Valve-in-valve transcatheter aortic valve implantation versus repeat surgical aortic valve replacement in patients with a failed aortic bioprosthesis
Selected in EuroIntervention by M. Alasnag , P. Looser
Structural valve deterioration remains the Achilles heel of both SAVR and TAVI. Since indications for TAVI have expanded to low-risk patients in 2019, this clinical scenario poses a significant conundrum for physicians and surgeons, as the number of patients undergoing aortic valve interventions continues to grow and patients live longer, ultimately requiring additional valvular interventions.
References
Authors
Monil Majmundar , Rajkumar Doshi, Ashish Kumar, Douglas Johnston, James Brockett, Anmar Kanaa'N, Joseph A Lahorra, Lars G Svensson, Amar Krishnaswamy, Grant W Reed, Rishi Puri, Samir R Kapadia, Ankur Kalra
Reference
10.4244/EIJ-D-21-00472
Published
September, 15 2021
Link
Read the abstractReviewers
Our Comment
Why this study? – the rationale/objective
Structural valve deterioration remains the Achilles heel of both surgical aortic valve replacement (SAVR) and transcatheter aortic valve implantation (TAVI). Since TAVI was approved for valve-in-valve implantation in 2015 for patients with a degenerated aortic valve prostheses, controversy has existed regarding the optimal strategy for treatment of these patients. Advancements in technology, improvement in procedural success, and lower complication rates have made TAVI an efficient treatment strategy for a subset of these patients. However, surgical outcomes during this time period were also excellent, with comparable morbidity and mortality. Since indications for TAVI have expanded to low-risk patients in 2019, this clinical scenario poses a significant conundrum for physicians and surgeons, as the number of patients undergoing aortic valve interventions continues to grow and patients live longer, ultimately requiring additional valvular interventions.
The existing data comparing valve in valve TAVI (ViV TAVI) and redo surgical AVR show comparable results but are somewhat limited. In a study of the French administrative database PMSI (French Programme de Médicalisation des Systèmes d’Information), a propensity-matched cohort of 717 undergoing ViV TAVI versus redo SAVR, TAVI patients demonstrated favorable short term results at 30 days. However, there was a trend toward lower mortality at four years in the SAVR cohort.
Given the lack of available data informing clinicians, the authors sought to elucidate the short-term outcomes in a cohort of patients in the US undergoing repeat SAVR or ViV TAVI for degenerated surgical prostheses.
How was it executed? - the methodology
The authors queried the National Readmission Database (NRD) from 2016 to 2018 using the International Classification of Diseases, Tenth Revision (ICD-10) (Z95.2) and included all adults (≥ 18 years) with a history of prosthetic valves and who had undergone TAVI or SAVR.
Two cohorts were evaluated: one for in-hospital and 30-day outcomes and the second for 6-month outcomes. Patients undergoing concomitant coronary artery bypass graft (CABG), mitral, tricuspid, or pulmonary valve, atrial or ventricular septum closure surgeries were excluded from both cohorts.
Baseline characteristics and center volumes were captured. The primary endpoint was in-hospital mortality and readmission at 30 days and 6 months. The secondary outcomes were defined as major adverse cardiac events (MACE), all-cause mortality, major bleeding or vascular complications, non-cardiac infection, and procedural complications. Importantly, resource utilisation, length of stay (LOS), and total cost were included in the secondary endpoints.
Multivariable regression analysis was used to assess robustness for matched cohorts. Logistic regression analysis was used to calculate the odds ratio (OR) with a 95 % confidence interval (CI) for in-hospital outcomes. Cox regression was used for 30-day and 6-month outcomes and results were reported as hazard ratio (HR) with a 95 % confidence interval.
What is the main result?
A total of 6,769 procedures were included in the analysis of which 55 % were ViV TAVI and 45 % were repeat SAVR.
Women constituted 48.9 % of the ViV TAVI and 38.9 % of the redo SAVR group.
Hypertension was the most common comorbidity in both groups. The ViV TAVI group appeared to be higher risk with a much higher rate of heart failure (80 % vs 45 %), ischemic cardiomyopathy (70.6 % vs 43.4 %), and other comorbidities such as prior myocardial infarction, prior revascularization, chronic renal failure, diabetes, and chronic pulmonary disease. The redo SAVR group had a higher rate of obesity and coagulopathy.
