Mid-term echocardiographic outcomes following transapical mitral valve replacement: Updates from the Intrepid Pilot Study
Reported from TCT 2022
Pamela Gatto provides her take on the Intrepid Global Pilot Study which was presented by Renuka Jain at TCT Congress 2022.
Mitral regurgitation (MR) is a common valvular heart disease. Surgical mitral valve repair/replacement has been associated with good clinical outcomes in patients with severe MR. However, a high percentage of patients suffering from this condition are still rejected from surgery because of their comorbidities and high or extreme surgical risk.
Several catheter-based therapies have emerged over the past decades. Particularly, the transcatheter edge-to-edge mitral valve repair (TEER) technique is currently supported by growing evidence. However, TEER is prone to some limitations in applicability related to the anatomical substrate (e.g., leaflet thickening and calcification, short posterior mitral leaflet with limited motion). There is also a limited capability to fully correct the severity of the regurgitation and prevent MR progression over time [1,2]. Transcatheter mitral valve replacement (TMVR) has emerged as a less invasive approach than standard surgery, which could overcome some of the current limitations associated with TEER.
The Intrepid Global Pilot Study [3] is a prospective, multi-center, non-randomized study. It assesses the feasibility of treating MR with the Intrepid Transcatheter Mitral Valve Replacement (TMVR) Transapical System in patients at high risk for surgical MVR. It evaluates clinical outcomes and echocardiographic findings.
In the paper published in 2018, the authors reported their early experience. The valve investigated was implanted using a transapical delivery system; the population was characterised by patients suffering from symptomatic MR, at high or extreme surgical risk, according to the evaluation of the local heart teams.
In the study, fifty consecutively enrolled patients (mean age: 73 ± 9 years; 58.0% men; 84% secondary MR) underwent TMVR. The mean Society for Thoracic Surgery score was 6.4 ± 5.5%; 86% of patients were New York Heart Association functional class III or IV, and the mean left ventricular ejection fraction was 43 ± 12%. Device implant was successful in 48 patients with a median deployment time of 14 min (interquartile range: 12 to 17 min). The 30-day mortality was 14%, with no disabling strokes, or repeat interventions. Median follow-up was 173 days (interquartile range: 54 to 342 days). At latest follow-up, echocardiography confirmed mild or no residual MR in all patients who received implants. Improvements in symptom class (79% in New York Heart Association functional class I or II at follow-up; p < 0.0001 vs. baseline) and Minnesota Heart Failure Questionnaire scores (56.2 ± 26.8 vs. 31.7 ± 22.1; p = 0.011) were observed.
The investigators concluded that TMVR was feasible in a study group at high or extreme risk for conventional mitral valve replacement. Stable valve function was observed longitudinally, and most patients experienced significant improvement in their clinical symptoms and functional class. [3]
At TCT 2022, Renuka Jain presented for the Global Pilot Study Investigators, the mid-term echocardiographic outcomes following transapical mitral valve replacement.
The author summarised echocardiographic outcomes for subjects up to 3-years of follow-up.
The 95 consecutively enrolled patients in the Global Pilot Study, of whom 42 had 3 year ± 6 months echo available for paired data. The transapical delivery system was used for valve delivery in all 95 patients. All echocardiographic data were examined in an independent core laboratory (University of California, San Francisco, California). Grading of valvular and paravalvular MR was performed using standard criteria [4].
At baseline, the median age of the 42 patients with paired echo data was 74.5 years (interquartile range [IQR]: 66.0, 81.0). The majority (59.5%) were men, most (88.1%) were in New York Heart Association functional class III or IV, median Society of Thoracic Surgeons Predicted Risk of Mortality was 4.8% (IQR: 3.2%, 6.1%), and median EuroSCORE II was 5.1% (median: 3.3%, 9.1%). A plurality (47.6%) had one or more sternotomies, 40.5% had prior percutaneous coronary intervention, 35.7% had prior coronary artery bypass grafting, and 35.7% had diabetes. Most had secondary MR (66.7%), and the median left ventricular ejection fraction was 43.0% (IQR: 34.0%, 55.0%).
