2024 ESC Guidelines: Peripheral arterial and aortic diseases - Focus on Peripheral Arterial Diseases
Reported from ESC Congress 2024
The 2024 ESC Guidelines for aortic diseases, merged with peripheral arterial disease guidelines, update prior guidance and emphasize atherosclerotic conditions. In this article, Antoine Sauguet summarizes the content related to peripheral arterial diseases.
Focus on peripheral arterial diseases
Peripheral arterial and aortic diseases (PAAD) are highly prevalent and significantly increase cardiovascular mortality and morbidity in the general population, consequently, intensive preventive strategies are needed. However, patients with PAAD are generally underdiagnosed and undertreated compared with patients with coronary artery disease. These 2024 guidelines address PAAD, updating and merging the 2017 peripheral arterial diseases guidelines. New guidelines explore treatment options, assess patient values, and reach decisions collaboratively with multidisciplinary approach in expert and high-volume PAAD centres for complex patients or procedures. We will focus on what’s new concerning medical management for PAAD and address different strategies regarding different lesions to treat.
Medical management PAD
1 - Lipid-lowering therapy
Patients with symptomatic peripheral artery disease (PAD) are at very high CV risk but are usually inadequately managed compared with patients with CAD. Both LDL-C reduction by ≥50% from baseline and an LDL-C goal of <1.4 mmol/L (<55 mg/dL) are recommended to obtain a reduction in CV death, MI, and stroke, and to improve walking distance, Class IA. Statins are recommended in all patients with PAD. If the target LDL chol is not achieved on maximally tolerated statins and ezetimibe, treatment with a PCSK9 inhibitor is recommended to achieve target values (Class IA).
2 - Recommendations for exercise therapy
Supervised exercise training (SET) is recommended for patients with symptomatic PAD and for patients after endovascular revascularization as an adjuvant therapy (Class IA). Training frequency at least three times per week with session duration of at least 30 min and training duration at least 3 months before superficial femoral artery revascularization decision making (Class IB).
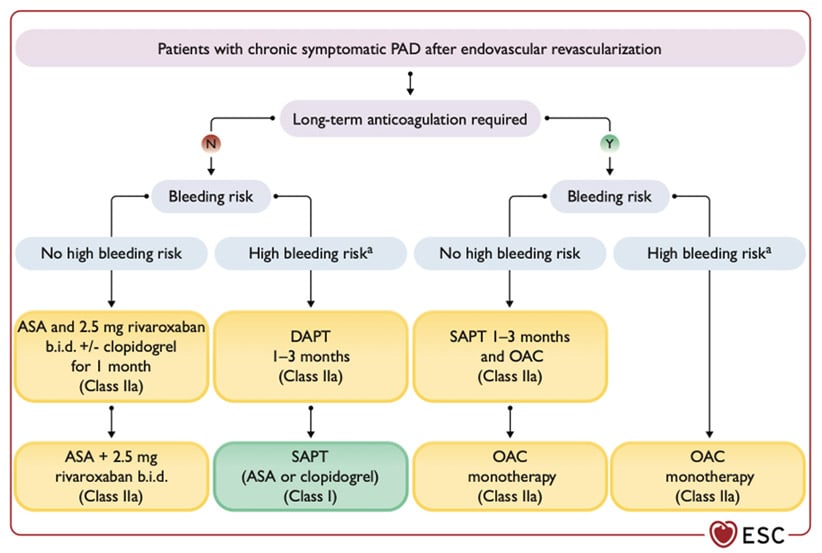
3 - Recommendations for antithrombotic therapy in patients with PAD
Aspirin (75-100mg) for primary prevention may be considered in patients with asymptomatic PAD and diabetes, in the absence of contra indications (Class IIBA).