ViV TAVI was associated with lower in-hospital mortality (1.2 % vs 3.4 %), major bleeding (29.7 % vs 67.7), and cardiorespiratory complications (9.3 % vs 26.5 %). The median length of stay for ViV TAVI was significantly shorter (4 days vs 10 days). Other in-hospital outcomes such as stroke, vascular complications, pacemaker implantation, and cost were similar between the two groups. However, ViV TAVI had a higher rate of 30-day and 6-month all-cause readmission compared with repeat SAVR.
Critical reading and the relevance for clinical practice
An administrative database such as the Nationwide Inpatient Sample (NIS) or National Readmission Database (NRD) can be useful for elucidating overall trends in procedural volume over time, rates of complications, and in-hospital/short term mortality for uncommonly performed interventions. It also captures “real-world” data, including patients who would have been excluded from clinical trials.
Though useful for identifying trends and certain clinical outcomes, these databases can lack patient-specific variables that are germane to the question posed by the authors: for instance, frailty, aortic valve prosthesis used (balloon-expandable versus self-expanding), echocardiographic variables such as left ventricular function, coronary anatomy, etc.
The authors offer predictors of readmission for both procedures whereby LOS and chronic kidney disease were significant predictors of 30-day or 6-month readmission in both groups.
What was somewhat reassuring was the trend to lower 30-day readmissions over time. Although the ViV TAVI group had higher baseline comorbidities, this cohort had better in-hospital outcomes, particularly all-cause mortality, cardiorespiratory complications, and bleeding. This may be suggestive of improved operator experience. Whether center volume impacts these findings is unknown. The interaction of paravalvular leak and other complications such as acute kidney injury cannot be determined from this registry data.
Finally, TAVI ViV is an evolving procedure and the current analysis does not discriminate between those who underwent valve fracture or Basilica and those with ViV alone.
Overall, this data unequivocally demonstrates the safety of TAVI ViV in a higher-risk population. Future trials designed to factor in the STS score and frailty would aid clinicians and the heart team in selecting the most appropriate procedure for patients with degenerated prostheses. This is of particular importance as we move towards a discussion about lifetime management of patients with valvular heart disease.
Lifetime Management of Degenerated Prosthetic Valves
Courtesy of Mirvat Alasnag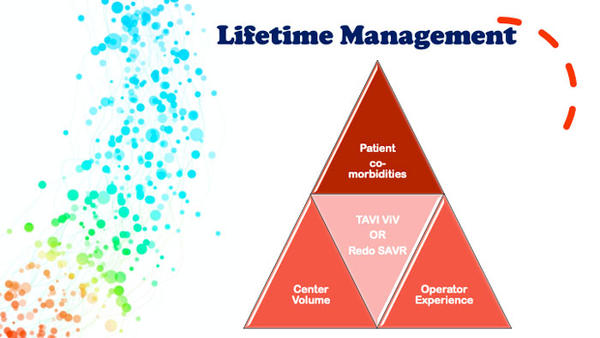
References
- Raschpichler MC, Woitek F, Chakravarty T, Flint N, Yoon SH, Mangner N, Patel CG, Singh C, Kashif M, Kiefer P, Holzhey D, Linke A, Stachel G, Thiele H, Borger MA, Makkar RR. Valve-in-Valve for Degenerated Transcatheter Aortic Valve Replacement Versus Valve-in-Valve for Degenerated Surgical Aortic Bioprostheses: A 3-Center Comparison of Hemodynamic and 1-Year Outcome. J Am Heart Assoc. 2020 Jul 21;9(14):e013973. doi: 10.1161/JAHA.119.013973. Epub 2020 Jul 9.
- Deharo P, Bisson A, Herbert J, Lacour T, Etienne CS, Porto A, Theron A, Collart F, Bourguignon T, Cuisset T, Fauchier L. Transcatheter Valve-in-Valve Aortic Valve Replacement as an Alternative to Surgical Re-Replacement. J Am Coll Cardiol. 2020 Aug 4;76(5):489-499. doi: 10.1016/j.jacc.2020.06.010. PMID: 32731926.
- Kim LK, Swaminathan RV, Looser P, Minutello RM, Wong SC, Bergman G, Naidu SS, Gade CL, Charitakis K, Singh HS, Feldman DN. Hospital Volume Outcomes After Septal Myectomy and Alcohol Septal Ablation for Treatment of Obstructive Hypertrophic Cardiomyopathy: US Nationwide Inpatient Database, 2003-2011. JAMA Cardiol. 2016 Jun 1;1(3):324-32. doi: 10.1001/jamacardio.2016.0252. Erratum in: JAMA Cardiol. 2017 Feb 1;2(2):230. Erratum in: JAMA Cardiol. 2017 Feb 1;2(2):230. PMID: 27438114.







No comments yet!