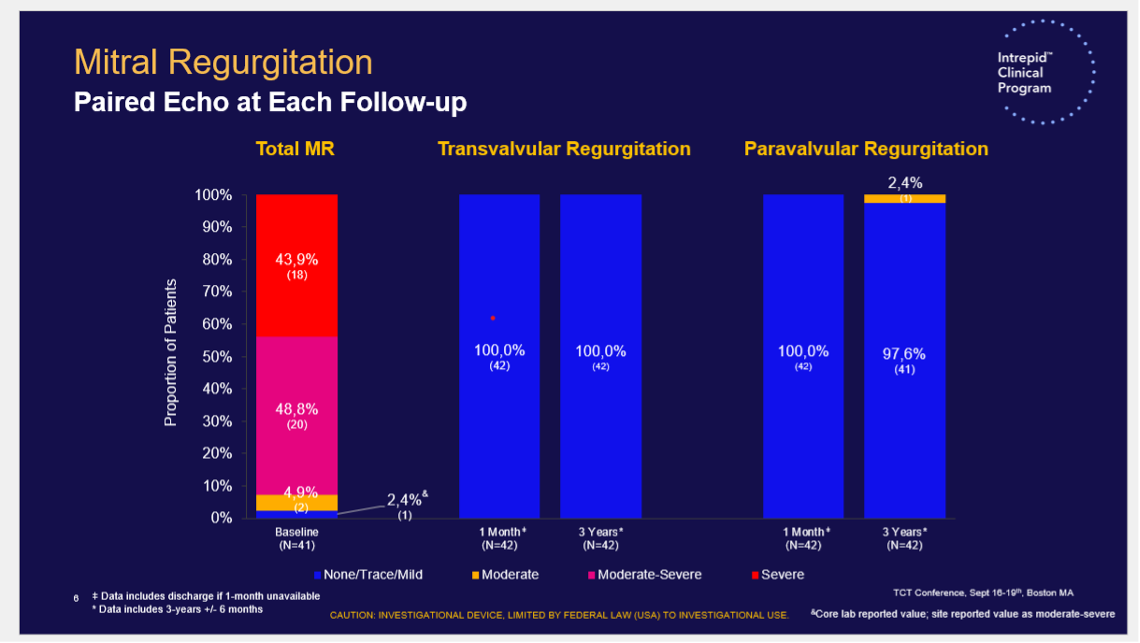
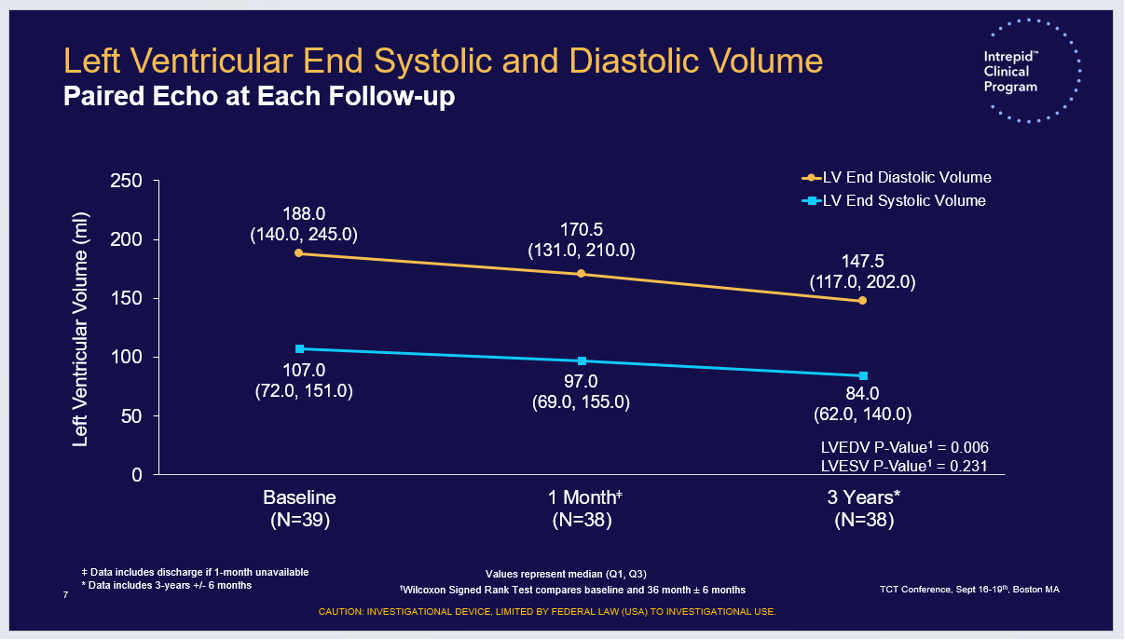
The author announced the Echocardiographic outcomes in 3-year survivors. They showed a stable valve function with low mean MV gradients at 3 years, a persistent MR reduction with only one patient with ≥ moderate PVL and a significant reduction in LV end diastolic volume from baseline.
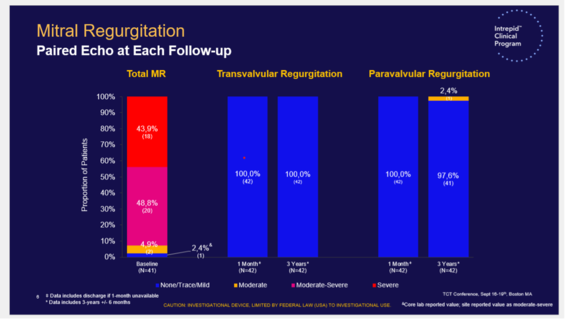
Mitral regurgitation - Paired echo at each follow-up. Source: TCT 2022
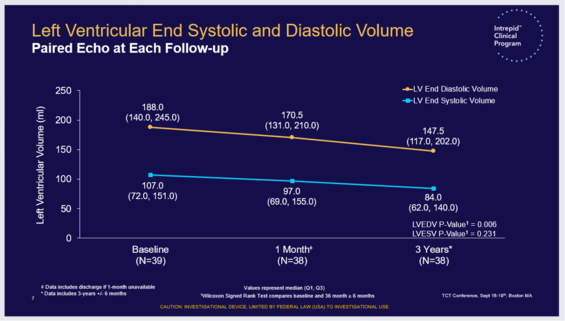
Left ventricular end systolic and diastolic volume - Paired echo at each follow-up. Source: TCT 2022
In conclusion, the Global Pilot Study currently has the longest follow-up from the largest series of high surgical risk patients with severe MR treated with a transapical TMVR system. The evidence is encouraging and reinforces the role of this therapeutic option.
References
- R.A. Nishimura, A. Vahanian, M.F. Eleid, M.J. Mack, Mitral valve disease - Current management and future challenges, Lancet, 387 (2016), pp. 1324-1334
- M. Chiarito, M. Pagnesi, E.A. Martino, et al. Outcome after percutaneous edge-to-edge mitral repair for functional and degenerative mitral regurgitation: a systematic review and meta-analysis Heart, 104 (2018), pp. 306-312
- Bapat et al. Early Experience With New Transcatheter Mitral Valve Replacement, J Am Coll Cardiol 2018; 71(1): 12-21;
- Zoghbi WA et al. J Am Soc Echocardiogr. 2009;22:975-1014





No comments yet!