13 Apr 2022
Randomized clinical trial on prevention of radial occlusion after transradial access using nitroglycerin: PATENS Trial
Selected in JACC: Cardiovascular Interventions by E. Asher
The aim of the current study was to evaluate whether administration of nitroglycerin at the beginning or end of a trans-radial approach procedure would preserve radial artery patency.
References
Authors
Roberto L. da Silva, Pedro B. de Andrade, George Dangas, Rodrigo M. Joaquim, Thaís R.W. da Silva, Ramiro G. Vieira, Vanderlei C. Pereira, Amanda G.M. Sousa, Fausto Feres, and José R. Costa
Reference
J Am Coll Cardiol Intv. Mar 21, 2022. Epublished DOI: 10.1016/j.jcin.2022.02.026
Published
21 March 2022
Link
Read the abstract
Reviewer
My Comment
Why this study – the rationale/objective?
The Trans-radial approach (TRA) is becoming the preferred vascular access for coronary interventions. Nevertheless, radial artery occlusion (RAO) is the most frequent complication.
Routine vasodilator treatment aims to reduce spasms and possibly prevent RAO. Hence, the aim of the current study was to evaluate whether administration of nitroglycerin at the beginning or end of a TRA procedure would preserve radial artery patency.
How was it executed? - the methodology
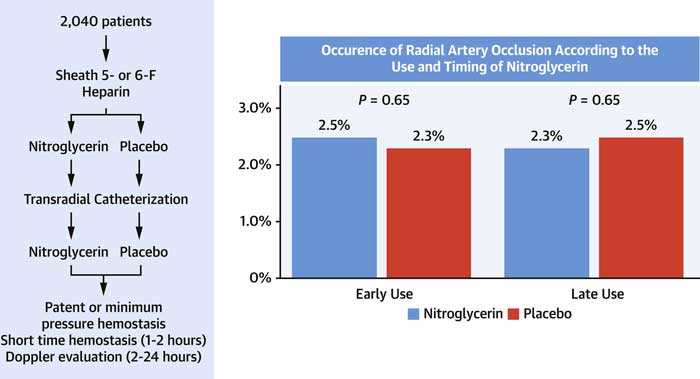
PATENS (Prevention of Radial Artery Occlusion After Transradial Access Using Nitroglycerin) was a prospective, multicenter, randomized, double-blind, 2-by-2 factorial, placebo-controlled clinical trial (between August 2017 and October 2021) comparing the superiority (reduction of RAO) between the use of intra-arterial nitroglycerin and the use of placebo before performing percutaneous procedures via TRA or before removing the sheath.
Primary objective: Reduction of RAO
- Inclusion criteria: a) clinical indications for coronary angiography or percutaneous coronary intervention (PCI) if there were trans-radial access route and the use of 5- or 6-F sheath size.
- Exclusion criteria were:
- Acute myocardial infarction;
- complications during the procedure (cardiac arrest, pulmonary edema, cardiogenic shock, and stroke);
- known allergy or intolerance to nitrates;
- medication with continuous intravenous nitrates or any nitrates within the past hour;
- and use within 24 hours before randomization of phosphodiesterase inhibitors.
Randomization:
Patients were randomized in a 1:1 ratio to nitroglycerin or a placebo in 2 Interventions just after access was obtained (nitroglycerin or placebo) and the sheath placed and before sheath removal.
Nitroglycerin was administrated at a dose of 500 µg, diluted in 10 mL saline solution (0.9 % NaCl).
The second time point of intervention was at the end of the procedure, before the removal of the hemostatic introducer. In all patients, 3 to 4 mL blood was aspirated through the sheath to remove any residual thrombus, followed by the local administration of nitroglycerin, at a same dose of 500 µg (late group), diluted in 10 mL saline solution; the control group received placebo (saline solution) (late placebo) in the same volume.
TRA technique: a total of 11 operators performed all procedures. Local subcutaneous anesthesia was applied with 1 % lidocaine at the wrist, 1 to 2 cm proximal to the styloid process of the radial bone. All arterial punctures were performed using only the palpatory method, without ultrasound use. Then, patients received heparin (5,000 U) through the radial sheath as an intra-arterial bolus. In cases of PCI, additional heparin was used (total 100 IU/kg).
After the procedure, hemostasis was achieved as follows by a staff member not aware of the randomization group.
All pneumatic wristbands were positioned and adjusted to the lowest pressure required for hemostasis. After 1 hour of continuous compression at the puncture site, after the diagnostic procedure or 2 hours postintervention, 3 mL air was removed every 15 minutes until complete deflation.
