Early intervention in patients with asymptomatic severe aortic stenosis and left ventricular myocardial fibrosis (EVOLVED)
Reported from TCT 2024
Ali Nazmi Calik provides his take on the EVOLVED trial presented by Marc Dweck at TCT 2024 in Washington.
Why this study? – The rationale/objective
Aortic valve replacement (AVR), whether through surgical or transcatheter methods, is a fundamental treatment option primarily for patients experiencing severe aortic stenosis (AS) who are symptomatic or have a left ventricular ejection fraction (LVEF) of less than 50%. (1,2) In asymptomatic patients with severe aortic stenosis, current guidelines recommend a strategy of watchful waiting until symptoms develop. Nevertheless, the results of RECOVERY and AVATAR trials have suggested that early aortic valve intervention may improve clinical outcomes in select younger patients with asymptomatic severe aortic stenosis and normal LVEF. (3,4)
Beyond plasma high-sensitivity cardiac troponin I levels and left ventricular hypertrophy on ECG, midwall late gadolinium enhancement (LGE) on cardiac magnetic resonance imaging (CMRI) provides a more definitive specific measure of cardiac damage through the identification of myocardial fibrosis, the key pathological process driving the transition from left ventricular hypertrophy to heart failure in AS.
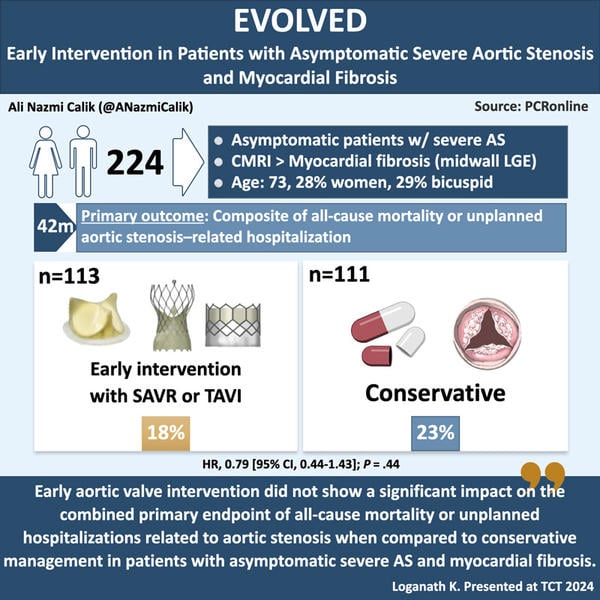
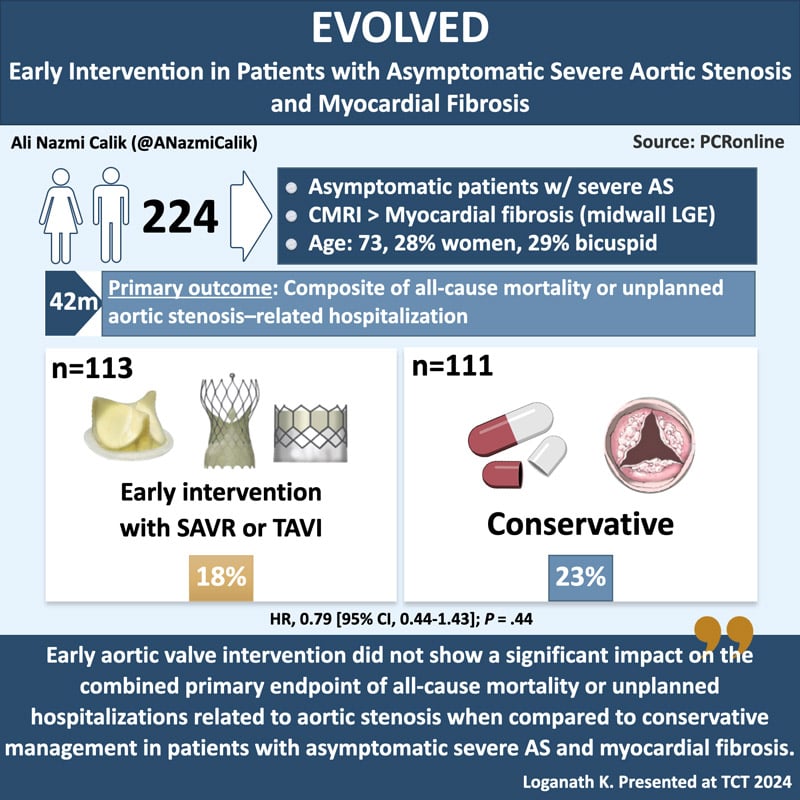
The Early Valve Replacement Guided by Biomarkers of Left Ventricular Decompensation in Asymptomatic Patients with Severe Aortic Stenosis (EVOLVED) trial aimed to develop an enrichment strategy using these biomarkers to identify asymptomatic patients with severe AS who showed evidence of myocardial fibrosis. It was designed to investigate whether early aortic valve intervention can enhance clinical outcomes in patients with asymptomatic severe AS and myocardial fibrosis.
