07 Jan 2026
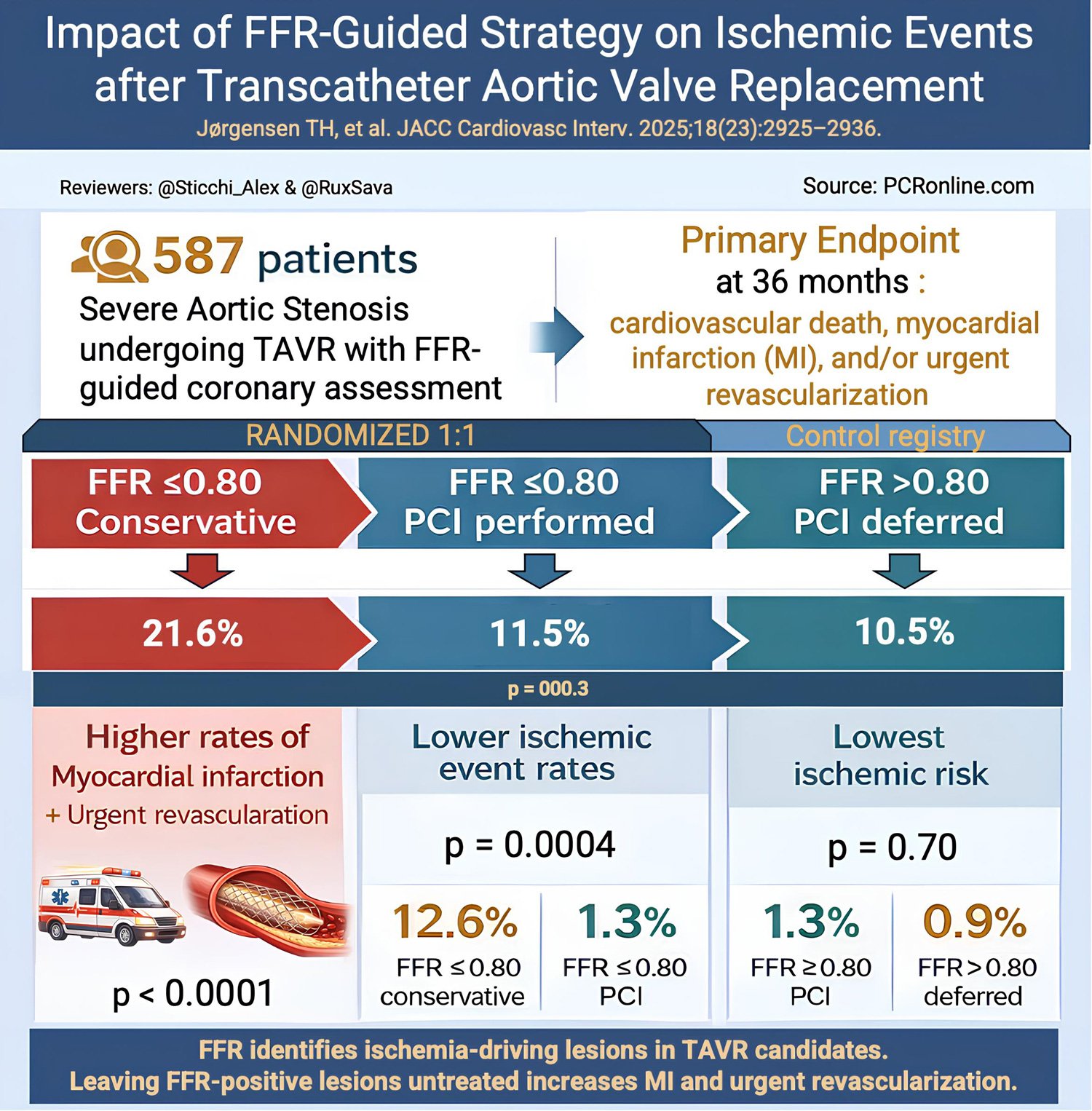
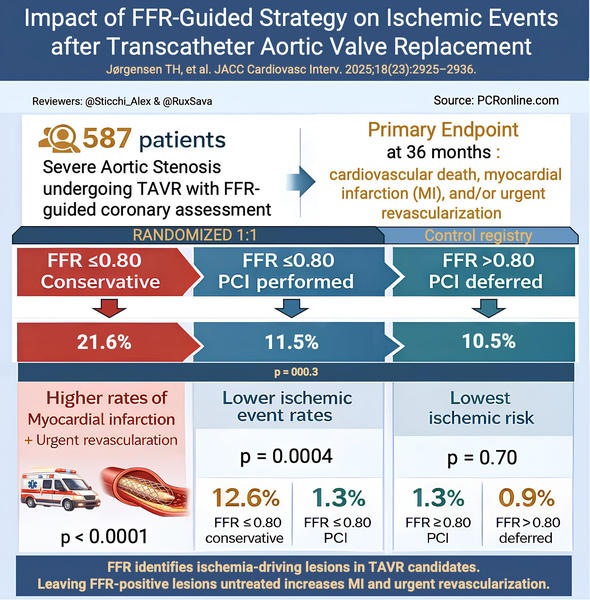
Fractional flow reserve to guide revascularisation in patients with coronary artery disease undergoing TAVR
Selected in JACC: Cardiovascular Interventions by R. Sava , A. Sticchi
The present analysis compared major adverse cardiac events in patients with significant coronary stenosis (FFR ≤ 0.80 or visual stenosis ≥ 90 %) versus those with non-significant stenosis (FFR > 0.80).
References
Authors
Troels Højsgaard Jørgensen, Thomas Engstrøm, Reza Jabbari, Charlotte Glinge, Muhammed Sabbah, Karsten Tange Veien, Matti Niemela, Phillip Freeman, Rickard Linder, Rikke Sørensen, Lene Holmvang, Dan Ioanes, Christian Juhl Terkelsen, Julia Ellert-Gregersen, Evald Christiansen, Ashkan Eftekhari, Jarkko Piuhola, Olli Kajander, Sasha Koul, Mikko Savontaus, Pasi Karjalainen, Lars Søndergaard, Ole De Backer, and Jacob Lønborg
Reference
JACC: Cardiovascular Interventions - Volume 18, Number 23 - 2925-2936
Published
8 December 2025
Link
Read the abstractReviewers
Our Comment
Reviewers: @Sticchi_Alex & @RuxSava - Source: PCRonline.com
Why this study – the rationale/objective?
Coronary artery disease (CAD) frequently coexists with severe aortic stenosis (AS), and its management in patients undergoing transcatheter aortic valve replacement (TAVR) remains a major clinical challenge. Fractional flow reserve (FFR) is the reference standard for physiological assessment of coronary lesions in stable CAD2–4. However, the reliability of measuring FFR and RFR in patients with severe AS has been a matter of debate. Alterations in microvascular resting and hyperemic pressures related to increased myocardial mass and end-diastolic LV pressure have been shown to impact real-life pre and post-AVR coronary physiology testing5.
The NOTION-3 trial and registry were designed to address this gap by evaluating whether FFR-guided coronary revascularisation using the 0.80 threshold improves long-term clinical outcomes in TAVR candidates6.
The present analysis specifically compared major adverse cardiac events in patients with significant coronary stenosis (FFR ≤ 0.80 or visual stenosis ≥ 90 %) versus those with non-significant stenosis (FFR > 0.80).
How was it executed? The methodology
Study design
This is a post-hoc analysis of the NOTION-3 randomised controlled trial (RCT)6 and registry. For an in-depth analysis of the main RCT, please consult the previous Journal Club review7.
