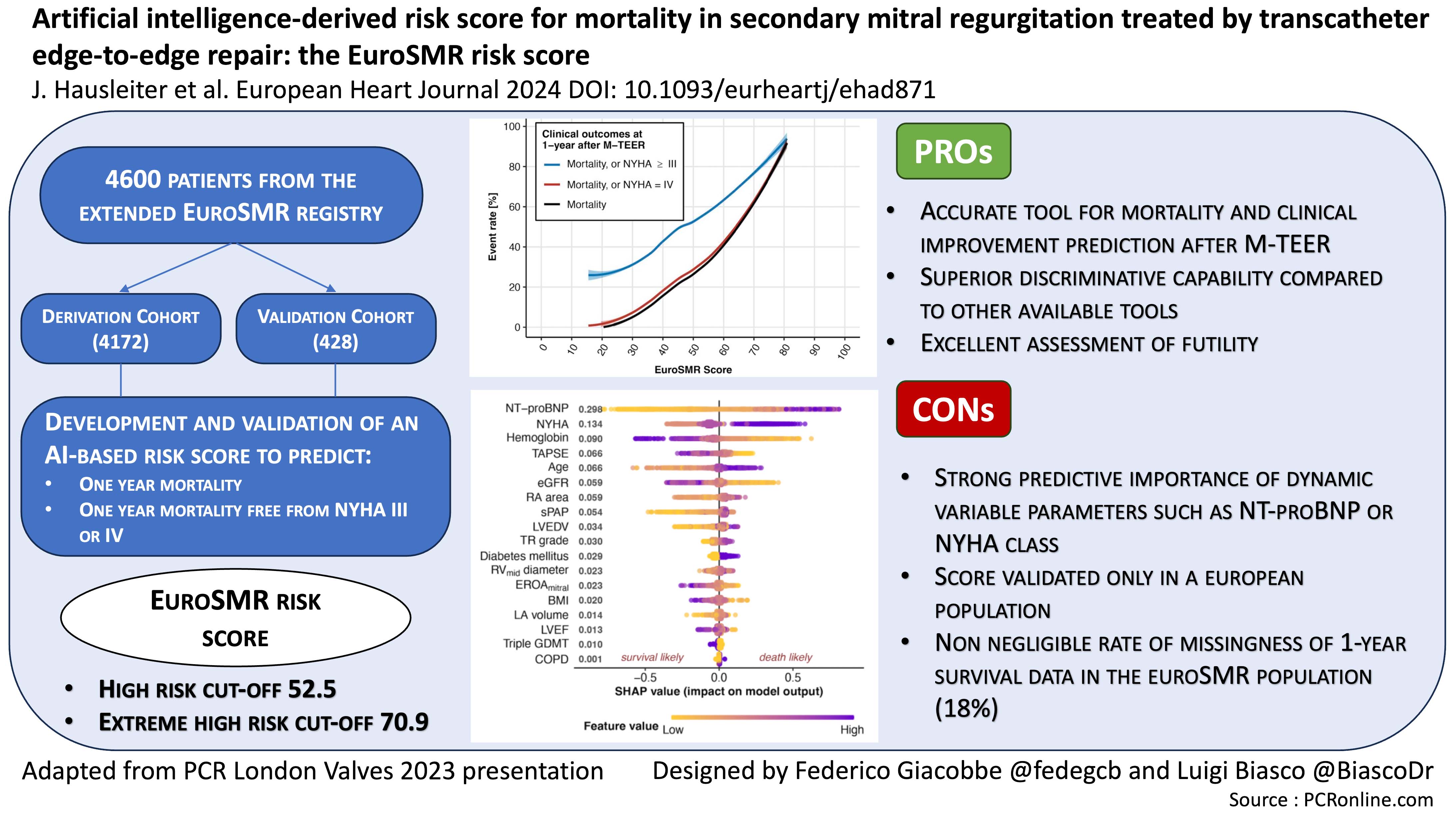
Artificial intelligence-derived risk score for mortality in secondary mitral regurgitation treated by transcatheter edge-to-edge repair: the EuroSMR risk score
Selected in European Heart Journal by L. Biasco , F. Giacobbe
The study aim was to develop and validate a novel score for prediction of 1-year mortality and clinical outcomes through artificial intelligence (AI) application in patients undergoing M-TEER.
References
Authors
Jörg Hausleiter, Mark Lachmann, Lukas Stolz, Francesco Bedogni, Antonio P Rubbio, Rodrigo Estévez-Loureiro, Sergio Raposeiras-Roubin, Peter Boekstegers, Nicole Karam, Volker Rudolph, the EuroSMR Investigators
Reference
European Heart Journal, ehad871 - European Heart Journal (2023) 00, 1–15
Published
19 January 2024
Link
Read the abstractReviewers
Our Comment
Why this study – the rationale/objective?
