Right ventricular-pulmonary arterial coupling and afterload reserve in patients undergoing transcatheter tricuspid valve repair
Selected in Journal of the American College of Cardiology by C. Allen , A. Duncan
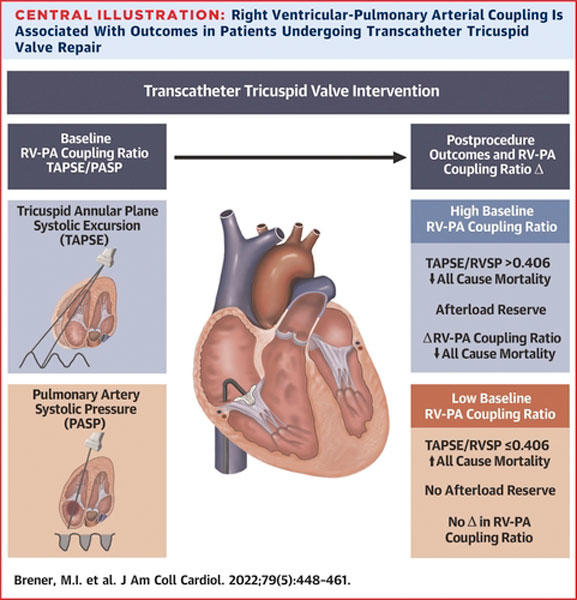
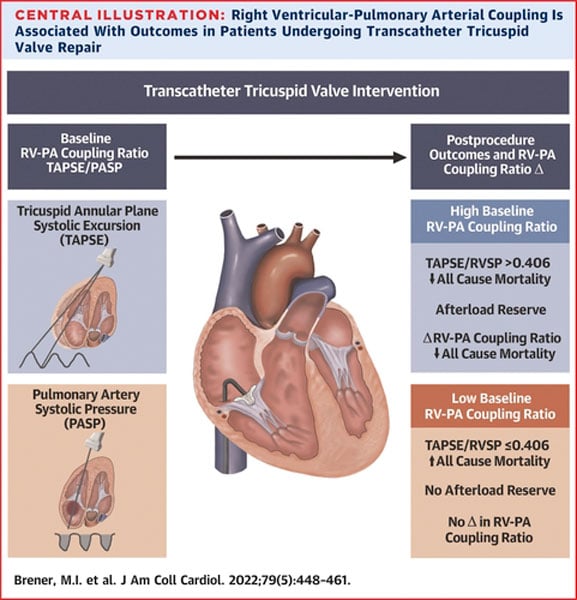
The authors hypothesized that disordered right ventricular to pulmonary artery (RV-PA) coupling may denote RV decompensation in patients undergoing transcatheter tricuspid valve repair (TTVR) that may correlate with poor clinical outcomes.
References
Authors
Michael I. Brener, Philipp Lurz, Jörg Hausleiter, Josep Rodés-Cabau, Neil Fam, Susheel K. Kodali, Karl-Philipp Rommel, Guillem Muntané-Carol, Mara Gavazzoni, Tamim M. Nazif, Alberto Pozzoli, Hannes Alessandrini, Azeem Latib, Luigi Biasco, Daniel Braun, Eric Brochet, Paolo Denti, Edith Lubos, Sebastian Ludwig, Daniel Kalbacher, Rodrigo Estevez-Loureiro, Kim A. Connelly, Christian Frerker, Edwin C. Ho, Jean-Michel Juliard, Claudia Harr, Vanessa Monivas, Georg Nickenig, Giovanni Pedrazzini, François Philippon, Fabien Praz, Rishi Puri, Joachim Schofer, Horst Sievert, Gilbert H.L. Tang, Martin Andreas, Holger Thiele, Matthias Unterhuber, Dominique Himbert, Marina Ureña Alcázar, Ralph Stephan Von Bardeleben, Stephan Windecker, Mirjam G. Wild, Francesco Maisano, Martin B. Leon, Maurizio Taramasso, and Rebecca T. Hahn
Reference
J Am Coll Cardiol. 2022 Feb, 79 (5) 448–461
Published
February 2022
Link
Read the abstract
Reviewers
Our Comment
Why this study – the rationale/objective?
Severe tricuspid regurgitation (TR) carries a poor prognosis, has an absence of effective medical therapy, and has been historically underserved by conventional surgery. Fervent recent expansion of transcatheter techniques has sought to bridge this gap, with several approaches demonstrating encouraging procedural success. However, clinical outcomes remain heterogeneous and considerable uncertainty exists over optimal patient selection, timing of intervention, and the avoidance of futile procedures.
The authors aimed to address these questions from a physiological standpoint, hypothesizing that disordered right ventricular to pulmonary artery (RV-PA) coupling may denote RV decompensation in patients undergoing transcatheter tricuspid valve repair (TTVR) that may correlate with poor clinical outcomes.
How was it executed? - the methodology
Patients at high surgical risk (n = 444, mean EuroSCORE II 10.0 ± 10.4, mean age 77 ± 9 years) undergoing TTVR were enrolled in the international multicentre TriValve registry1. The majority had functional TR (89 %) and received an edge-to-edge (83 %, MitraClip) device; with the remainder a mix of annuloplasty, spacer, and heterotopic devices.
RV-PA coupling was defined by simple echocardiographic measures, using the ratio of tricuspid annular plane systolic excursion (TAPSE) to estimated pulmonary artery systolic pressure (PASP). The primary endpoint was 1-year all-cause mortality.
What is the main result?
A baseline TAPSE/PASP ratio above the population median (> 0.406 mm/mmHg) was independently associated with decreased all-cause mortality (HR 0.57; 95 % CI: 0.35-0.93, p = 0.023).
