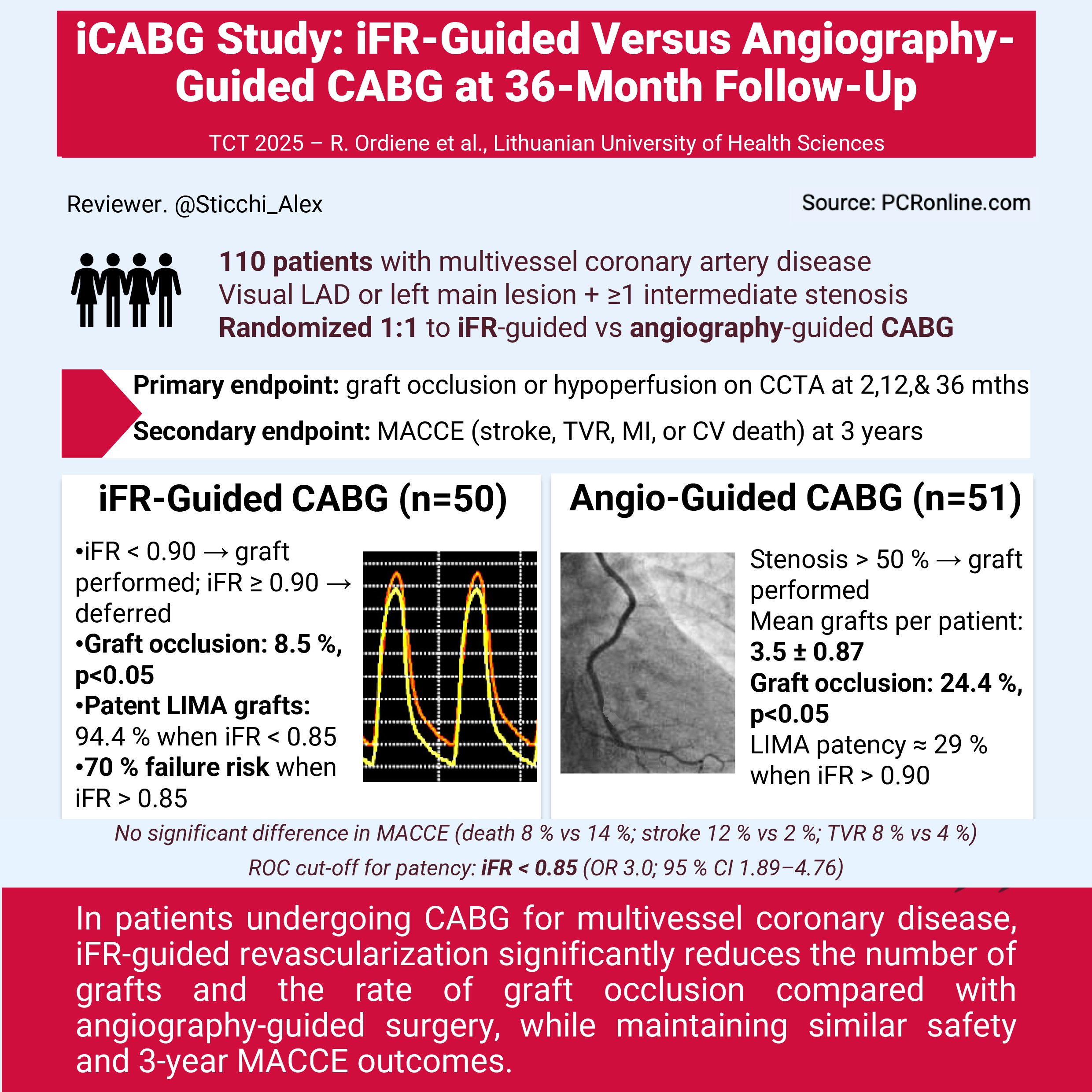
iFR versus angiography-guided CABG: 3-year results of the iCABG randomised trial
Reported from TCT 2025
Alex Sticchi provides his take on the iCABG trial presented by Rasa Ordiene at TCT 2025, in San Francisco.
