19 Sep 2022
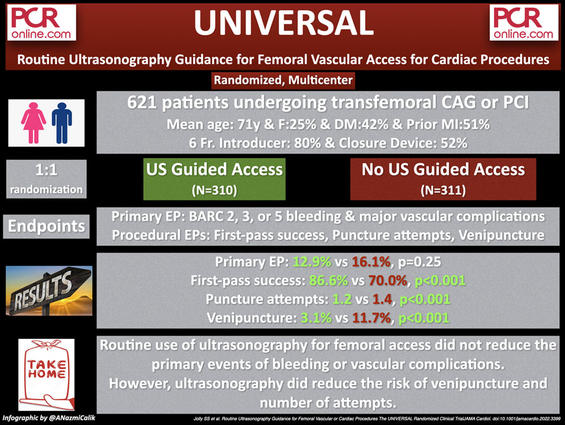
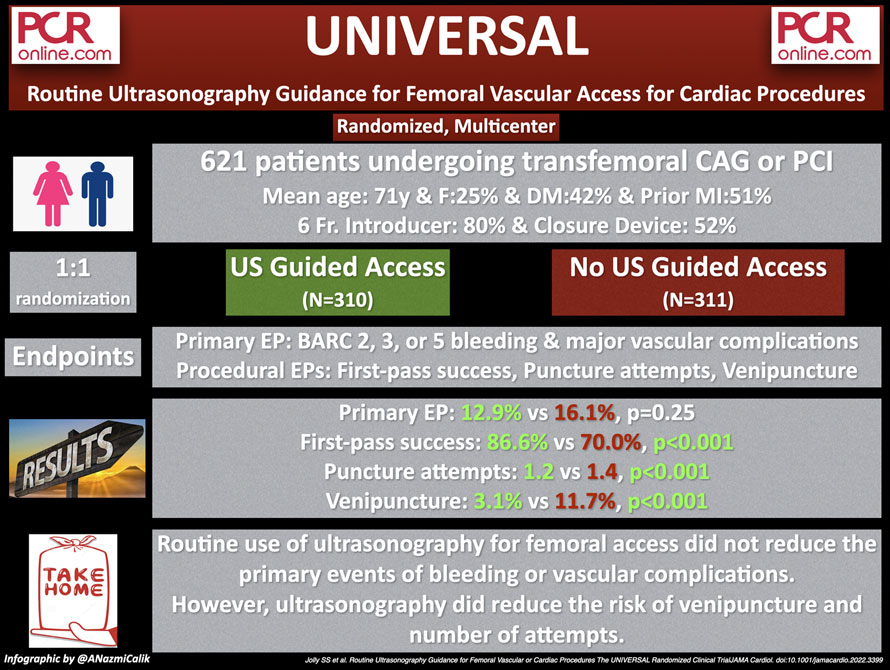
UNIVERSAL: routine ultrasonography guidance for femoral vascular access for cardiac procedures - A randomized clinical Trial
Reported from TCT 2022
Ali Nazmi Calik provides his take on UNIVERSAL randomized clinical trial, which questioned whether routine ultrasonography guidance for CFA access for cardiac procedures reduces bleeding or vascular complications. This trial was presented by Sanjit S. Jolly during TCT 2022.
Courtesy of Ali Nazmi Calik @ANazmiCalik. Source: PCRonline.com
Why this study? – the rationale/objective
Despite the reduced bleeding rates and major vascular complications with transradial access, femoral access is still used for large bore procedures, or when the radial arteries are not suitable for access because of insufficient dimensions or occlusion.
Common femoral artery (CFA), with its superficial course atop the femoral head, may be the most straightforward anatomical access side to the arterial system. However, running lateral to the femoral vein and its short course between the femoral bifurcation and the inferior epigastric artery make it prone to access site complications.
As the anatomical landmarks, such as femoral bifurcation and inguinal ligament, are not visible under fluoroscopy, an inadvertently lower (under femoral bifurcation) puncture may easily lead to pseudoaneurysm, arteriovenous fistula, and hematoma, whereas a puncture above the inguinal ligament may end up with a retroperitoneal hematoma. These CFA access-related vascular complications are not uncommon and are closely associated with extended hospital stays or a need for further procedures1.
Without a doubt, all efforts should be made to perform safe femoral access. Ultrasonography-guided CFA access is a cost-effective method to perform #safefemoral with the ability to provide visualization of key anatomical landmarks such as CFA bifurcation, inguinal ligament, and femoral vein. As for the interventions where large bore access is needed, it allows the interventionalists to puncture the CFA's nondiseased and noncalcified region safely, thus facilitating the use of a closure device. Although ultrasonography is available at almost nine out of ten catheterization laboratories, according to a survey conducted in the US, only 26 % of interventionalists use it routinely for CFA puncture2.
The routine ultrasound guidance for vascular access for cardiac procedures (UNIVERSAL) randomized clinical trial questioned whether routine ultrasonography guidance for CFA access for cardiac procedures reduces bleeding or vascular complications.
How was it executed? - the methodology
The UNIVERSAL trial is a multicenter randomized clinical trial of ultrasonography-guided approach vs no ultrasonography for femoral access for cardiac procedures in the background of fluoroscopic landmarking. The trial is an open-label trial with a blinded assessment of outcomes.
