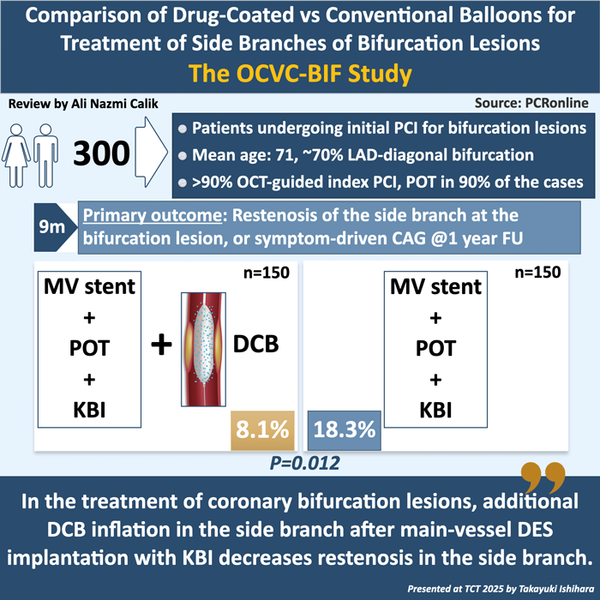
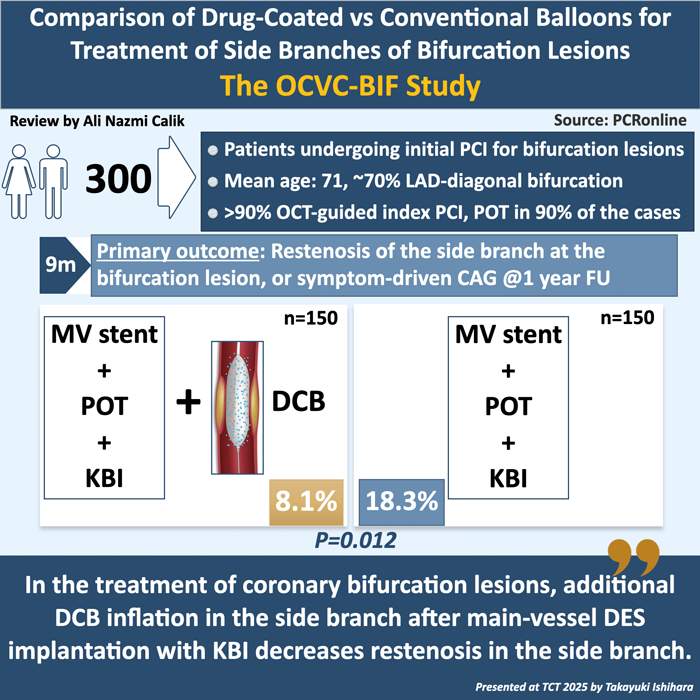
Comparison of drug-coated versus conventional balloons for treatment of side branches of bifurcation lesions: the OCVC-BIF study
Reported from TCT 2025
Ali Nazmi Calik provides his take on the OCVC-BIF study presented by Takayuki Ishihara at TCT 2025, in San Francisco.
Designed by: Ali Nazmi Calik
Source: PCRonline.com
Why this study – The rationale / objective
Coronary bifurcation lesions remain a technical challenge in percutaneous coronary intervention (PCI). Despite the evolution of modern drug-eluting stents (DES), proximal optimisation technique (POT), and kissing-balloon inflation (KBI), the side branch (SB) often remains a site of restenosis.
The rationale for the OCVC-BIF trial was to test whether adjunctive use of a drug-coated balloon (DCB) in the side branch—following main-branch DES implantation and KBI—could deliver antiproliferative therapy without additional stent implantation, thereby improving side-branch patency and outcomes compared with a non-DCB strategy.
How was it executed – The methodology
The OCVC-BIF trial was a multicentre, randomised, open-label study conducted at several high-volume centres within the Osaka Cardiovascular Conference (OCVC) network among patients undergoing initial PCI for a bifurcation lesion.
Patients were eligible if they had a bifurcation lesion involving a side branch with a diameter ≥ 2.0 mm and < 3.0 mm, were suitable for main-branch DES implantation, and had no exclusion criteria such as in-stent restenosis (ISR), bypass graft lesions, hemodialysis, or a recent acute myocardial infarction (MI).
After main-vessel stenting and KBI (and POT when applicable), patients were randomised to:
- DCB arm: side-branch inflation using a paclitaxel-coated balloon (DCB) after adequate lesion preparation.
- Control arm: no DCB use in the side branch (main-vessel stenting and KBI alone).
The primary endpoint was restenosis of the side branch at 9 months or symptom-driven angiography within 1 year. Restenosis was defined as ≥ 50 % diameter stenosis of the side branch, assessed by three-dimensional quantitative coronary angiography (3D-QCA).