How was it executed? - The methodology
The EVOLVED trial is a parallel-group, multicenter, prospective, randomized, open-label, masked end-point trial conducted across 24 cardiac centers in the UK and Australia. Patients aged 18 years or older with severe AS and without symptoms due to valve disease were included in the study. The attending physician assessed for the presence of AS–related symptoms with the option of exercise stress testing according to their clinical practice. Routine exercise stress testing was not mandated because of the challenges of interpretation and consequent exclusion of many patients who would be unable to perform exercise stress due to poor mobility or comorbidities. Patients having symptoms attributable to AS, LVEF less than 50%, concomitant severe aortic or mitral regurgitation, estimated glomerular filtration rate less than 30 mL/min/1.73 m2, contraindications to MRI were excluded from the study.
Potentially eligible participants who met any of the criteria—specifically, having a plasma cardiac troponin I concentration greater than or equal to 6 ng/L or exhibiting left ventricular hypertrophy on ECG, both indicative of adverse left ventricular remodelling—underwent CMRI with gadolinium contrast following a standardized protocol. The presence or absence of midwall LGE was assessed by the core laboratory blinded to clinical details. Eligible participants with midwall myocardial fibrosis were randomly assigned in a 1:1 ratio to receive early aortic valve intervention or guideline-directed management.
In the intervention group, the choice of surgical AVR or transcatheter aortic valve implantation (TAVI) was made by the local heart valve team. Patients assigned to receive guideline-directed conservative management received treatment and were referred for aortic valve intervention at the discretion of their treating physician and local heart valve team.
The primary endpoint was a composite of all-cause mortality or unplanned aortic stenosis–related hospitalization during the median follow-up of 42 months.
Secondary endpoints included the individual components of the composite primary endpoint, symptom burden assessed by the New York Heart Association (NYHA) classification, and the development of left ventricular systolic dysfunction (ejection fraction less than 50%) 12 months after randomization.
What is the main result?
Between August 4, 2017, and October 31, 2022, a total of 427 asymptomatic patients with severe AS were screened. Of the 224 eligible participants with myocardial fibrosis detected by CMRI, 113 patients were randomized to receive early aortic valve intervention and 111 to receive guideline-directed conservative management. The average age of participants was 73, 28% were women and 64 (29%) had a bicuspid aortic valve.
In the early intervention group, 106 patients (94%) received aortic valve intervention and 97 (86%) received it within 12 months of randomization (median time to intervention was 5.0 months). SAVR was performed in 80 patients (75%) and TAVI in 26 patients (25%).
In the guideline-directed conservative management group, 85 patients (77%) received aortic valve intervention and 31 (28%) received it within 12 months of randomization (median time to intervention was 20.2 months). SAVR was performed in 47 patients (55%) and 38 (45%) underwent TAVI.
The primary composite end point of all-cause death or unplanned aortic stenosis-related hospitalization occurred in 20 patients (18%) in the early aortic valve intervention group and 25 (23%) in the guideline-directed conservative management group (HR, 0.79 [95% CI, 0.44-1.43]; P = .44). There were also no differences between the groups in the prespecified secondary endpoints of all-cause mortality and aortic stenosis–related mortality. Two secondary endpoints worth noting were unplanned aortic stenosis–related hospitalization and symptom burden during follow-up, both of which were less frequent in the early AVR group. Seven patients (6%) in the early aortic valve intervention group and 19 patients (17%) in the guideline-directed conservative management group experienced unplanned aortic stenosis–related hospitalization (HR, 0.37 [95% CI, 0.16-0.88]). At 1 year of follow-up, 21 patients (20%) in the early intervention group and 39 (38%) in the guideline-directed conservative management group had NYHA class II-IV symptoms (adjusted odds ratio, 0.37 [95% CI, 0.20-0.70]).
