14 Nov 2023
The mortality burden of untreated aortic stenosis
Selected in JACC by A. Sticchi , G. Costa
This study, based on extensive real-world data, aimed to assess mortality rates across different untreated AS severities and AS treatment rates.
References
Authors
Philippe Généreux, Rahul P. Sharma, Robert J. Cubeddu, Lucy Aaron, Omar M. Abdelfattah, Konstantinos P. Koulogiannis, Leo Marcoff, Mostafa Naguib, Samir R. Kapadia, Rajendra R. Makkar, Vinod H. Thourani, Benjamin S. van Boxtel, David J. Cohen, Michael Dobbles, Glenn R. Barnhart, Michelle Kwon, Philippe Pibarot, Martin B. Leon, and Linda D. Gillam
Reference
J Am Coll Cardiol. Oct 24, 2023. Epublished DOI: 10.1016/j.jacc.2023.09.796
Published
24 October 2023
Link
Read the abstractReviewers
Our Comment

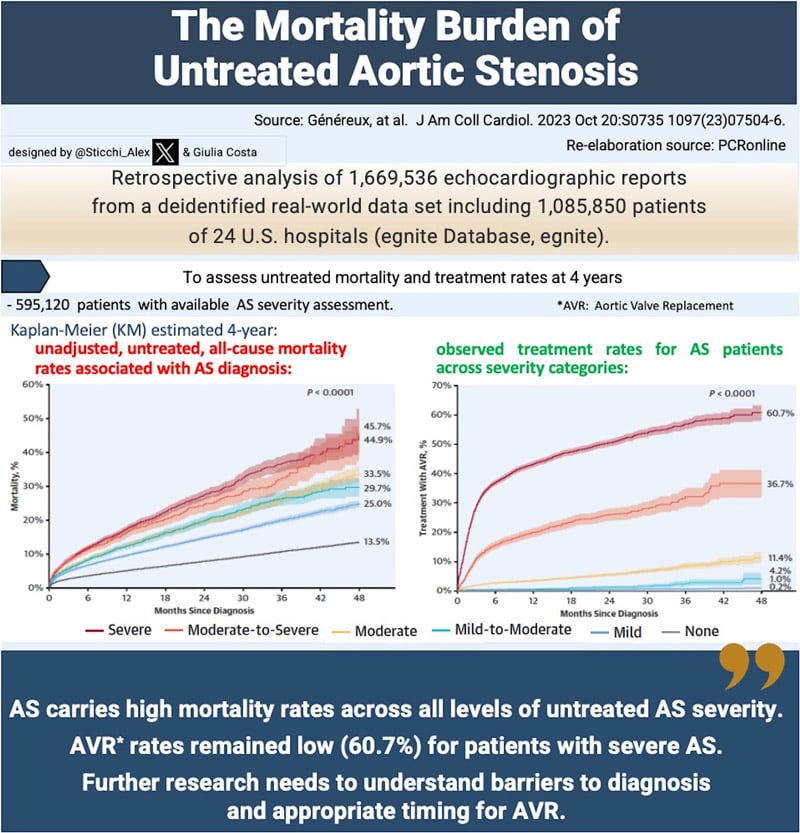
Aortic stenosis (AS) is a progressive and potentially fatal heart condition. This study, based on extensive real-world data, aimed to assess mortality rates across different untreated AS severities and AS treatment rates. The research highlighted challenges in accurately diagnosing AS severity, leading to undertreatment, and emphasized the importance of early intervention.
Why this study – the rationale/objective?
The study addresses the underappreciation of AS severity in real-world settings, leading to potential undertreatment and impacting patient prognosis. The objective is to evaluate mortality rates across various untreated AS severities using a large dataset, and to emphasize the need for early diagnosis and intervention.
How was it executed – the methodology?
The study analyzed data from 1,669,536 echocardiograms and 1,085,850 patients, classifying AS severity through American College of Cardiology / American Heart Association guidelines recommendation. Patients were followed for 4 years or until treatment, and outcomes were assessed based on AS severity. Statistical analyses, including Kaplan-Meier estimates and Cox proportional hazards regression, were performed.
What is the main result?
The study analyzed data from 595,120 patients with available aortic stenosis (AS) severity assessment, out of which 70,778 patients (11.9 %) were diagnosed with varying degrees of AS based on echocardiographic reports.