Aspirine alone or clopidogrel alone is recommended for MACE reduction in patients with symptomatic PAD (class IA). Treatment with combination of rivaroxaban 2.5mg b.i.d an aspirin (100mg) should be considered for patients with PAD and high ischemic risk, non-high bleeding risk (Class IIa A) and for those patients following lower limb revascularization (Class IIa B)
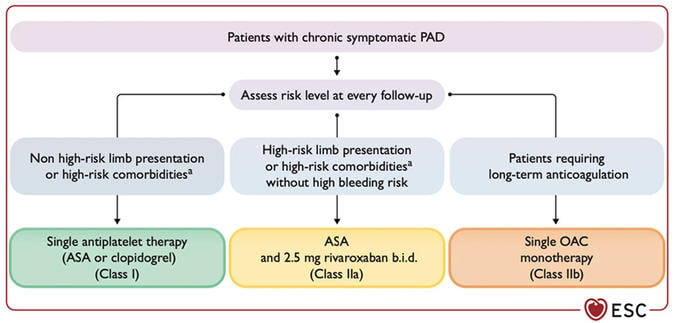
Source: European Heart Journal
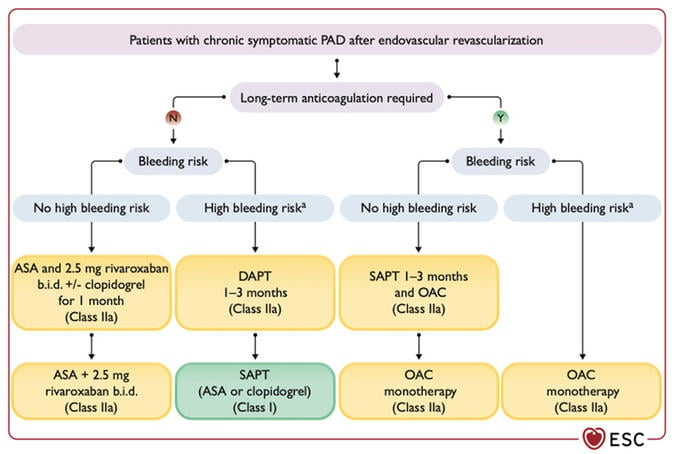
Source: European Heart Journal
4 - Recommendations for imaging in patients with PAD
Duplex ultrasound is recommended as the first-line imaging method to confirm PAD lesions (class IC). Analysis of anatomical imaging tests is crucial to rely lesion to symptoms and hemodynamic tests before invasive procedure, CTA and /or MRA are recommended as adjuvant techniques to prepare revascularization procedures for aorto iliac or multi-segmental complex disease (Class IC)
Lower limb revascularization
1 - Aorto-iliac lesion revascularization
Aorto-iliac lesions can be treated by either an endovascular or a surgical approach according to the lesion morphology and patient risk. Long-term patency with a low risk of complications can be achieved by balloon angioplasty with or without stenting in external iliac arteries or primary stenting in common iliac arteries (ClassIIaB). A meta-analysis evaluated outcomes of open surgery vs. an endovascular approach in aorto-iliac lesions (TASC II C-D) and found that short-term morbidity and mortality favours the endovascular approach, but early and mid-term primary patency favours open surgery. However, secondary patency is comparable in all groups.
2 - Femoro-popliteal lesion revascularization
If revascularization is indicated, endovascular therapy should be the first choice even for complex lesions, especially in surgical high-risk patients. Endovascular therapy faces the challenge of sustaining long-term patency and durability in the femoro-popliteal region, particularly post-stent placement in a highly mobile artery. Drug-eluting balloons have improved long-term patency in complex patient cohorts and lesions. With regard to paclitaxel-coated devices, a meta-analysis caused a decline in their usage, especially as the United States Food and Drug Administration (FDA) reacted and restricted their use. Consequently, data from large national databases were evaluated and the mortality signal could not be confirmed. The FDA revised its position, and drug-eluting treatment is now deemed to be a safe and efficient treatment strategy for femoro-popliteal lesions.
In femoro-popliteal lesions, drug-eluting treatment should be considered as the first-choice strategy (ClassIIaA).
An open surgical approach in femoro-popliteal lesions should be considered when an autologous vein (e.g. great saphenous vein [GSV]) is available and the patient shows low surgical risk, and in complex lesions after an interdisciplinary team discussion.
3 - Below the knee
In short infra-popliteal lesions, endovascular therapy is the first choice. Drug-eluting balloons and bare metal stent implantation have shown no superiority over plain balloon angioplasty, although drug-eluting stents may be used for relatively short proximal lesions.
4 - Critical limb ischemia (CLI)
For patients with CLI, it is recommended to perform revascularization as soon as possible (Class IB). Individual risk assessment by multi-disciplinary vascular team is needed to choose endovascular versus surgical revascularization (ClassIC). If patient needs open surgery for femoro popliteal lesions autologous veins are recommended (Class IB). In CLI patients, endovascular treatment may be considered as first-line therapy, especially in patients with increased surgical risk or inadequate autologous veins (Class IIbB).
