Balloon lithotripsy added to conventional preparation before stent implantation in severely calcified coronary lesions
Selected in JACC: Cardiovascular Interventions by N. Ryan
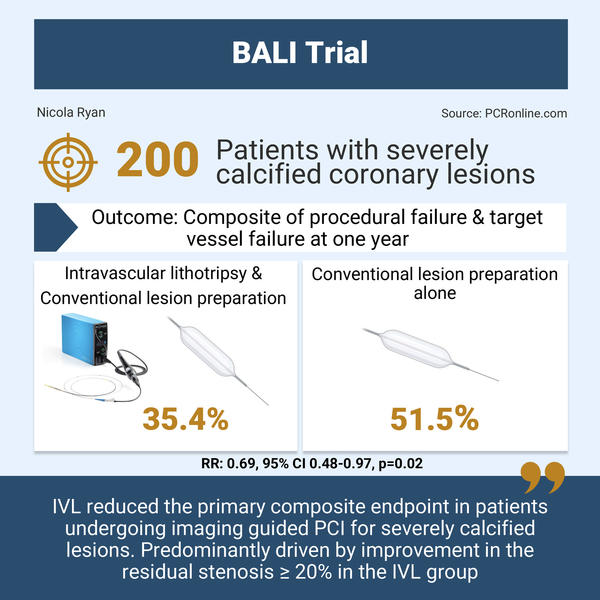
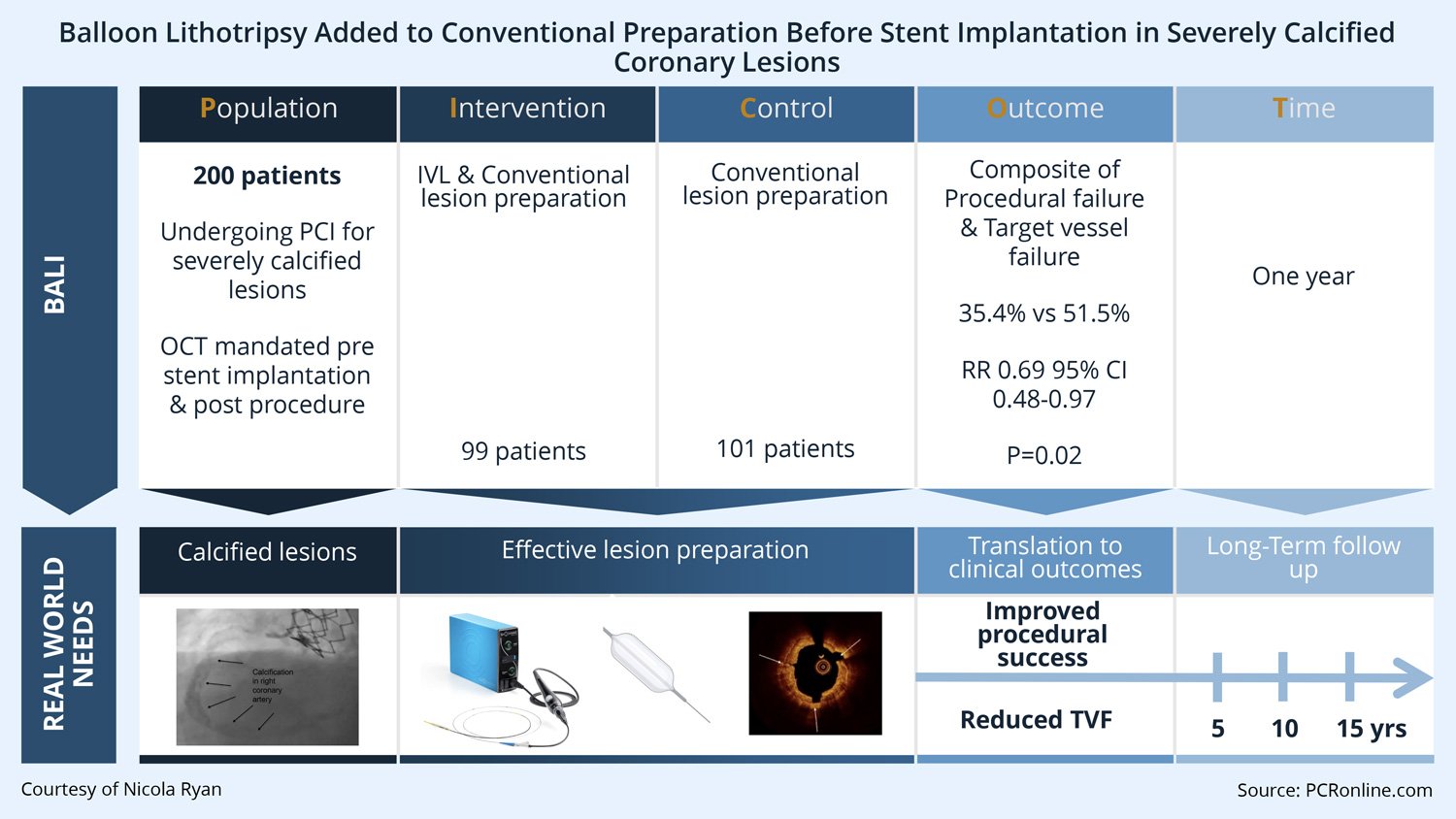
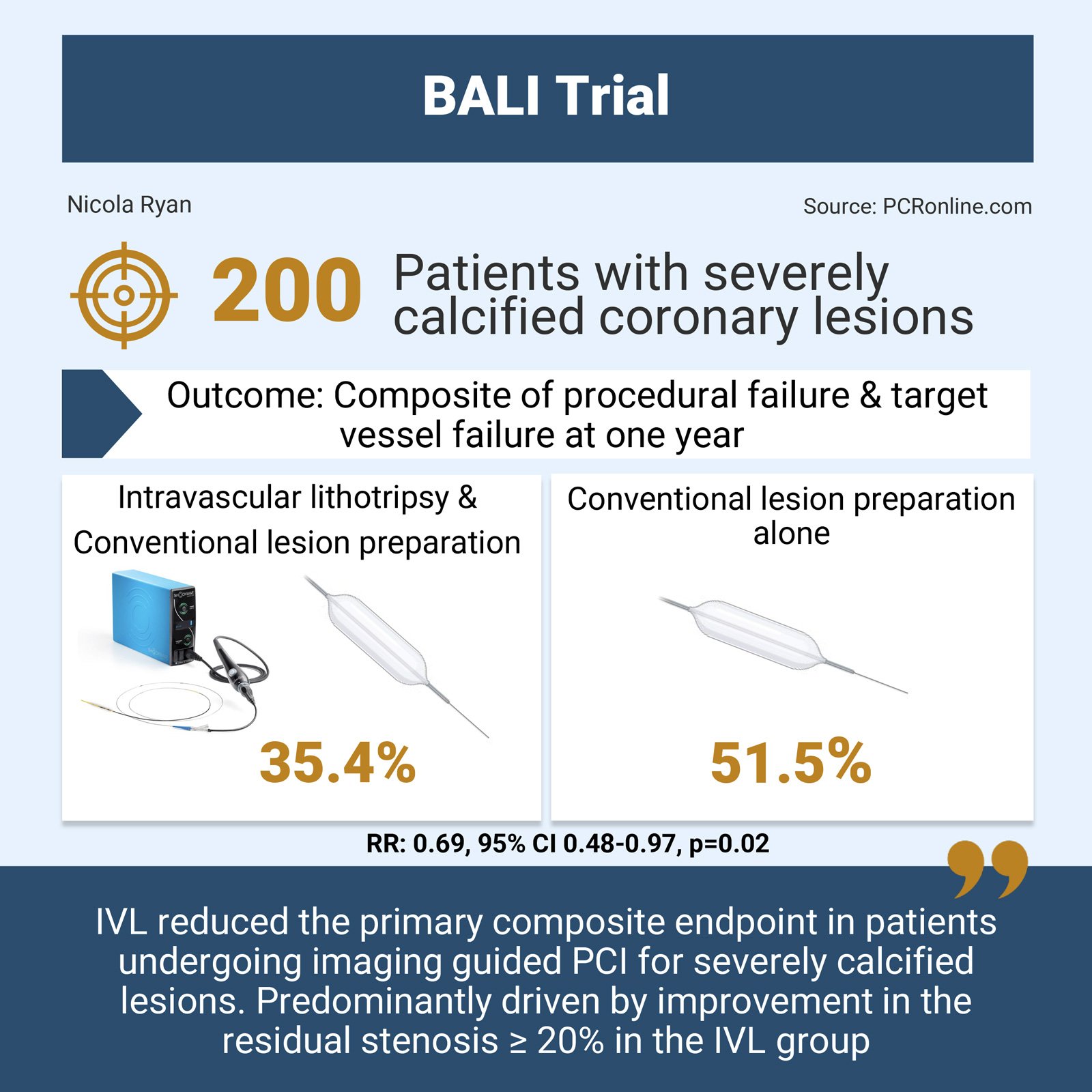
In patients with severely calcified coronary lesions undergoing PCI, the BALI trial evaluated the benefit of the addition of intravascular lithotripsy to conventional lesion preparation on the composite endpoint of procedural failure and target vessel failure.