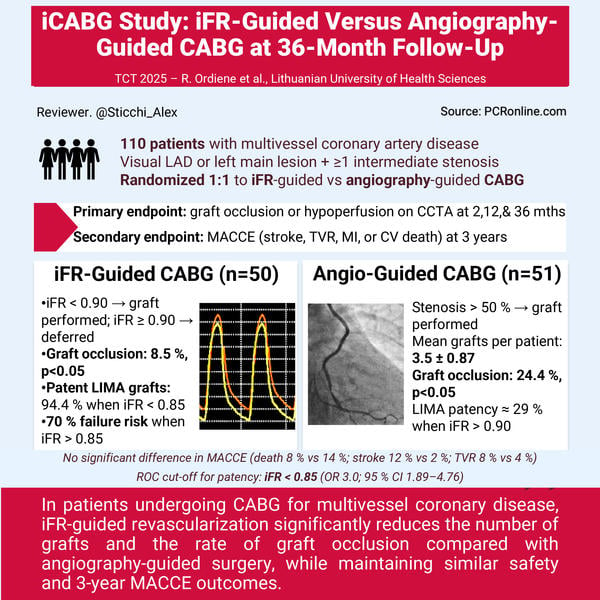
Designed by Alessandro Sticchi. Source: PCRonline.com
Why this study – The rationale / objective
Coronary artery bypass grafting (CABG) has traditionally relied on angiographic assessment to define surgical targets, despite the fact that anatomical severity does not always reflect the functional significance of coronary stenoses.
Several single-center studies using fractional flow reserve (FFR) before surgery suggested that physiology-guided grafting might reduce the number of anastomoses, limit unnecessary revascularisation, and lower the rate of graft failure in non-significant lesions, though without clear improvement in major adverse cardiac and cerebrovascular events (MACCE) up to three years.
The iCABG study was designed to assess whether physiology-guided surgical revascularisation using the instantaneous wave-free ratio (iFR) could improve graft patency and optimise procedural efficiency compared with angiography-guided CABG in patients with multivessel coronary artery disease1,2.
How was it executed – The methodology
This was a prospective, randomised, single-blind trial conducted at the Lithuanian University of Health Sciences. A total of 110 patients with multivessel coronary artery disease were referred by the Heart Team for CABG, all presenting with a visually significant LAD or left main lesion and at least one intermediate stenosis.
Patients were randomised in a 1:1 fashion to undergo either angiography-guided or iFR-guided CABG. In the angiography-guided arm, grafts were performed for lesions with > 50 % stenosis by visual estimation. In the iFR-guided arm, surgery was performed for lesions with iFR < 0.90 and deferred for those with iFR ≥ 0.90. Follow-up coronary CT angiography (CCTA) was scheduled at 2, 12, and 36 months to assess graft patency, and all patients were followed for major adverse cardiovascular and cerebrovascular events through 36 months. The primary endpoint was graft occlusion or hypoperfusion on CCTA. Secondary endpoints included MACCE, defined as stroke, target vessel revascularisation (TVR), non-fatal myocardial infarction, or cardiovascular death1,2.
What are the main results?
The iFR-guided strategy resulted in a smaller number of grafts per patient, with a mean of 2.98 ± 0.87 compared to 3.5 ± 0.87 in the angiography-guided group (p = 0.003).
Less than four grafts were performed in 76 % of patients in the iFR-guided group, versus 64 % in the angiography-guided arm.
Operative time, aortic clamp time, and in-hospital stay were similar between groups (mean duration 55–57 minutes; median hospital stay 10.5 days).
At 2 months, 94 % of patients underwent follow-up CCTA, and 78 % completed the 36-month imaging. At 36 months, graft occlusion was significantly less frequent in the iFR-guided group (8.5 %) compared with angiography-guided CABG (24.4 %, p < 0.05).
