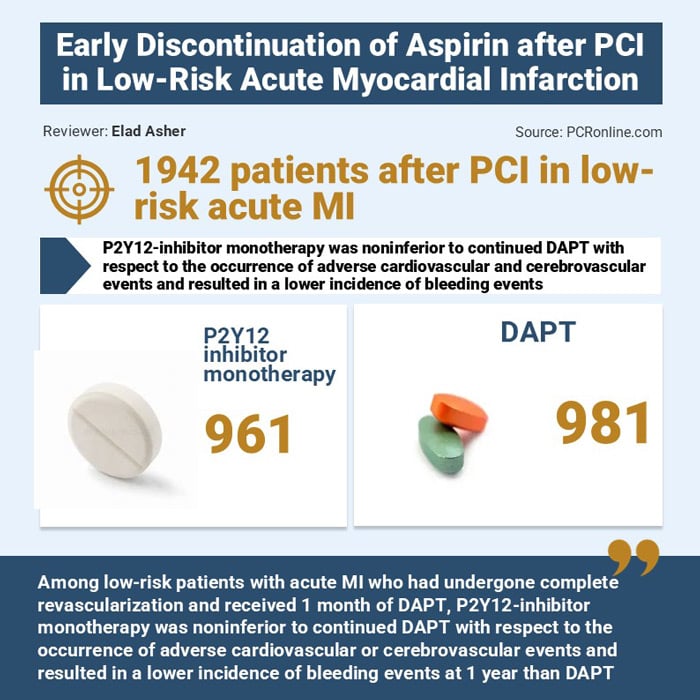
TARGET-FIRST: Early aspirin discontinuation after PCI in low-risk acute MI patients
Reported from ESC Congress 2025
Elad Asher provides his take on the results of TARGET-FIRST presented by Giuseppe Tarantini at the ESC Congress 2025 in Madrid.
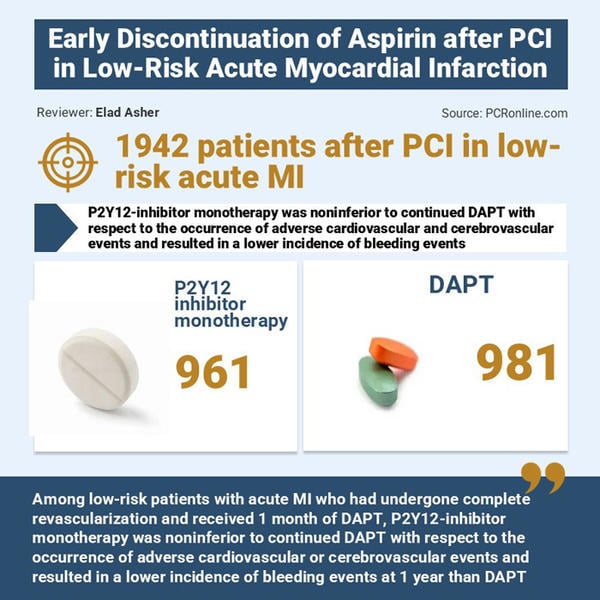
Source: PCRonline.com
Why this study – the rationale/objective?
Aspirin has been a cornerstone of dual antiplatelet therapy (DAPT) following percutaneous coronary intervention (PCI). The conventional standard is 12 months of DAPT (aspirin plus a P2Y12 inhibitor) in patients with acute coronary syndromes (ACS), including myocardial infarction (MI). However, prolonged use of aspirin is associated with a significant increase in bleeding risk, which can offset the ischemic protection provided.
Over the last decade, several randomized controlled trials have questioned the need for prolonged aspirin therapy after PCI, suggesting that early discontinuation of aspirin, while maintaining potent P2Y12 inhibitor therapy, might reduce bleeding complications without increasing ischemic events.
The rationale for this study was therefore to determine:
- Is early discontinuation of aspirin after PCI safe and effective in patients with low-risk acute MI?
- Could P2Y12 inhibitor monotherapy provide sufficient ischemic protection while lowering bleeding risk?
The study aimed to generate high-quality evidence to guide the evolving debate between ischemic protection versus bleeding minimization, and whether international guidelines should reconsider the necessity of prolonged aspirin use in this patient group.
How was it executed – the methodology?
- Design: Multicenter, randomized controlled trial.
- Population: Patients with low-risk acute myocardial infarction (as defined by angiographic and clinical criteria) undergoing PCI with drug-eluting stents.
- Intervention groups:
- Standard therapy (control): 12 months of DAPT (aspirin + P2Y12 inhibitor).
- Experimental arm: Early aspirin discontinuation (after at least 30 days of DAPT) followed by P2Y12 inhibitor monotherapy.
- Endpoints:
- Primary endpoint: Composite of major adverse cardiovascular events (MACE), including cardiovascular death, MI, stroke, and stent thrombosis.
- Secondary endpoint: Bleeding events (according to BARC classification), all-cause mortality, and net adverse clinical events (NACE).
- Follow-up duration: 12–24 months.
- Statistical analysis: Non-inferiority design with intention-to-treat analysis. Hazard ratios and Kaplan–Meier survival estimates were used to compare outcomes.
Results – Major findings
- Efficacy (Ischemic outcomes):
- Rates of MACE were non-inferior between the aspirin-discontinuation group and the standard DAPT group.
- No significant increase in stent thrombosis or recurrent MI was observed after aspirin discontinuation.
- Safety (Bleeding outcomes):
- Bleeding rates were significantly lower in the aspirin-discontinuation group.
- Clinically relevant non-major bleeding and major bleeding events both decreased when aspirin was withdrawn.
- Net Clinical Benefit:
- The strategy of early aspirin withdrawal demonstrated a favorable net clinical outcome, balancing ischemic safety with bleeding reduction.
In short, P2Y12 inhibitor monotherapy after early aspirin discontinuation proved safe and effective, with clear reductions in bleeding complications without compromising ischemic protection.
Critical reading and relevance for clinical practice
This study adds to a growing body of evidence supporting aspirin-free strategies post-PCI.
However, some limitations must be noted:
- The trial population was low-risk, limiting generalizability to higher-risk ACS or complex PCI cases.
- Relatively short follow-up may miss very late ischemic events.
- The findings apply primarily to settings where potent P2Y12 inhibitors (ticagrelor, prasugrel) are available and affordable.
Clinical relevance
- The results strongly suggest that for carefully selected low-risk MI patients, prolonged aspirin therapy after PCI may no longer be necessary.
- Reducing aspirin exposure decreases bleeding risk, which is particularly relevant in elderly patients and those with comorbidities such as renal disease or prior gastrointestinal bleeding.
- This evidence may shift clinical practice toward P2Y12 inhibitor monotherapy after PCI, at least in selected populations.
Should common practice and guidelines be changed?
Current ESC and ACC/AHA guidelines still recommend 12 months of DAPT after ACS/PCI, though recent updates acknowledge that shorter durations may be reasonable in patients with high bleeding risk.
In your opinion, should current guidelines be updated? Would you consider discontinuing aspirin after one month of DAPT in patients with low-risk myocardial infarction?
Latest news from ESC Congress 2025




No comments yet!