References
Authors
Andreas T. Kristensen, Evald H. Christiansen, Niels R. Holm, Henning Kelbæk, Thomas Engstrøm, Karsten Veien, Bent Raungaard, Ola Kleveland, Johan Bennett, Peep Laanmets, Lars Jakobsen, Ole Havndrup, Jacob T. Lønborg, Ole Ahlehoff, Allan Iversen, Anil K. Vatwani, Nicolaj B. Støttrup, Lisette O. Jensen, Martin K. Christensen, Sune A. Haahr-Pedersen, Mette G. Charlot, Erin E. Gabriel, and Niels T. Olsen
Reference
JACC: Cardiovascular Interventions - Preprint - Just accepted
Published
19 December 2025
Link
Read the abstractReviewer
Latest contributions
Balloon lithotripsy added to conventional preparation before stent implantation in severely calcified coronary lesions Impact of pullback pressure gradient on clinical outcomes after percutaneous coronary interventions Validation of intravascular ultrasound-defined optimal stent expansion criteria for favorable 1-year clinical outcomesMy Comment
Designed by: Nicola Ryan - Source: PCRonline.com
Why this study – the rationale/objective?
Coronary calcium is associated with increased procedural complications and poorer clinical outcomes in patients undergoing PCI. Calcium can lead to inability to deliver equipment including stents, with inadequate lesion preparation increasing the risk of stent under-expansion and malapposition, and, as a consequence, clinical outcomes.
Several techniques, both atherectomy and balloon-based, are available for calcium modification with intravascular lithotripsy, delivering high frequency pressure waves to fracture calcified plaques.
The BALI trial was designed to determine if the addition of IVL to conventional lesion preparation is superior to conventional lesion preparation alone in patients undergoing OCT guided PCI in severely calcified coronary lesions.
How was it executed? The methodology
Patients undergoing PCI for severely calcified coronary lesions presenting with CCS or NSTE-ACS were randomised to IVL & conventional lesion preparation or conventional lesions preparation alone.
Severe calcification was defined as at least one of angiography: radiopacities visible on both sides of the vessel wall on cine images before contrast injection in > 1 projection, OCT: calcium arc > 180°, thickness > 0.5 mm, longitudinal length > 5 mm, IVUS > 270°. Key exclusion criterial included unprotected LMS, CTOs, bifurcation lesions with expected 2-stent technique, LVEF < 35 %, eGFR < 30 mL/min/1.73 m2.
In the IVL group, the Shockwave C2 or C2+ intravascular lithotripsy catheter was used as early as possible during then procedure sized 1:1 to the reference diameter. In the conventional group, semi-compliant, non-compliant, cutting, scoring and high-pressure balloons were permitted at the operators discretion. Rotational atherectomy was allowed in both groups for uncrossable lesions, if a 1:1 angiographic balloon expansion could not be achieved, or if a stent could not be delivered. OCT pullback was mandated immediately prior to stent implantation, and the end of the procedure.
- The primary endpoint was a composite of procedural failure (failed or no stent delivery or in-stent residual are stenosis ≥ 20 % assessed by OCT) or target vessel failure (cardiac death, target vessel MI or clinically driven target vessel revascularisation) at one year.
- Secondary endpoints included:
- Composite of cardiac death, any MI or stroke at one year
- Procedural complication (periprocedural MI, flow limiting dissection or perforation)
- Minimal stent expansion
- In-stent late lumen loss assessed on OCT at one year
What is the main result?
Courtesy of Nicola Ryan - Source: PCRonline.com
From January 2020 to September 2023, 200 patients were included in the trial, 99 randomised to IVL and 101 randomised to conventional lesion preparation. The majority, 76 %, were men, with a mean age of 74 years, with CCS, the indication for intervention in 78 % of cases. Rotational atherectomy was common in both groups (IVL 31.3 %, conventional 41.6 %) with the majority of lesions post dilated.