In an exploratory sub-analysis restricted to patients in whom follow-up transthoracic echocardiography (TTE) was available (53 % original study group, taken median 41 days post-TTVR), reduction in TR by ³1+ grade was associated with a decrease in TAPSE/PASP ratio post-procedure, and (assumed to reflect increased forward flow) was also independently associated with reduced mortality at 1-year (OR 2.53; 95 % CI:1.06-6.03, p = 0.037).
Source: JACC
Critical reading and the relevance for clinical practice
The independent association between baseline RV-PA coupling and all-cause mortality in this well-conducted study provides a practical and potentially potent predictor of outcomes in patients undergoing TTVR, elegantly illustrating the clinical relevance of RV ‘afterload reserve’; a physiologically attractive concept readily derived from a standard baseline investigation (transthoracic echocardiogram).
These novel and timely findings may have important implications for patient selection in TTVR, a critical unmet need in a rapidly evolving field.
However, there are several considerations emphasised by both the study authors and accompanying editorialists2 which warrant attendant caution.
Firstly, the observational design of the TriValve registry dictates the absence of a control arm and a central core lab review of the imaging. In particular, the potential limitations of echocardiographic parameters studied within the context of severe TR (e.g. pressure gradient underestimation with laminar flow, fixed RA pressure upper limit of 15 mmHg) should be borne in mind.
More fundamentally, the compelling simplicity of resting TAPSE/PASP ratio as a surrogate of RV-PA coupling may also be a limitation – omitting conventional metrics of RV wall stress (wall thickness, chamber dimensions, and mechanics). Whether incorporation of these parameters, invasively determined haemodynamics, use of pharmacological/exercise stress, or additional information gleaned from cardiac magnetic resonance (e.g. RV late gadolinium enhancement) have the potential to refine this measure further is likely to be the focus of future work.
Lastly, the dichotomisation of the continuous TAPSE/PASP ratio variable via the median value has some statistical limitations, particularly if, as detailed by Afilalo et al, its relationship with mortality is non-linear2,3. Notably, a TAPSE/PASP ratio cut-off (0.317) defined by the more statistically robust receiver-operator curve (ROC) analysis was also associated with mortality, although the area under the curve (0.63) suggested a more modest discriminative capacity. Ultimately further work in an external validation cohort(s) is ideally required before translating these cut-offs directly into clinical decision making.
Conclusion
In this simple but elegant study, a readily derived non-invasive metric of RV-PA coupling from the baseline transthoracic echocardiogram demonstrated an association with all-cause mortality in a large cohort of patients undergoing TTVR. Further work is anticipated to develop this concept and provide refinements in objective patient selection and outcome prediction in this rapidly expanding patient cohort.
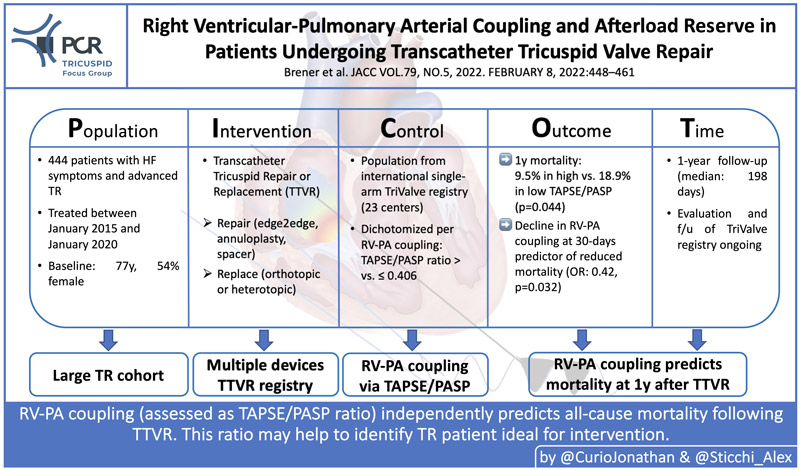
PICOT Analysis by Jonathan Curio and Alex Sticchi
References
- Brener MI, Lurz P, Hausleiter J, Rodés-Cabau J, Fam N, Kodali SK, Rommel KP, Muntané-Carol G, Gavazzoni M, Nazif TM, Pozzoli A, Alessandrini H, Latib A, Biasco L, Braun D, Brochet E, Denti P, Lubos E, Ludwig S, Kalbacher D, Estevez-Loureiro R, Connelly KA, Frerker C, Ho EC, Juliard JM, Harr C, Monivas V, Nickenig G, Pedrazzini G, Philippon F, Praz F, Puri R, Schofer J, Sievert H, Tang GHL, Andreas M, Thiele H, Unterhuber M, Himbert D, Alcázar MU, von Bardeleben RS, Windecker S, Wild MG, Maisano F, Leon MB, Taramasso M, Hahn RT. Right Ventricular-Pulmonary Arterial Coupling and Afterload Reserve in Patients Undergoing Transcatheter Tricuspid Valve Repair. Journal of the American College of Cardiology. 2022;79:448–461. Available from: https://www.jacc.org/doi/10.1016/j.jacc.2021.11.031
- Rudski LG, Afilalo J. Right Ventricle-Pulmonary Artery Coupling in Percutaneous Tricuspid Valve Repair: Is Simple Sufficient?∗. Journal of the American College of Cardiology. 2022;79:462–464. Available from: https://www.jacc.org/doi/10.1016/j.jacc.2021.11.030
- Altman DG, Royston P. The cost of dichotomising continuous variables. BMJ (Clinical research ed). 2006;332:1080. Available from: https://pubmed.ncbi.nlm.nih.gov/16675816/







No comments yet!