PCI or CABG for left main coronary artery disease: the SWEDEHEART registry
Selected in European Heart Journal by P. Xaplanteris , L. Koliastasis
While the choice between PCI and CABG for LMCA disease continues to be one of the most controversial topics, patient characteristics & comorbidities must be taken into account, as must the external validity of the results of RCTs in the real world, as the SWEDEHEART registry does.
References
Authors
Jonas Persson, Jacinth Yan, Oskar Angerås, Dimitrios Venetsanos, Anders Jeppsson, Iwar Sjögren, Rikard Linder, David Erlinge, Torbjörn Ivert, Elmir Omerovic
Reference
European Heart Journal, ehad369, https://doi.org/10.1093/eurheartj/ehad369
Published
08 June 2023
Link
Read the abstract
Reviewers
Our Comment
Why this study – the rationale/objective?
The choice between percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) for left main coronary artery (LMCA) disease continues to be one of the most heated topics among cardiologists and cardiac surgeons.
Randomized controlled trials (RCT) have reported better outcomes for either CABG (NOBLE trial) or PCI (EXCEL trial), while the 2018 ESC/EACTS guidelines on myocardial revascularization suggest equivalent results for death, myocardial infarction (MI) and stroke up to 5 years of follow-up, based on RCTs and meta-analyses.
Patient characteristics and comorbidities should be taken into account, bearing in mind that not all patient subsets are equally represented in RCTs. In addition, reports on the external validity of RCT results in the real-world setting are scarce. The recently published analysis of real-world data from the SWEDEHEART registry comes to fill this gap.
How was it executed? - the methodology
This observational study included patients with LMCA disease who were eligible for CABG. Patients with previous CABG, cardiogenic shock or ST-elevation myocardial infarction (STEMI) were excluded.
Data from 28 centers in Sweden spanning 11 years were analyzed leading to 11,137 eligible patients. CABG was performed in 9,364 patients, and PCI with drug eluting stents (1st, 2nd or 3rd generation) in 1,773 patients, with a median follow-up of 4.7 years.
In order to account for differences in baseline characteristics between the two treatment groups, all variables associated to cardiovascular mortality that were available in the registry were used for weight adjustments in the statistical analysis and the inverse probability weighting (IPW) method was applied.
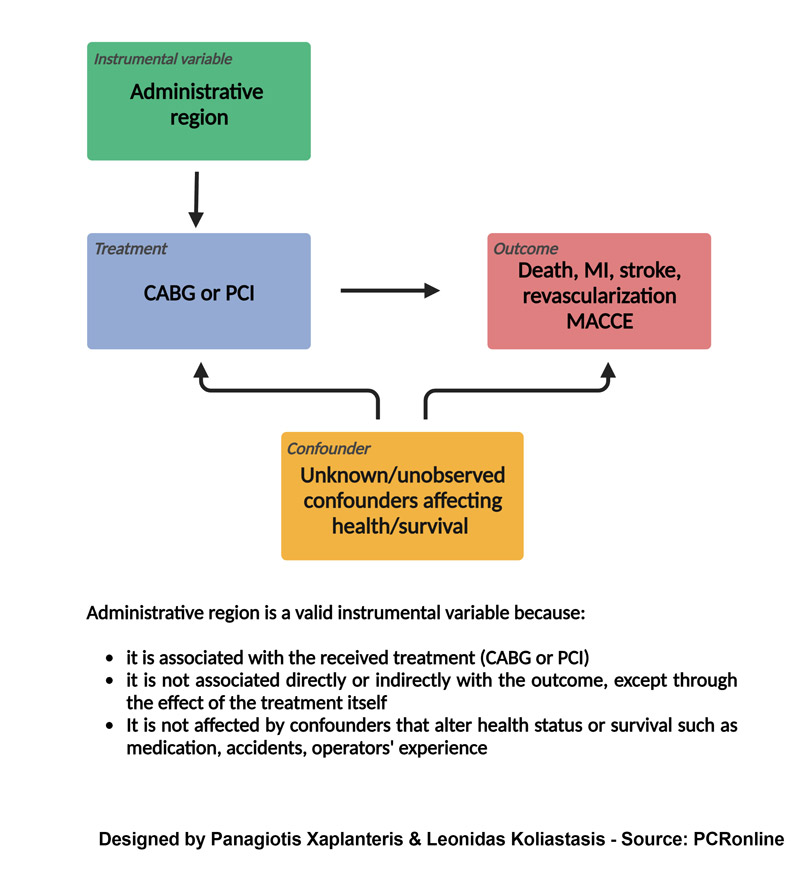
A novelty of this study is the use of instrumental variable analysis (IV) in order to adjust for unknown confounders. The principle of IV analysis is shown in Figure 1.
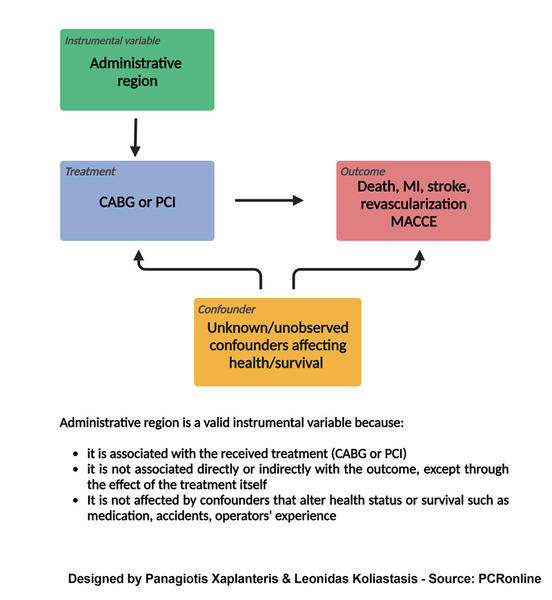
Figure 1: Principle of instrumental variable analysis
Designed by Panagiotis Xaplanteris & Leonidas Koliastasis
What is the main result?