The median iFR value differed according to graft outcome: for left internal mammary artery (LIMA) grafts, median iFR was 0.83 [0.78–0.87] in patent grafts, 0.91 [0.89–0.93] in hypoperfused grafts, and 0.90 [0.85–0.94] in occluded grafts. Among venous grafts, median iFR was 0.78 [0.62–0.91] in patent and 0.96 [0.89–0.99] in occluded or hypoperfused conduits. Graft failure strongly correlated with preoperative iFR values: when iFR exceeded 0.90, only 29.4 % of LIMA grafts remained patent, while 94.4 % were patent when iFR was below 0.85. This translated into a 70 % probability of graft failure for lesions with iFR > 0.85 during the 3-year follow-up. ROC curve analysis identified an optimal cut-off of iFR < 0.85 to predict 12-month graft patency, with threefold higher odds for LIMA–LAD patency (OR 3.0; 95 % CI 1.89–4.76) and 2.6-fold higher odds for venous RCA grafts (OR 2.6; 95 % CI 1.31–5.17).
Clinical outcomes were comparable between groups. The overall MACCE rate did not differ significantly at 3 years: all-cause death occurred in 8 % vs 14 %, stroke in 12 % vs 2 %, and target vessel revascularisation in 8 % vs 4 % in the iFR- and angiography-guided groups, respectively (all p > 0.05). No myocardial infarction or cardiovascular death excess was reported.
Critical reading and relevance for clinical practice
The iCABG study supports the concept that physiology-guided surgical revascularisation can refine lesion selection, reduce procedural burden, and improve graft patency without compromising safety. By identifying hemodynamically relevant lesions (iFR < 0.85) as the optimal revascularisation threshold, this approach minimises the risk of competitive flow in non-significant segments.
However, the interpretation of these findings should remain cautious. Prior randomised studies such as FARGO1 and GRAFFITI2 failed to demonstrate significant differences in graft patency or clinical outcomes between FFR-guided and angiography-guided CABG. In FARGO, graft occlusion at six months was 16 % in the FFR-guided group and 12 % in the angiography-guided group (p = 0.97), whereas in GRAFFITI, 12-month graft patency was 80 % vs 81 % (p = 0.885).
Similarly, no differences in MACCE were observed in either trial. A recent meta-analysis by Maznyczka et al.3 concluded that while physiology-based lesion assessment is well established in PCI, its translation to CABG remains less supported by evidence, given that surgical outcomes are influenced by multiple factors including conduit type, target vessel size, flow competition, and anastomotic quality.
The iCABG results diverge from prior FFR-based studies, possibly because iFR is performed in the resting wave-free period, eliminating the need for hyperemia and potentially providing a more stable measure of physiological relevance. Nonetheless, limitations remain: single-center design, modest sample size, partial completion of 36-month imaging, and lack of invasive angiographic confirmation.
From a clinical perspective, the study offers a pragmatic insight: incorporating physiology into surgical planning may help avoid unnecessary grafts and enhance long-term durability, particularly in complex multivessel disease. Yet, large multicenter studies are required to confirm whether this physiological approach should become standard in CABG decision-making.
References
- Thuesen AL et al. Fractional Flow Reserve Versus Angiographically-Guided Coronary Artery Bypass Grafting. J Am Coll Cardiol. 2018; 72(22):2732–2743. doi: 10.1016/j.jacc.2018.09.043.
- Toth GG et al. Graft Patency After FFR-Guided Versus Angiography-Guided Coronary Artery Bypass Grafting: The GRAFFITI Trial. EuroIntervention. 2019; 15(11):e999–e1005. doi: 10.4244/EIJ-D-19-00463.
- Maznyczka AM et al. Fractional Flow Reserve Versus Angiography-Guided Management of Coronary Artery Disease: A Meta-Analysis of Contemporary Randomised Controlled Trials. J Clin Med. 2022; 11(23):7092. doi: 10.3390/jcm11237092.




No comments yet!