Patients with severe AS and a coronary artery stenosis measuring ≥ 50 % in arteries measuring at least 2.5 mm diameter were considered for inclusion. FFR was measured in all patients with stenosis between 50-90 %. Patients with functionally significant disease, defined as FFR ≤ 0.80 or angiographically severe stenosis (≥ 90 %), were randomised 1:1 to PCI or conservative management. Patients with FFR > 0.80 were not randomised nor revascularised, and were included in a registry cohort. Acute coronary syndromes, left main lesions and patients with more than one chronic total occlusion were excluded6.
Study endpoints
The primary endpoint was the composite risk for cardiovascular mortality, myocardial infarction, or need for urgent revascularisation (defined as unplanned revascularisation in the setting of an acute coronary event).
The secondary endpoints were the individual components of the primary endpoint as well as any elective coronary revascularisation.
For the purpose of the analysis, patients were stratified into three groups: FFR ≤ 0.80 treated conservatively; FFR ≤ 0.80 treated by PCI; and FFR >0.80 treated conservatively (defer group).
What is the main result?
A total of 587 patients were included in the as-treated population: 232 participants in the FFR ≤ 0.80 conservative group, 220 in the FFR ≤ 0.80 PCI group, and 214 in the FFR >0.80 defer group.
At 36 months, the cumulative incidence of the primary composite endpoint was significantly higher in patients with FFR ≤ 0.80 managed conservatively compared with those treated with PCI and those with FFR > 0.80 in whom PCI was deferred (21.6 % vs 11.5 % vs 10.5 %; p = 0.003).
The excess risk in the conservative FFR-positive group was driven by significantly higher rates of myocardial infarction (6.9 % vs 13.5 %, HR 0.2, 95 % CI 0.08-0.6, P = 0.004) and urgent revascularisation (2.3 % vs 10.4 %, HR 0.2, 95 % CI 0.09-0.6, P = 0.002). Cardiovascular mortality alone did not differ significantly between groups.
Outcomes were similar between PCI-treated FFR-positive lesions and deferred FFR-negative lesions.
At the coronary segment level, untreated FFR ≤ 0.80 lesions showed a markedly higher incidence of subsequent revascularisation compared with PCI-treated FFR-positive segments and deferred FFR-negative segments (12.6 % vs 1.3 % vs 0.9 %; p < 0.0001).
Critical reading and the relevance for clinical practice:
The NOTION-3 study provides the strongest outcome-based evidence to date supporting the use of coronary physiology to guide revascularisation in patients with severe AS undergoing TAVR. It showed that an FFR ≤ 0.80 or severe stenosis ≥ 90 % identifies patients who benefit from revascularisation versus those who can be safely deferred.
As highlighted in the accompanying editorial, angiographic severity alone is an insufficient surrogate for ischemic burden and prognosis in the TAVR population8. The current substudy demonstrated that PCI of FFR-positive lesions reduces event rates to levels comparable with those observed in patients with FFR-negative disease, while deferral of PCI in FFR-negative lesions appears safe, mirroring decades of evidence from stable CAD populations2–4.
A major strength of the study is the consistency of results across patient-level and lesion-level analyses, reinforcing their biological plausibility. The excess risk associated with conservative management of FFR-significant lesions was not limited to repeat revascularisation but extended to spontaneous myocardial infarction, suggesting that untreated ischemic burden in patients with severe AS is not a benign condition.
A critical issue concerns the optimal FFR threshold in patients with severe aortic stenosis. Previous physiological studies have suggested higher cut-offs, such as 0.83, based on ischemia detected by SPECT imaging5. However, SPECT has limited concordance with invasive physiology, and the impact of severe aortic stenosis on its diagnostic performance remains uncertain9. NOTION-3 supports the pragmatic use of the conventional 0.80 threshold, particularly at the extremes of physiological severity, while acknowledging that the ideal binary cut-off for predicting hard clinical events in this population remains undefined.