- The primary endpoint was lower in the IVL group 35.4 % vs 51.5 % (RR 0.69, 95 % CI 0.48-0.97, p = 0.02)
- In-stent residual area stenosis ≥ 20 % was numerically lower in the IVL group 32.3 % vs. 44.6 % (RR 0.73, 95 % CI 0.49-1.04)
- Target vessel failure was numerically higher in conventional group 4.0 % vs. 10.9 %, (RR 0.37, 95 % CI 0.07-1.09)
- There was no difference in the composite of cardiac death and MI or stroke between groups at 1 year (5.1 % IVL vs. 6.9 % conventional, RR 0.73, 95 %CI 0.22-2.29, p = 0.79)
- At one-year follow-up, there was no difference between groups in OCT parameters:
- In-stent late lumen loss 1.6 ± 1.7 mm2 vs. 1.6 ± 2.0 mm2 (effect estimate -0.1, 95 % CI -0.7 – 0.6)
- In-segment area stenosis 42.6 ± 18.7 % vs. 43.1 ± 18.6 % (effect estimate -0.5, 95 % CI -6.3 – 5.3)
- In-segment area stenosis ≥ 50 % 29.3 % vs. 26.6 % (effect estimate 1.1, 95 % CI 0.64 – 1.9)
- In-segment minimal luminal area 5.2 ± 2.5 mm2 vs. 5.0 ± 2.4 mm2 (effect estimate 0/2, 95 % CI -0.6 – 1.0)
Critical reading and the relevance for clinical practice:
The results of the BALI trial shows that the addition of IVL to conventional lesion preparation reduced the composite endpoint of procedural failure or target vessel failure at one year. The reduction in the composite endpoint was predominantly driven by a numerically lower rate of a residual area stenosis ≥ 20 % on OCT in the IVL group.
Importantly, the BALI trial mandated OCT immediately prior to stent implantation, and at the end of the procedure. Patients were followed with angiography and OCT at one year, though clinical endpoints were collected prior to follow-up angiography. Though not powered for clinical outcomes, the improved primary outcome did not translate to improved clinical outcomes in the IVL group. Overall, the complication rate was low and whilst numerically higher in the IVL group did not appear to be directly related to the device.
There are several explanations as to the lack of difference in the one year OCT findings as well as clinical outcomes in the BALI trial beyond simple underpowering. The MSA in BALI was large in both arms (8.7 ± 2.8 mm2 in the IVL group, 8.0 ± 2.4 mm2 in the conventional group), which is a predictor of improved clinical outcomes. Similarly, there were no differences in calcium fractures on OCT prior to stent implantation between the IVL and conventional group suggesting a similar level of lesion preparation. In the conventional group, there was a high usage of both cutting or scoring balloons (57.4 %) and rotational atherectomy, which likely contributed to the high MSA achieved in this arm.
There is a number of important limitations to consider in the BALI trial, including the fact that the primary endpoint is primarily driven by an immediately post-procedural imaging outcome. This outcome did not appear to translate to significant changes in the imaging endpoints at the one-year follow-up OCT. It would be of interest to understand the number of OCT runs carried out during the procedures and the modifications made based on the imaging data.
An important question to be asked based on the BALI trial is whether the calcium modification device or the use of intra-coronary imaging influences the outcome. The ECLIPSE trial demonstrated that, in patients with calcified coronary lesions and equipoise for the use of orbital atherectomy or conventional balloon angioplasty, orbital atherectomy did not improve MSA or TVF at one-year follow-up1. However, whilst only hypothesis-generating analysis by use or not of intracoronary imaging demonstrated that intravascular imaging was associated with a 26 % risk reduction in TVF irrespective of technique used2.
The results of the BALI trial suggest the IVL is a safe and efficacious. The systematic use of intracoronary imaging, along with adequate plaque preparation, likely contributed to the lack of long-term difference in either OCT or clinical outcomes between groups. In clinical practice, a strategy of careful assessment of plaque characteristics and choosing the most appropriate tool/s to achieve optimal plaque preparation prior to implantation of stents is likely of give the best long term outcomes in calcified coronary lesions.
References
- In severely calcified lesions eligible for both treatment strategies (ECLIPSE): a multicentre, open-label, randomised trial - The Lancet. [cited 2026 Jan 3]
- Intravascular Imaging vs Angiography Guidance for PCI of Severely Calcified Lesions: The ECLIPSE Trial | JACC: Cardiovascular Interventions. [cited 2026 Jan 3]





No comments yet!