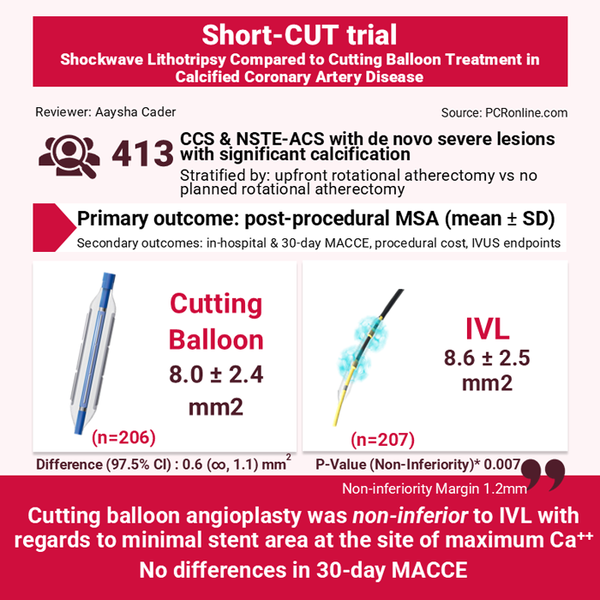
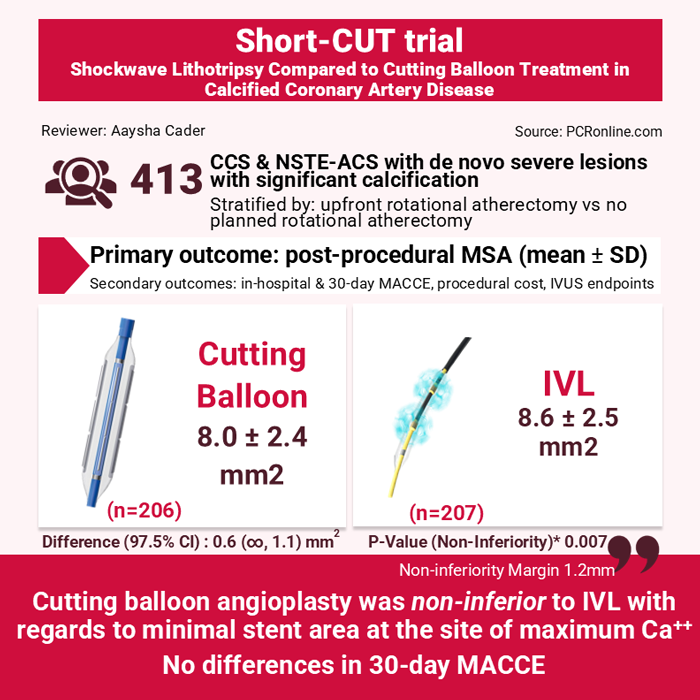
Randomised comparison of intravascular lithotripsy vs. cutting balloon treatment in calcified coronary artery disease – The Short-CUT trial
Reported from TCT 2025
Aaysha Cader provides her take on the Short-CUT trial presented by Suzanne J. Baron at TCT 2025, in San Francisco.
Designed by: Aaysha Cader
Source: PCRonline.com
Why this study – the rationale/objective?
Significant coronary lesion calcification is associated with increased procedural complexity and poorer post-PCI outcomes. Intravascular lithotripsy (IVL) is widely used because of its ease of use, with minimal learning curve, but there are no randomised head-to-head comparisons of safety and efficacy of IVL with other balloon-based devices.
The Short-CUT trial aimed to evaluate the safety, efficacy and procedural cost of cutting balloon angioplasty compared with IVL in PCI for patients with moderate-to-severe calcification1,2.
Methodology
This was an investigator-initiated, multicentre, randomised controlled trial designed to demonstrate non-inferiority between cutting balloon angioplasty and IVL prior to drug-eluting stent (DES) implantation in significantly calcified coronary artery disease (CAD) undergoing IVUS-guided PCI2.
Patients were stratified into 2 cohorts:
- Those treated with up-front rotational atherectomy; randomisation occurred after successful atherectomy (hence, “rota-cut” or “rota-shock”)
- Those with no planned rotational atherectomy; randomisation occurred after successful wire passing
In each of these cohorts, patients were randomised 1:1 to either cutting balloon angioplasty [Device sized 0.5 mm smaller than reference vessel diameter, high-pressure inflation (e.g. 16-20 atm) or IVL [device sized 1:1 to reference vessel diameter, number of pulses at operator discretion].
Inclusion criteria:
- Presentation with stable angina or down-trending biomarker NSTE-ACS with de novo native lesion > 70 % or 50-70 % with evidence of hemodynamic significance were included.