ST segment elevation MI presentation, being younger than 18 years old, and absence of a palpable femoral pulse were defined as the exclusion criteria. Patients undergoing coronary angiography (CAG) or percutaneous coronary intervention (PCI) with planned femoral access were included in the study. Since many patients’ CAG or PCI at the participant centres were performed by transradial access, the randomized patients were not consecutive.
In the ultrasonography group, operators were required to have completed at least ten observed ultrasonography-guided femoral access and demonstrate proficiency, including identifying the crucial anatomical landmarks and confirming the wire entry in orthogonal views on ultrasonography. Identifying the femoral head with fluoroscopy was recommended for both groups prior to the puncture of the artery.
The primary outcome was the composite of Bleeding Academic Research Consortium (BARC) 2, 3, and 5 bleeding or major vascular complications (femoral artery pseudoaneurysm, arteriovenous fistula, retroperitoneal bleed, large hematoma of more than 5 cm in diameter, or ischemic limb requiring intervention or surgery) within 30 days. The key secondary outcome was BARC 2, 3, or 5 major bleeding.
Besides the components of the primary outcome, including major vascular complications, the number of attempts for arterial puncture, successful common femoral artery cannulation, venipunctures, closure device failure, and the total time to obtain femoral access were defined as the other outcomes.
Successful cannulation of CFA was defined as at or above femoral bifurcation and below inferior epigastric artery by core laboratory reviewers.
What is the main result?
A total of 621 patients (310, ultrasonography vs 311 no-ultrasonography) were randomized at two centres. The patients had a mean age of 71 years, and 158 (25.4 %) were female. Half of the trial population (51 %) had prior MI, 261 (42 %) had diabetes, 353 (57 %) had previous coronary bypass surgery, and 110 (18 %) had peripheral vascular disease. 509 patients (80 %) received 6 Fr. introducer, 262 (42 %) of the procedures were PCI, and closure devices were used in 331 (52.1 %) patients.
The ultrasonography-guided access did not significantly reduce the risk of the primary outcome, a composite of BARC grade 2, 3, or 5 bleeding at 30 days and major periprocedural vascular complications (12.9 % vs 16.1 %; odds ratio, 0.77; 95 % CI, 0.49-1.20, p = 0.25). Further, the rates of BARC grade 2, 3, or 5 bleeding (10.0 % vs 10.7 %, p = 0.78) and major vascular complications (6.4 % vs 9.4 %, p = 0.18) were not significantly different between two groups.
In a prespecified, nonrandomized subset of patients treated with a vascular closure device placed via operator discretion, ultrasonography guidance was associated with a reduction in risk of the primary outcome (11.8 % vs 23.4 %; odds ratio, 0.44; 95 % CI, 0.23-0.82, p = 0.004).
As for the procedural outcomes, ultrasonography-guided approach improved first-pass success (86.6 % vs 70.0 %, p < 0.001), reduced the number of arterial puncture attempts (mean 1.2 vs 1.4, p < 0.001), and venipuncture (3.1 % vs 11.7 %, p < 0.001).
Critical reading and the relevance for clinical practice
In summary, the UNIVERSAL study showed that routine ultrasonographic guidance for CFA access did not reduce major vascular complications and major bleeding, but improved first-pass success, reduced the number of puncture attempts, and the incidence of accidental venipuncture, without a significant delay in obtaining femoral artery access.
Further, in a subgroup analysis of patients receiving vascular closure devices, the ultrasonography-guided approach reduced the incidence of the primary outcome and improved safety.
Of note, an updated meta-analysis of nine randomized controlled studies, including the present study, showed significantly reduced rates of major vascular access complications and bleeding with ultrasonography guidance.
Therefore, before interpreting the results of this trial as neutral, it is crucial to bear in mind the following considerations and limitations:
- The micropuncture technique was not used, which could have affected the incidence of complications.
- The composite primary outcome, including the assessment of BARC 2,3 and 5 bleeding, which was primarily driven by BARC 2 bleeding, at 30 days, might have been influenced by non-access related bleeding events. Thus, an adequately powered study for investigating vascular access complications could have potentially found a significant difference between ultrasound guidance in the background of fluoroscopy and fluoroscopic guidance only.
- Ultrasonography does not appear to have any risks, facilitates access, is widely available, and has a short learning curve.
To conclude, the transradial (#radialfirst) approach should be the choice of access for any procedure when feasible. Otherwise, one should put a solid effort into performing #safefemoral access with ultrasonography to preclude access site and bleeding complications.
References
- Dehmer GJ, Weaver D, Roe MT, et al. A contemporary view of diagnostic cardiac catheterization and percutaneous coronary intervention in the United States: a report from the CathPCI Registry of the National Cardiovascular Data Registry, 2010 through June 2011. J Am Coll Cardiol. 2012;60(20):2017-2031. doi:10.1016/j.jacc.2012.08.966
- Damluji AA, Nelson DW, Valgimigli M, et al. Transfemoral approach for coronary angiography and intervention: a collaboration of international cardiovascular societies. JACC Cardiovasc Interv. 2017;10(22):2269-2279. doi:10.1016/j.jcin.2017.08.035




1 comment
micropuncture technique would affect both modalities, so unclear as to how it will affect the results.