One-year outcomes of blinded physiological assessment of residual ischemia after successful PCI - DEFINE PCI trial
Selected in JACC: Cardiovascular Interventions by M. Pighi , S. Fezzi
The objective of this analysis was to evaluate the impact of residual ischemia detected by post-PCI iFR on clinical outcomes and on residual-angina at the 12-month follow-up of the DEFINE PCI study.
References
Authors
Manesh R. Patel, Allen Jeremias, Akiko Maehara, Mitsuaki Matsumura, Zixuan Zhang, Joel Schneider, Kare Tang, Suneel Talwar, Koen Marques, Nicolas W. Shammas, Luis Gruberg, Arnold Seto, Habib Samady, Andrew S.P. Sharp, Ziad A. Ali, Gary Mintz, Justin Davies, Gregg W. Stone
Reference
J Am Coll Cardiol Intv. 2022 Jan, 15 (1) 52–61
Published
January, 10th 2022
Link
Read the abstract
Reviewers
Our Comment
Why this study – the rationale/objective?
Suboptimal physiological result despite successful angiographic PCI is common (20-30 %) and may have an impact on clinical events.
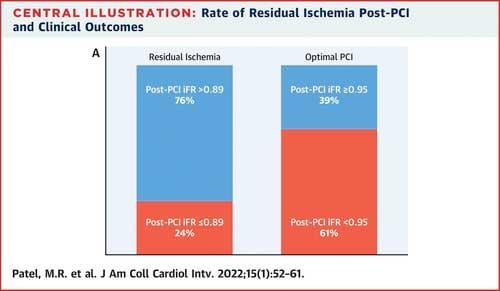
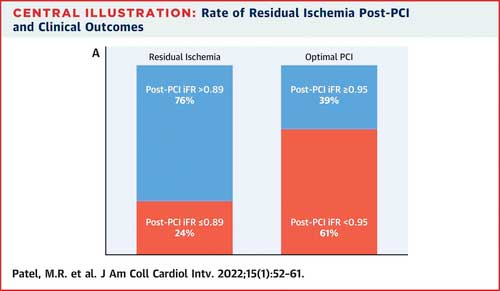
DEFINE PCI (Physiologic Assessment of Coronary Stenosis Following PCI) was a multicenter, prospective, observational study aiming to define the incidence and the characteristics of post-PCI iFR pullback defined suboptimal results. The primary endpoint of the study showed 24.0 % of patients had residual ischemia (iFR ≤ 0.89) after successful PCI, with 81.6 % of cases attributable to angiographically inapparent focal lesions.
Whether some retrospective and prospective analyses showed a relationship between post-PCI FFR and clinical outcomes, mainly vessel-oriented, similar evidence on post-PCI instantaneous wave-free ratio (iFR) is still limited.
The objective of this analysis was to evaluate the impact of residual ischemia detected by post-PCI iFR on clinical outcomes and on residual-angina at the 12-month follow-up of the DEFINE PCI study.
How was it executed? - the methodology
- DEFINE PCI was a prospective, single-arm, blinded, observational, multicenter study
- Blinded iFR pullback was performed after angiographically successful PCI in 562 vessels in 500 patients. Post-PCI iFR pullback amenable for core-lab analysis was available in 467 patients (520 vessels).
- Included patients presented with angina with either multivessel (or multiple lesions) coronary artery disease with an abnormal baseline iFR.
- As a post hoc analysis, ROC analysis was performed, defining 0.95 as the optimal post-PCI iFR cut-off value to predict events, derived using the Youden index.
What is the main result?
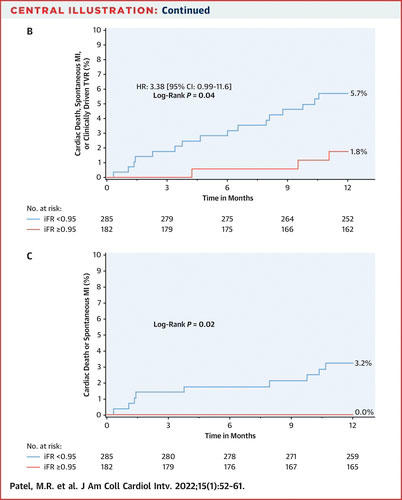
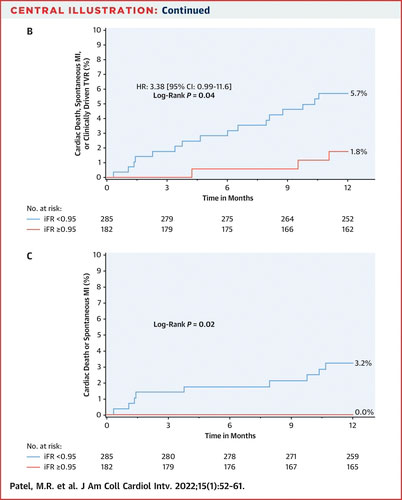
- Post-PCI iFR ≥ 0.95 (182/467 [39 %]) was associated with a significant reduction MACE compared with post-PCI iFR < 0.95 (1.8 % vs. 5.7 %; P = 0.04), driven by a reduction of MI and cardiac death.
- In highly symptomatic patients (SAQ-AF≤60), an increase of at least 10 points was more frequent in patients with residual iFR ≥ 0.95 (100.0 % vs. 88.5 %; P = 0.01).