- Significant calcification was defined either as:
- Radio-opacities involving both sides of arterial wall > 5 mm at lesion site
- > 270o arc of Ca++ > 5 mm length on HD-IVUS
- 360o arc of Ca++ on HD-IVUS
Exclusion criteria:
STEMI within 30 days, LVEF < 25 %, cardiogenic shock or anticipated mechanical/pharmacological support, excessive tortuosity or anatomic considerations precluding intravascular imaging, and target vessel dissection.
Endpoints:
The primary endpoint was post-procedural minimal stent area (MSA) as measured by IVUS at the site of maximal calcification.
Key secondary endpoints:
Procedural cost, strategy success, in-hospital and 30-day MACCE and IVUS endpoints: stent expansion, calcium fractures, significant residual stenosis (any stent area < 4.5 mm2).
Design:
Non-inferiority design with reflex superiority testing of primary endpoint: at an assumed mean MSA 6.5 mm2 with SD 2.5 mm2 and non-inferiority margin of 1.2 mm2, 412 patients (206 in each arm) provides 90 % power to detect non-inferiority.
What is the main result?
A total of 413 patients were randomised across 21 sites in the United States, stratified by cohort as n = 208 in upfront rotational atherectomy group, and n = 205 in no planned rotational atherectomy group.
Across these cohorts, 207 were randomised to IVL and 206 to cutting balloons. Mean age was ~72 years, and ~75 % were men. Target lesion stenosis was 87.4 ± 9.8 vs 88.8 ± 8.9 %, and reference vessel diameter was 3.5 ± 0.5 vs 3.5 ± 0.5 mm for IVL vs CB respectively. ~25 % were nodular calcium.
The primary endpoint, mean post-procedural MSA was 8.6 ± 2.5 mm2 in the IVL group and 8.0 ± 2.4 mm2 in the cutting balloon group, with a difference of 0.6 mm2. The upper bound of the confidence interval (1.1 mm2) was within 1.2 mm2 non-inferiority margin, hence establishing non-inferiority of cutting balloons (P = 0.007). Superiority testing indicated no significant difference between groups.
There were no differences in key core-lab derived IVUS endpoints of stent expansion at site of maximum Ca++ (%), minimum stent expansion (%), evidence of and number of calcium fractures.
There were no between-group differences of key secondary endpoints of device-related complications, intraprocedural adverse events, strategy success, in-hospital or 30-day MACCE.
However, there was a significant difference in total procedural cost difference of $3,632 in favour of cutting balloons (p < 0.001).
Upon analysis of primary endpoint stratified by atherectomy plan, an interaction was observed, wherein the non-inferiority of cutting balloons was seen in patients with planned atherectomy but not in those without planned atherectomy; however, further analyses indicated that this discrepancy could be related to slightly smaller reference vessels among patients treated with cutting balloons, given that stent expansion and fracture indices were similar between groups.
Critical reading and the relevance for clinical practice
Short-CUT certainly adds to the literature on balloon-based strategies that can be safely and effectively used to treat moderate to severe calcified lesions, particularly given reduced cost implications of cutting balloons as compared to IVL.
The VICTORY trial, also presented at TCT, showed non-inferiority of OPN balloons compared to IVL in terms of post-PCI MSA as assessed by OCT3. As compared to OPN and OCT, cutting balloons and IVUS are more widely available, providing lower cost, safe alternatives and greater applicability as an initial strategy for balloon-crossable lesions, given availability across different cathlab settings.
The analyses of RA vs non-RA cohorts in this trial is important, with results indicating no difference between a rota-cut vs rota-shock plan among patients undergoing atherectomy. However, in those that did not undergo atherectomy, the fact that cutting balloons angioplasty did not meet non-inferiority could imply that when atherectomy is not used, cutting balloons alone likely do not suffice, and there might still be a need for further calcium modification strategies.
Finally, the trial was not powered for clinical or long-term outcomes nor are there plans for angiographic follow-up. Although post-PCI MSA is a reliable surrogate for longer-term clinical outcomes, the lack of long term follow-up in this trial means that we won’t know if any differences in late lumen loss or longer-term clinical outcomes could emerge between groups.
References
- https://www.clinicaltrials.gov/study/NCT06089135
- https://www.tctmd.com/slide/short-cut-randomized-trial-cracking-calcium-code
- A randomised, multicenter, non-inferiority comparison of intravascular lithotripsy and super-high-pressure non-compliant balloons for treatment of calcified and refractory coronary lesions - The VICTORY trial




No comments yet!