- CABG was more frequently chosen for patients with multivessel disease, diabetes, smoking and peripheral artery disease. Patients treated with PCI were older with higher prevalence of comorbidities and isolated LMCA disease. Acute coronary syndrome as the cause of revascularization was more frequent in the PCI group and 75 % of them received 2st generation DES.
- The incidence of death was significantly higher in the PCI group after adjusting for known (with IPW analysis) and unknown confounders (with IV analysis): IPW - HR 2.0, 95 % CI: 1.5-2.7 and IV - HR 1.5, 95 % CI: 1.1-2.0.
- Major cardiovascular and cerebrovascular adverse events (MACCE) were more common with PCI after adjusting for known (IPW - HR 2.5, 95 % CI: 1.9-3.2) as well as unknown confounders (IV - HR 2.8, 95 % CI: 1.8-4.5). There was an interaction for MACCE showing benefit from CABG in patients ≤ 70 years and those with multivessel disease.
- CABG demonstrated a favorable outcome for diabetics that was translated into 3.6 additional free-of-death years.
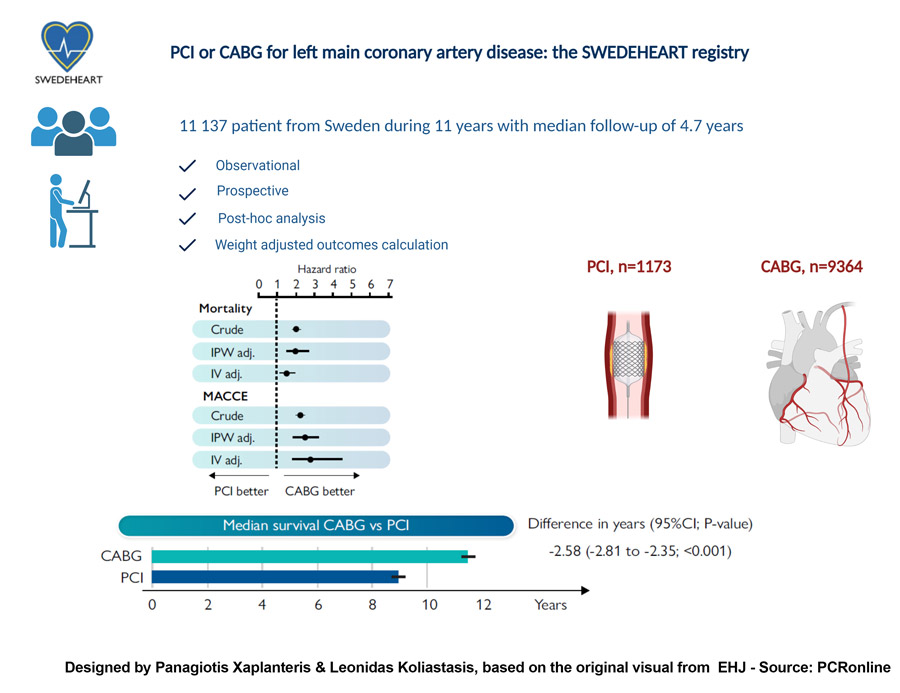
Figure 2: The SWEDEHEART Registry design and results
Designed by Panagiotis Xaplanteris & Leonidas Koliastasis, based on the original visual from EHJ
Critical reading and the relevance for clinical practice
This large observational study provides useful insights on real-world outcomes of PCI and CABG for LMCA revascularization; in a non-RCT context, the benefit of CABG in all hard endpoints is shown over a follow-up period of 5 years.
The design, analysis and results of the study additionally bring up a number of points for critical reflection:
- Is the discordance in outcomes between this study and RCTs due to its observational, non-randomized nature? RCTs are considered as providing the highest level of evidence to inform therapeutic decisions; this is mostly due to randomization and the administration of the highest quality of care in a group of patients that meets specific inclusion criteria. Observational studies reflect real world practice which does not always align with the “ideal” setting of an RCT and refer to an all-comers population. In this respect, the findings from the SWEDEHEART registry are not necessarily contradictory to what has been reported by previous RCTs and meta-analyses. The fact that PCI was more frequently chosen for older, sicker patients may partially explain the results in favor of CABG. The use of sophisticated statistical methods (IPW and IV analysis) to account for confounding factors may not fully adjust for residual confounding.
- Almost 70 % of patients in SWEDEHEART had NSTEMI/unstable angina as the presenting indication for revascularization. This differs from RCTs where patients were mostly included because of chronic coronary syndrome.
- Diabetes mellitus reemerges as a risk factor that should be taken into account for clinical decision making when choosing between PCI and CABG for LMCA disease. Ìn SWEDEHEART, a mortality benefit exists for diabetic patients treated with CABG, whereas no such interaction was noted in the NOBLE and EXCEL trials.






No comments yet!