Source = JACC: Cardiovascular Interventions
Source = JACC: Cardiovascular Interventions
Critical reading and the relevance for clinical practice
This report builds up the evidence on the importance of post-PCI physiological evaluation in stratifying the risk for further clinical events and residual symptoms. On the one side, post-PCI iFR ≥ 0.95 was related to a reduced incidence of major adverse cardiac events, driven by MI and cardiac death, and on the other, it was also related to a significant improvement in symptoms at the 12-month follow-up.
To date, physiology evaluation after apparently successful angio-guided PCI remains underused (less than 10 %), mainly due to technical and economic reasons, prolonging procedural times, and requiring the administration of hyperemic agents when FFR is performed. However, suboptimal physiological results are observed in up to 30 % of the cases, with LAD localization, low baseline FFR, and the presence of diffuse disease associated with an increased risk.
Combined physiology-intracoronary imaging studies have outlined several stent-related factors, such as geographical miss of the plaque, stent malapposition, under expansion, major edge dissections, as well as plaque or thrombus in-stent prolapse, are prone to a residual physiological impairment following PCI.
However, besides several retrospective analyses, only a few prospective studies (FFR-SEARCH, HAWKEYE trial) are available and have suggested a significant relationship between post-PCI physiology and clinical outcomes, mainly related to vessel-oriented outcomes. Overall, post-PCI evaluation should be acknowledged as safe and feasible.
Interestingly, the DEFINE-PCI study suggested that post-PCI iFR < 0.95, besides being a common finding (> 60 %), significantly impacts clinical outcomes and residual angina. In this view, the DEFINE-PCI study has paved the way for further trials aiming to tailor the physiological-based intervention even on symptoms relief. In the ORBITA trial, a significant interaction was detected between PCI-derived improvement of ischemia and pre-randomization higher stress echocardiography score, lower FFR/iFR values, and focal pattern of disease.
In this view, the pressure pullback seems to represent a key tool in defining the underlying problem and the consequent possible need for an intervention.
Moreover, in the iFR GRADIENT registry, iFRpred showed a strong linear relationship with iFRobs. The iFR pullback, compared to angiography-based strategy, led to the change of the revascularization strategy in one out of three cases, with the reduction of lesion number and length. Overall, in the case of diffuse disease, it is unlikely that further interventions would provide improvement in the physiological result, as the use of long stents could increase the risk for stent-restenosis and side-branch occlusion.
One of the main reasons that may have limited post-PCI physiology penetration into the catheterization laboratory routine was the lack of randomized prospective trials. However, in the 1:1 randomized TARGET-FFR trial, a physiology-guided incremental optimization strategy, even without showing a significant increase in the proportion of patients with a final FFR > 0.90, showed a reduction in the proportion of patients with a final FFR < 0.80.
To overcome such limitations, non-hyperemic pressure indexes and angiography-derived ones (iFR, QFR, FFRangio, and vFFR) may offer additional information to define the exact location and mechanism of suboptimal post-PCI physiology results, and, thus, leading to a patient-tailored treatment (i.e., conservative medical therapy or additional PCI).
References
- Kikuta Y, Cook CM, Sharp ASP, et al (2018) Pre-Angioplasty Instantaneous Wave-Free Ratio Pullback Predicts Hemodynamic Outcome In Humans With Coronary Artery Disease: Primary Results of the International Multicenter iFR GRADIENT Registry. JACC Cardiovasc Interv 11:757–767.
- Scarsini R, Fezzi S, Pesarini G, et al. Impact of physiologically diffuse versus focal pattern of coronary disease on quantitative flow reserve diagnostic accuracy. Catheter Cardiovasc Interv 2021; : 1–10
- Jeremias A, Davies JE, Maehara A, et al. Blinded Physiological Assessment of Residual Ischemia After Successful Angiographic Percutaneous Coronary Intervention: The DEFINE PCI Study. JACC Cardiovasc Interv 2019; 12: 1991–2001.
- Ding D, Huang J, Westra J, et al (2021) Immediate post-procedural functional assessment of percutaneous coronary intervention: current evidence and future directions. Eur Heart J 353:1–16
- Biscaglia S, Uretsky B, Barbato E, et al (2021) Invasive Coronary Physiology After Stent Implantation. JACC Cardiovasc Interv 14:237–246.
- Biscaglia S, Tebaldi M, Brugaletta S, et al. Prognostic Value of QFR Measured Immediately After Successful Stent Implantation: The International Multicenter Prospective HAWKEYE Study. JACC Cardiovasc Interv 2019; 12: 2079–88.
- Van Zandvoort LJC, Masdjedi K, Witberg K, et al. Explanation of postprocedural fractional flow reserve below 0.85: A comprehensive ultrasound analysis of the FFR SEARCH registry. Circ Cardiovasc Interv 2019; 12: 1–10.
- Diletti R, Masdjedi K, Daemen J, et al. Impact of Poststenting Fractional Flow Reserve on Long-Term Clinical Outcomes: The FFR-SEARCH Study. Circ Cardiovasc Interv 2021; : 314–22.
- Damien Collison, Matthaios Didagelos, Muhammad Aetesam-ur-Rahman et al. Post-stenting fractional flow reserve vs coronary angiography for optimization of percutaneous coronary intervention (TARGET-FFR), European Heart Journal, Volume 42, Issue 45, 1 December 2021, Pages 4656–4668.







No comments yet!