Radial patency:
Patency was evaluated using vascular duplex doppler ultrasound performed in all patients within 24 hours of the removal of the compression band, during the in-hospital stay. RAO was defined by the absence of anterograde flow. To evaluate recanalization, all patients with confirmed RAO were further assessed 30 days after the index procedure with a new duplex doppler ultrasound (US) examination.
Study endpoints:
The primary outcome was the incidence of early RAO, confirmed by the absence of antegrade flow in US, up to 24 hours after catheterization.
The secondary outcome was late RAO, among all patients with early occlusion, assessed using duplex US to detect the presence of antegrade flow 30 days after index catheterization.
What is the main result?
- Treatment groups (1,020 Patients) did not differ from the placebo group (1,020 Patients) concerning the number of puncture attempts, use of 6-F sheaths, procedural time, and puncture technique.
- There was a trend toward more radial artery spasms among those who did not receive prophylactic nitroglycerin (13.4 % vs 10.8 %; P = 0.06).
- There was a significant relationship between nitroglycerin use and hypotension (2.5 % vs 1.2 %; P = 0.03).
- A preliminary test for interaction among the factors showed no statistical significance (P = 0.665). The incidence of the primary outcome, RAO defined by US until 24 hours after catheterization, was not significantly different between nitroglycerin early use and placebo (2.5 % vs 2.3 %; P = 0.664); it was also not different between nitroglycerin late use and placebo (2.3 % vs 2.5 %; P = 0.664).
- Presence of recanalization by antegrade flow on US at 30-day follow-up was 30.6 %, with no difference between groups.
- Subgroup analysis showed no benefit from nitroglycerin use in any of the evaluated subgroups
- There was no interaction between diagnostic and therapeutic procedures in the occurrence of RAO.
- By multivariable analysis, only the presence of clinical spasm (OR: 3.53; 95 % CI: 1.87-6.66. P < 0.001) and access achieved with more than a single puncture attempt (OR: 2.58; 95 % CI: 1.43-4.66; P = 0.002) were significant independent predictors of 24-hour RAO.
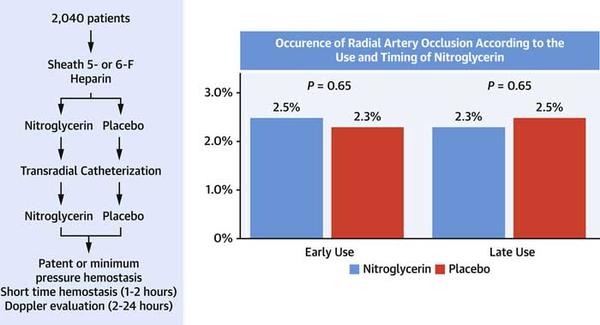
Study flowchart and primary endpoint of nitroglycerin vs placebo for radial artery occlusion prevention
Source = JACC: Cardiovascular Interventions
Critical reading and the relevance for clinical practice?
This PATENS trial shows that routine intra-arterial use of nitroglycerin does not reduce the risk for early RAO after trans-radial coronary catheterization, despite early use, at the beginning of the procedure or later before sheath removal.
Nevertheless, spasm was an independent predictor of RAO. The intra-arterial use of nitroglycerin at the beginning of the procedure shows a trend to lessen the incidence of spasm, which could facilitate the advancement and manipulation of the catheter and lower patient discomfort, without reducing RAO occurrence.
The use of nitroglycerin after placement of the introducer may have avoided injuries induced by higher contact of the catheter with the arterial wall, but it did not affect the segment covered by the sheath, which is precisely the segment in which most of the endothelial trauma occurs after the procedure, even with the use of hydrophilic coated sheaths in all cases.
Should common practice and guidelines be changed?
The study has several limitations: The RAO rate found was much lower than expected, which might affect the sample size assumptions.
Further, the study is pertinent to nitroglycerin use but not to other prophylactic anti-spasmolytic therapies. Verapamil and other medications or combinations should be tested in the future for their effect on preventing RAO. Moreover, participating centers are highly experienced with radial access and care in the hemostatic process, and the outcome may be different at centers with a broader spectrum of expertise.
The authors concluded that routine intra-arterial nitroglycerin should not be considered mandatory in RAO prevention.
-> What is your approach regarding the use of nitroglycerin to prevent RAO? Do you think one should change his/her common practice regarding the routine use of nitroglycerin in TRA?





2 comments
the use of Verapamil with the addition of a minimum dose of nitrate has a good result in normal blood pressure
In my opinion, we should not use intra-arterial nitroglycerin as routine. Its prevalence is after more than one unsuccessful puncture attempts or small caliber of the arterial lumen/diameter. Best regards from Dr..med. Santoso Adhiwana