Optical coherence tomography- vs angiography-guided coronary stent implantation in calcified lesions: the ILUMIEN IV trial
Selected in European Heart Journal by S. Brugaletta
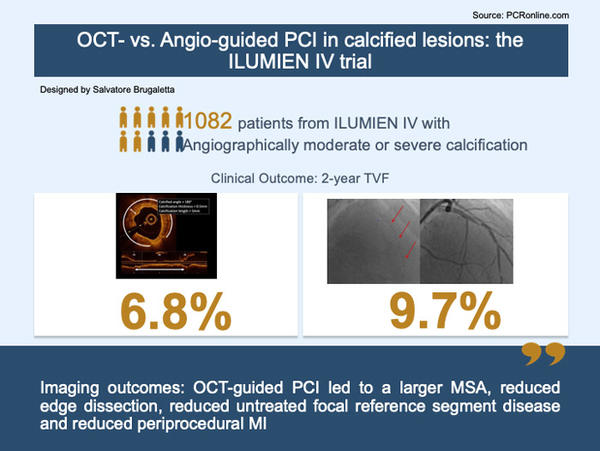
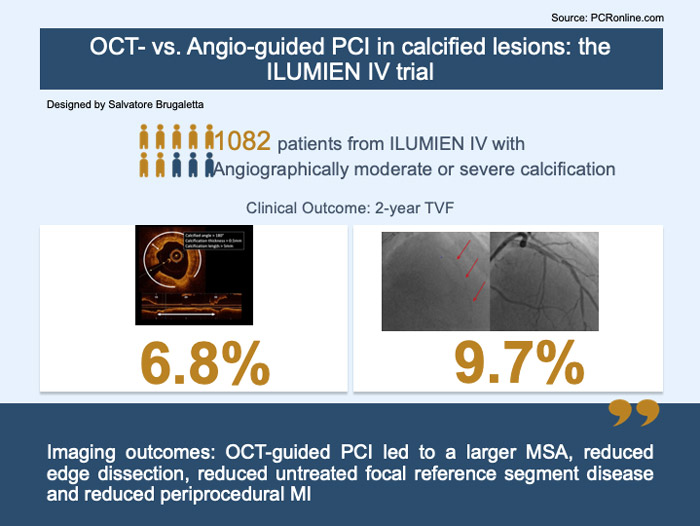
In the overall population (n = 2,114), there was a significant interaction between the effect of randomisation to OCT guidance vs angiography guidance in lesions with moderate/severe calcification (n = 1,082) vs no/mild calcification (n = 1,032) on the 2-year rate of TVF (Pinteraction = 0.01).
References
Authors
Ziad A Ali , Doosup Shin , Rajesh Vijayvergiya , Atit A Gawalkar , Richard A Shlofmitz , Fernando Alfonso , Giuseppe Calligaris , Paolo Canova , Koshiro Sakai , Matthew J Price , David Leistner , Francesco Prati , Gary Mintz , Mitsuaki Matsumura , Robert J McGreevy , Robert W McNutt , Hong Nie , Jana Buccola , Ulf Landmesser , Akiko Maehara , Gregg W Stone for the ILUMIEN IV Investigators
Reference
European Heart Journal, Volume 46, Issue 32, 21 August 2025, Pages 3201–3210
Published
05 June 2025
Link
Read the abstractReviewer
My Comment
Designed by: Salvatore Brugaletta
Source: PCRonline.com
Why this study – the rationale/objective?
Coronary artery calcification represents a significant challenge in percutaneous coronary intervention (PCI).
PCI of calcified coronary lesions is associated with an increased risk of suboptimal stent implantation, procedural complications, and long-term adverse events.
No prior RCT has reported detailed outcomes specifically in patients with calcified coronary lesions undergoing PCI, and it remains unclear whether and how OCT guidance can improve procedural and clinical outcomes in this complex lesion subset.
How was it executed? The methodology
Patients with a single PCI target lesion from the ILUMIEN IV trial were included in the present analysis. The presence of none, mild, moderate or severe lesion calcification was determined by an angiographic core laboratory.
The primary imaging endpoint was the post-PCI minimal stent area (MSA) assessed by OCT. The primary clinical endpoint was 2-year target-vessel failure (TVF), a composite of cardiac death, target-vessel myocardial infarction (TV-MI), or ischaemia-driven target-vessel revascularisation.
What is the main result?
In the overall population (n = 2,114), there was a significant interaction between the effect of randomisation to OCT guidance vs angiography guidance in lesions with moderate/severe calcification (n = 1,082) vs no/mild calcification (n = 1,032) on the 2-year rate of TVF (Pinteraction = 0.01).
The post-PCI MSA in moderately and severely calcified lesions was larger with OCT guidance (n = 544) compared with angiography guidance (n = 538) (5.57 ± 1.86 mm2 vs 5.33 ± 1.78 mm2; P = 0.03).
In the moderate/severe calcified lesion cohort, TVF within 2 years occurred in 35 patients with OCT guidance and in 51 patients with angiography guidance (6.8 % vs 9.7 %; adjusted hazard ratio [aHR] 0.62; 95 % confidence interval [CI] 0.40–0.96), whereas there was no significant difference in TVF in the no/mild calcified lesion cohort (7.7 % vs 5.2 %; aHR 1.48; 95 % CI 0.90–2.44) (Pinteraction = 0.01).
In moderately/severely calcified lesions, OCT-guided PCI also reduced the 2-year rates of serious major adverse cardiac events (2.8 % vs 4.7 %; aHR 0.49; 95 % CI 0.25–0.95; P = 0.03), TV-MI (1.9 % vs 4.0 %; aHR 0.36; 95 % CI 0.17–0.79; P = 0.01), and stent thrombosis (0.2 % vs 1.5 %; aHR 0.11; 95 % CI 0.01–0.89; P = 0.04) compared with angiography-guided PCI.
Critical reading and the relevance for clinical practice:
In patients with angiographically moderately or severely calcified lesions undergoing PCI in the large-scale ILUMIEN IV trial, OCT guidance led to a larger final MSA and reduced the 2-year risks of TVF, a composite of cardiac death, TV-MI, or ID-TVR, compared with angiography guidance, as well as stent thrombosis and both early and late serious MACE.
PCI with OCT guidance may be especially beneficial when treating patients with moderate or severe lesion calcification, mitigating the poor prognosis in this high-risk cohort compared with PCI in patients without calcified coronary lesions.
Although these findings may appear quite obvious, it is important to reflect on it. Lesions included were not necessarily treated by advanced lesion preparation, meaning that OCT is helpful also when we are not planning to use such devices. OCT may help us in understanding how to prepare better the lesion - even with a NC balloon. More importantly, OCT helps us in reaching a good IC imaging result which is not the same as a good angiographic result. This lack of correspondence between angio and IC imaging should motivate us to look beyond angio when we see calcium if we want to assure the best outcome to our patient. This is unfortunately not the current practice worldwide.
How many of you use IC imaging when making a PCI of an angiographically calcified lesion?





No comments yet!