Several limitations should be considered. First, this is a post-hoc analysis combining RCT data with registry data. Further bias may also have been introduced by the change in primary outcome between the original study and the present study, with all-cause mortality replaced by cardiovascular death. It is also unclear how many stenosis were considered as significant based on FFR or > 90 % diameter stenosis alone. Moreover, the open-label design may have influenced decisions regarding repeat or urgent revascularisation, particularly in patients known to have a low pre-TAVR FFR. Nevertheless, the persistence of a higher myocardial infarction rate in the conservatively managed FFR-positive group argues against this signal being explained solely by ascertainment bias. It should also be noted that most enrolled patients had low complexity of coronary artery disease (median Syntax score of 9), thus the results cannot be readily extrapolated to more complex CAD.
The study findings are aligned with the 2025 ESC/EACTS Guidelines on the management of valvular heart disease, which recommend a selective rather than routine approach to coronary revascularisation in TAVR candidates. The guidelines state that PCI should be considered in patients with severe AS undergoing TAVI who have high-grade coronary stenoses in large proximal vessels10.
The FAI-TAVI trial further supports this conceptual framework by prospectively testing a physiology-guided versus angiography-guided revascularisation strategy in TAVI candidates. Although outcome data are still awaited, FAI-TAVI reinforces the need for a nuanced, physiology-based approach rather than systematic revascularisation11.
The NOTION-3 study supports a clear approach in TAVR candidates: PCI should be strongly considered for patients with severe stenosis or FFR < 0.80, whereas it can be safely deferred for intermediate stenosis with FFR > 0.80. Routine conservative management of FFR-positive lesions should be avoided, as it is associated with major adverse cardiovascular events. Finally, as the study does not clarify the optimal timing of PCI relative to TAVR, decisions should remain individualised, integrating coronary anatomy, physiology, and the estimated feasibility of coronary access after TAVR.
References
- Jørgensen TH, Engstrøm T, Jabbari R, et al. Fractional Flow Reserve to Guide Revascularization in Patients With Coronary Artery Disease Undergoing TAVR. JACC Cardiovasc Interv. 2025;18:2925–36.
- Tonino PAL, De Bruyne B, Pijls NHJ, et al. Fractional Flow Reserve versus Angiography for Guiding Percutaneous Coronary Intervention. N Engl J Med. 2009;360:213–24.
- De Bruyne B, Fearon WF, Pijls NHJ, et al. Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med. 2014;371:1208–17.
- Zimmermann FM, Ferrara A, Johnson NP, et al. Deferral vs. performance of percutaneous coronary intervention of functionally non-significant coronary stenosis: 15-year follow-up of the DEFER trial. Eur Heart J. 2015;36:3182–8.
- Minten L, McCutcheon K, Vanhaverbeke M, et al. Coronary Physiological Indexes to Evaluate Myocardial Ischemia in Patients With Aortic Stenosis Undergoing Valve Replacement. JACC Cardiovasc Interv. 2025;18:201–12.
- Lønborg J, Jabbari R, Sabbah M, et al. PCI in Patients Undergoing Transcatheter Aortic-Valve Implantation. New England Journal of Medicine. 2024;391(23):2189-2200. doi:10.1056/NEJMoa2401513
- PCR. NOTION-3 - Percutaneous coronary intervention in patients undergoing transcatheter aortic valve implantation. Accessed December 28, 2025.
- Minten L. FFR-Guided Revascularization in Aortic Stenosis: A New Angle on an Old Question. JACC Cardiovasc Interv. 2025;18:2937–40.
- Danad I, Szymonifka J, Twisk JWR, et al. Diagnostic performance of cardiac imaging methods to diagnose ischaemia-causing coronary artery disease when directly compared with fractional flow reserve as a reference standard: a meta-analysis. Eur Heart J. 2017;38:991–8.
- Praz F, Borger MA, Lanz J, et al. ESC/EACTS Scientific Document Group. 2025 ESC/EACTS Guidelines for the management of valvular heart disease. Eur J Cardiothorac Surg. 2025;67:4635–736.
- Ribichini FL, Scarsini R, Pesarini G, et al. Physiology vs angiography-guided percutaneous coronary intervention in transcatheter aortic valve implantation: the FAITAVI trial. EuroIntervention. 2024;20:e504–e510.