Critical reading and the relevance for clinical practice
In this trial, the population at increased cardiac risk was enhanced by using cardiac biomarkers and CMRI. A specific group of patients with aortic stenosis was chosen, characterized by early left ventricular decompensation due to their severe valve disease. The hypothesis posited that these high-risk asymptomatic patients would benefit the most from a strategy of early aortic valve intervention. Nevertheless, the trial intervention did not show a significant effect on the primary outcome.
The mortality outcomes of the current trial are at odds with the findings of the RECOVERY and AVATAR trials, which demonstrated a mortality benefit and focused on younger patients with very severe aortic stenosis. Despite focusing on a high-risk population with myocardial fibrosis, the current trial indicates that the observed benefits of early intervention on mortality cannot be generalized to the larger older demographic with asymptomatic severe aortic stenosis, who typically have a higher burden of comorbid conditions. In fact, the study revealed that only one-third of the deaths were linked to the patient's underlying aortic valve disease, suggesting that the majority of fatalities were not influenced by aortic valve intervention.
In contrast to mortality outcomes, the current study indicated that patients receiving guideline-directed conservative management experienced a greater burden of heart failure symptoms at 12 months, which was not observed in those who underwent early aortic valve intervention. Furthermore, early aortic valve intervention was associated with fewer unplanned hospitalizations related to aortic stenosis compared to conservative management following guidelines. That said, the results indicating that early intervention was linked to a reduced incidence of unplanned aortic stenosis-related hospitalizations and a better symptom burden should be viewed as hypothesis-generating, as the study did not achieve its primary endpoint and was not adjusted for multiple comparisons. These hypotheses need to be addressed in future larger trials, such as the EASY-AS trial (NCT04204915). (5)
The following limitations should be taken into account when applying the results of the current study to daily practice. First, the underenrollment resulting from the COVID pandemic indicates that the trial was likely underpowered to meet its primary objective. Additionally, the number of primary events observed in the conservative group was smaller than expected, contributing to the wide confidence intervals (CIs). For these reasons, further research is needed to confirm the findings. Second, the rate of TAVI was greater in the guideline-directed conservative management group (45%) compared to the early intervention group (25%). This disparity likely reflects improved access to TAVI during the study and the necessity for urgent intervention following unplanned hospitalizations related to aortic stenosis, where patients may have been too ill to undergo SAVR. Third, there was a significant delay (with a median of 5 months) between randomization and aortic valve replacement (AVR) in the early intervention group, likely due in part to the scheduling practices for SAVR in the UK and Australia. Additionally, there were 6 patients in the early intervention group affected by this delay. Consequently, the implications of this delay and its outcomes may not be applicable to other countries. As both groups had LGE evidence of irreversible fibrosis, future trials might study whether it is more advantageous to intervene in asymptomatic patients before the development of LGE. A notable strength of the current study protocol is that patients without detectable myocardial fibrosis were included in an observational registry.
In conclusion, early aortic valve intervention did not show a significant impact on the combined primary endpoint of all-cause mortality or unplanned hospitalizations related to aortic stenosis when compared to guideline-directed conservative management in patients with asymptomatic severe AS and myocardial fibrosis. Additionally, the wide 95% CI surrounding the primary endpoint indicates that further research is necessary to validate these findings.
References
- Vahanian A, Beyersdorf F, Praz F, et al; ESC/EACTS Scientific Document Group. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022;43(7):561-632.
- Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;143(5):e72-e227.
- Kang DH, Park SJ, Lee SA, et al. Early surgery or conservative care for asymptomatic aortic stenosis. N Engl J Med. 2020;382(2):111-119.
- Banovic M, Putnik S, Penicka M, et al; AVATAR Trial Investigators. Aortic valve replacement versus conservative treatment in asymptomatic severe aortic stenosis: the AVATAR Trial. Circulation. 2022;145(9):648-658.
- Richardson C, Gilbert T, Aslam S, et al. Rationale and design of the early valve replacement in severe asymptomatic aortic stenosis trial. Am Heart J. 2024;275:119-127.






No comments yet!