Patients with AS, especially those with more severe cases, were generally older and had a higher prevalence of concomitant diseases such as hypertension, atrial fibrillation, and coronary artery disease. Discordance in diagnostic severity of AS and the presence of echocardiographic criteria for severe AS was noted in a significant proportion of patients.
Observed 4-year mortality and treatment rates varied across severity categories:
Mortality and treatment rates AS severity associated at 4 years | ||
AS severity | Unadjusted, untreated, all-cause mortality rates associated with AS diagnosis | Observed treatment rates |
None | 13.5% | 0.2% |
Mild | 25.0% | 1.0% |
Mild-to-moderate | 29.7% | 4.2% |
Moderate | 33.5% | 11.4% |
Moderate-to-severe | 45.7% | 36.7% |
Severe | 44.9% | 60.7% |
Table drawn up by Giulia Costa and Alessandro Sticchi based on data from the article by Généreux et al.
Critical reading and the relevance for clinical practice
The study on aortic stenosis (AS) mortality rates of Généreux et al. in this issue of JACC (10.1016/j.jacc.2023.09.796), grounded in a robust real-world dataset, unveils crucial insights into the challenges faced in diagnosing and treating this progressive heart condition. The findings not only underscore the importance of accurate diagnosis, but also shed light on the complexities surrounding AS management, urging the medical community to reevaluate existing practices and adopt a more proactive approach considering the high mortality observed across the full spectrum of untreated AS severity and the low treatment rate among patients with severe AS.
Underscoring the diagnostic challenges:
One of the key takeaways from the study is the inherent difficulty in accurately determining the severity of AS in real-world settings. Discordant data, including peak velocity, mean gradient, and aortic valve area, often lead to challenges in classification. The high prevalence (13.4 %) of patients receiving "intermediate" diagnoses (mild-to-moderate or moderate-to-severe) highlights the nuanced nature of AS diagnosis. Factors such as difficult image acquisition, patient echogenicity, and variable image quality contribute to this diagnostic complexity. This dilemma necessitates re-evaluating the current diagnostic criteria, urging clinicians to upgrade patients risk profile to a higher severity category when discordant data coexist. According to this view, we should consider independent risk factors in the current cardiovascular spectrum, including, for example, the inflammation theory and the lipoprotein a. Such a comprehensive approach might mitigate limitations, ensuring patients receive timely and appropriate care.
The urgent need for timely intervention:
The study's revelation that patients with intermediate diagnoses exhibit mortality rates akin to the next-most-severe grade emphasizes the urgency of intervention, even in cases deemed less severe by traditional guidelines. Delayed referral and treatment due to underappreciation of AS severity may have dire consequences. The historical perspective provided in the manuscript underscores the gravity of this issue, emphasizing the need for a paradigm shift in the management of AS. Early intervention strategies, based on a combination of symptomatology, echocardiographic findings, and emerging technologies, must be explored to improve patient outcomes. The study's documentation of low aortic valve replacement (AVR) rates for severe AS patients (60.7 %) despite effective AVR options highlights systemic gaps in treatment adherence. Addressing these gaps requires a comprehensive approach, considering patient education, clinician awareness, and potential societal factors influencing treatment decisions.
Exploring future avenues:
The manuscript also delves into the promising future of AS management. Artificial intelligence (AI) emerges as a potential game-changer, offering a solution to the diagnostic challenges faced by clinicians. In this case, the authors used Natural Language Processing (NLP), which is a machine-learning technology that gives computers the ability to interpret, manipulate, and comprehend human language. AI-driven algorithms can enhance early detection, enabling proactive patient care and timely interventions. Additionally, ongoing research exploring the pathogenesis of calcific aortic valve disease and the possible treatment strategies through simulation analysis holds immense potential. By addressing these studying opportunities, researchers may pave the way for innovative therapeutic interventions, ultimately reducing the prognosis of AS and its associated complications.
In conclusion, the study's intricate analysis of AS severity and its consequences paints a comprehensive picture of the challenges faced by both clinicians and patients. Emphasizing the need for precise diagnosis, timely intervention, and exploring futuristic technologies, the manuscript advocates for a holistic approach to AS management. By bridging the gap between diagnostic complexities, treatment adherence, and innovative research, the medical community can transform the landscape of AS care, offering hope for improved outcomes and quality of life for patients affected by this prognostically significant and debilitating condition.