Secondary endpoints included the rate of clinically driven target lesion revascularisation (CD-TLR) in the side branch at 12 months after PCI, procedural success rate, incidence of PCI-related complications, and the rate of major adverse cardiac events (MACE) at 12 months, as well as each individual component endpoint. MACE was defined as a composite of cardiac death, MI, CD-TLR, and stent thrombosis (ST).
Independent core-lab 3D-QCA was used for angiographic analysis. Intravascular imaging with optical coherence tomography (OCT) or intravascular ultrasound (IVUS) was encouraged but not mandated. Almost all procedures were performed under intravascular imaging guidance, predominantly using OCT (follow-up OCT evaluation is also performed for the patients who underwent OCT-guided PCI). Approximately 70 % of all bifurcation lesions in the study were located in the left anterior descending (LAD) artery–diagonal branch. POT was applied in approximately 90 % of procedures in both groups. Bailout DES implantation for the side branch was required in only three patients in the DCB group and one patient in the non-DCB group.
What is the main result?
In the OCVC-BIF study, the principal finding was a statistically significant reduction in angiographic side-branch restenosis at 9 months in the DCB arm compared with the control group. The DCB group demonstrated a restenosis rate of 8.1 % versus 18.3 % in the non-DCB group (P = 0.012; odds ratio [OR] ≈ 0.36). Quantitative coronary angiography analysis further showed a smaller mean diameter stenosis in the side branch (32.5 % vs 36.2 %; P = 0.03) and a greater minimal lumen diameter (1.45 mm vs 1.32 mm; P = 0.02) in the DCB arm. Late lumen loss in the main branch was also smaller in the DCB group (0.21 mm vs 0.36 mm; P = 0.037).
Regarding clinical outcomes, at 1 year, the rate of CD-TLR was 0.7 % vs 3.4 % (P = 0.20), and the incidence of MACE was 10.1 % vs 12.4 % (P = 0.65) in the DCB and control arms, respectively.
Critical reading and relevance for clinical practice
Integrating DCB therapy into bifurcation PCI reflects a contemporary, metal-sparing approach that may help mitigate long-term complications associated with additional stent layers, such as late stent thrombosis and neointimal proliferation. The OCVC-BIF study represents a well-designed, randomised investigation evaluating the role of DCBs for side-branch treatment in coronary bifurcation lesions. Its core-laboratory–adjudicated angiographic endpoints, real-world population, and focus on the provisional stenting strategy strengthen the validity and clinical applicability of its findings. The selection of side-branch restenosis as the primary endpoint is particularly relevant, as it closely correlates with the risk of future revascularisation. Furthermore, the use of intravascular imaging in nearly all procedures enhanced procedural optimisation and ensured high-quality lesion assessment and treatment precision.
However, several limitations temper the interpretation of these findings. The one-year follow-up was relatively short, leaving the durability of angiographic improvement uncertain, and the trial may have been underpowered to detect differences in hard clinical outcomes such as death, spontaneous MI, or TLR. Only paclitaxel-coated balloons were used, so the applicability of newer sirolimus-based technologies remains untested. The study population consisted mostly of relatively simple bifurcation lesions suitable for a single-stent strategy, limiting generalisability to more complex anatomies. While the angiographic benefit was evident, it did not translate into a statistically significant reduction in clinical events.
When considered alongside the larger DCB-BIF trial1 presented at TCT 2024, the results of OCVC-BIF gain further relevance. The DCB-BIF trial, which randomised 784 patients with true bifurcation lesions to receive either a DCB or a non-compliant balloon for side-branch treatment, demonstrated a significant reduction in the composite endpoint of cardiac death, target-vessel MI, or clinically driven TLR (7.2 % vs 12.5 %; hazard ratio [HR] 0.56; P = 0.013), driven mainly by fewer target-vessel MIs (1.0 % vs 3.6 %; HR 0.27; P = 0.029). The consistency between these two studies reinforces the potential role of DCB therapy as an adjunct to main-vessel stenting, suggesting that DCBs may not only improve angiographic outcomes but also reduce ischemic events in appropriately selected patients.
Clinically, a “DES in main branch + POT + KBI + DCB in side branch” approach may enhance side-branch patency and reduce restenosis while avoiding additional metal layers. Nonetheless, careful patient and lesion selection remains essential as simple bifurcations with adequate vessel size and proper lesion preparation are most likely to yield favorable outcomes.
Longer-term follow-up, comparative studies involving sirolimus-based DCBs, and trials incorporating systematic imaging guidance are needed to confirm the durability and generalisability of these findings.
Reference
Gao X, Tian N, Kan J, Li P, Wang M, Sheiban I, Figini F, Deng J, Chen X, Santoso T, Shin ES, Munawar M, Wen S, Wang Z, Nie S, Li Y, Xu T, Wang B, Ye F, Zhang J, Shou X, Chen SL. Drug-Coated Balloon Angioplasty of the Side Branch During Provisional Stenting: The Multicenter Randomized DCB-BIF Trial. J Am Coll Cardiol. 2025 Jan 7;85(1):1-15.




No comments yet!