Carotid artery stenosis and subclavian artery stenosis
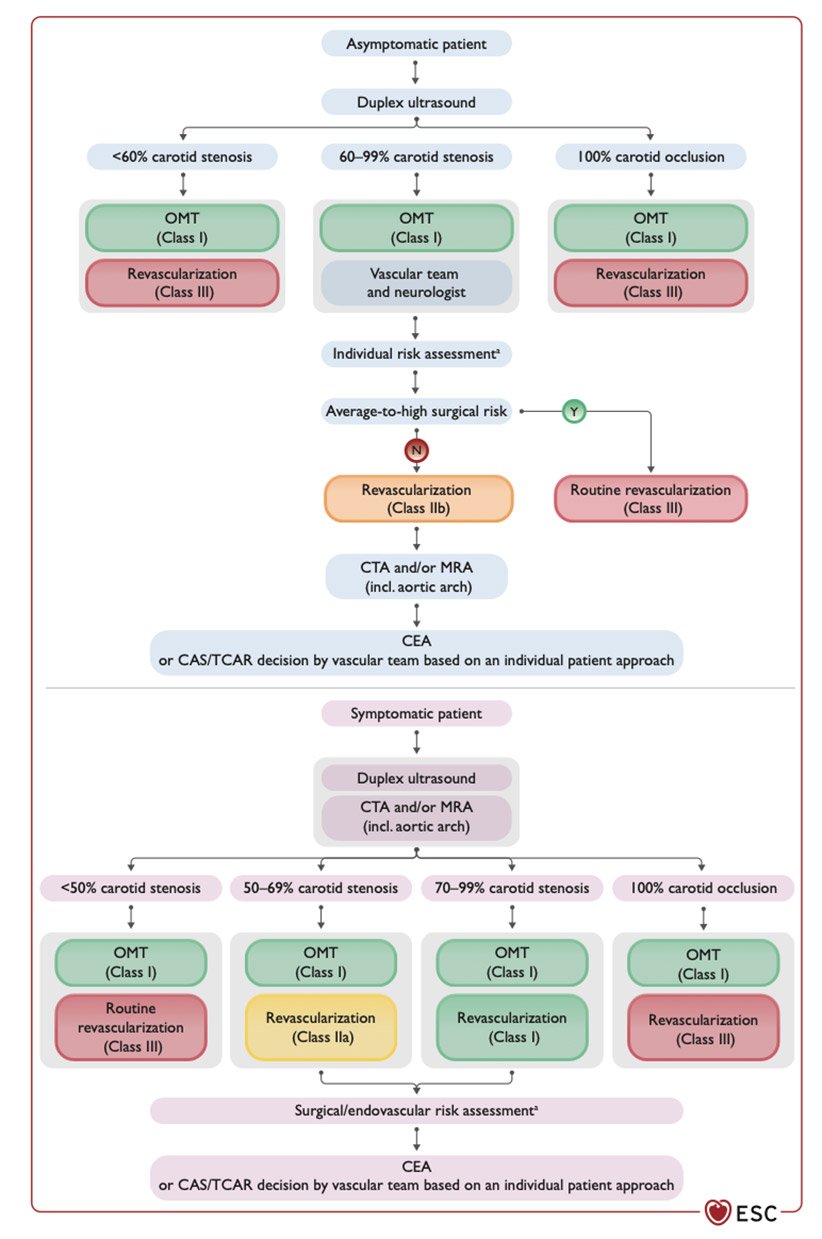
Regarding recent studies on carotid artery stenosis management with comparison on endovascular, endarterectomy and optimal medical therapy ESC guidelines give a clear algorithm for asymptomatic and symptomatic patients

Source: European Heart Journal
Concerning subclavian artery stenosis there is no place for asymptomatic routine revascularization. We could consider treatment only in case of mammary bypass (ClassIIaC).
Renal artery stenosis
Duplex ultrasound is recommended as the first-line imaging modality in patients with suspicion of renal artery stenosis (RAS) (ClassIB). In patients with unilateral or bilateral atherosclerotic RAS > 70% with signs of kidney viability, renal artery revascularization should be considered after optimal medical therapy (ClassIIaB). A clear algorithm for RAS diagnostic and treatment is summarized below.
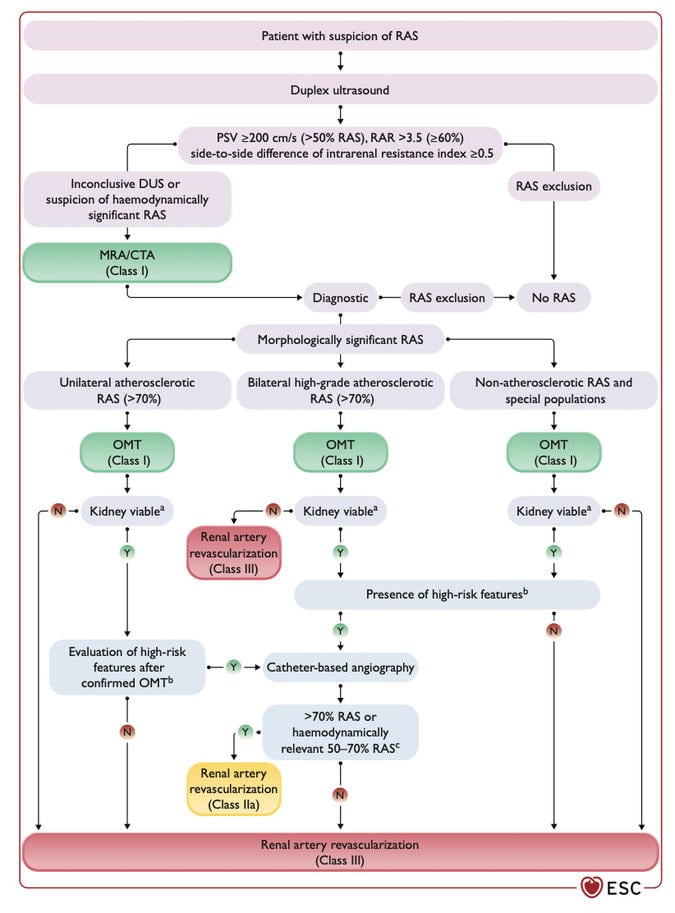
Source: European Heart Journal






No comments yet!