Optimal treatment of secondary mitral regurgitation (SMR) remains a matter of debate. While in SMR patients, surgery does not confer any prognostic impact and might be associated with a discrete surgical risk, skepticism often drives clinical decision making when evaluating high-risk patients eligible for transcatheter mitral edge-to-edge repair (M-TEER).
Notably, even after adequate treatment, a significant mid-term mortality is reported in trials and registries, while survival benefit seems to be a privilege of a specific subset of patients with definite clinical and echocardiographic characteristics, thus requiring for appropriate patients’ selection.
Furthermore, prediction of prognosis following M-TEER remains sub-optimal, as traditional surgical scores such as EuroScore II and STS score have shown poor prognostic performances, while procedure specific scores are either mainly derived from small cohorts of patients or do not differentiate between the primary and secondary etiologies of mitral regurgitation.
As a consequence, assessing patients’ prognosis and prevent potential futility remains a large unmeet need.
How was it executed – the methodology?
The study aim was to develop and validate a novel score for prediction of 1-year mortality and clinical outcomes through artificial intelligence (AI) application in patients undergoing M-TEER.
- Study Population: 4,600 patients from the extended EuroSMR registry (multicenter registry including patients derived from the retrospective EuroSMR registry, Giotto (IT), Spanish MitraScore (ES) and German Mitra Pro (DE) registries) were included in the analysis. 4,172 formed the derivation cohort, whereas 428 the validation cohort. One year follow-up data available in 3,449 patients of the derivation cohort, thus effectively used for score derivation.
- Primary outcome of interest was identified as mortality at 1 year following M-TEER. An additional secondary analysis assessing mortality and heart failure hospitalizations at 2 years was also performed to allow comparisons with COAPT trial. Finally, the composite endpoints of 1-year mortality and NYHA class IV or mortality and NYHA class ≥III at 1-year follow-up was considered as a surrogate to assess futility.
- All clinical, laboratory, echocardiographic and medication data were collected at index hospitalization or within 4 weeks prior to M-TEER. Missing values were imputed, using a random forest algorithm.
- The extreme gradient boosting (XGB) machine learning algorithm was chosen to analyze the impact of each variable on 1-year mortality. After assessing the relative impact of each different variable, they were ranked in a Shapley Additive explanation (SHAP) diagram, and the first 18 variables were used to derive the score.
- A comparison of the new AI-generated score with the current available scores (Euroscore II, COAPT, MitraScore) was carried out through ROC curves analysis.
- An extreme mortality risk prediction analysis in the validation cohort was conducted to test the ability of selecting the subgroup of patients with worse prognosis.
What is the main result?
From the analysis of the 1-year outcome in 3,449 patients followed up for a median of 1.7 years (IQR 1-2.7), the AI-generated EuroSMR score was created. The score is based on 18 parameters, 6 clinical (NYHA class, age, diabetes, BMI, triple GMDT and COPD), 9 echocardiographic (TAPSE, RA area, sPAP, LVEDV, TR grade, RV mid diameter, mitral EROA, LA volume, LVEF), and 3 lab tests (NTproBNP, haemoglobin, eGFR). The five variables with strongest impact on outcome were NTproBNP, NYHA class, haemoglobin, TAPSE and age in order of predictive importance.
Patients with a EuroSMR score over 52.5 (cut-off chosen according to Youden index) showed a hazard ratio (HR) of 4.3 (95 % CI 3.7-5.0, p < 0.001) for one year mortality as compared to patients with score < 52.5. A similar result was obtained in the validation cohort, leading to reasonable sensitivity, specificity and positive and negative predictive values.
The EuroSMR with an AUC of 0.789 performed significantly better than EuroScore II, MitraScore and COAPT score (AUC 0.705, 0.695 and 0.685 respectively) for prediction of 1-year mortality.
Furthermore, an additional analysis regarding the baseline characteristics of the patients enrolled was focused on the COAPT eligibility criteria. Patients not fulfilling the COAPT criteria showed discrete increase in one-year mortality risk compared to “COAPT-like” patients (HR 1.4, 95 % CI 1.1-1.7, p = 0.005).
An EuroSMR score > 70.9 identified a small cohort extremely high-risk patients with 1-year mortality exceeding 65 %. In this regard, the score resulted particularly accurate and extremely specific in selecting patients with a poor prognosis.
Critical reading and the relevance for clinical practice
AI-derived risk score for mortality in secondary MR treated by TEER: the EuroSMR risk score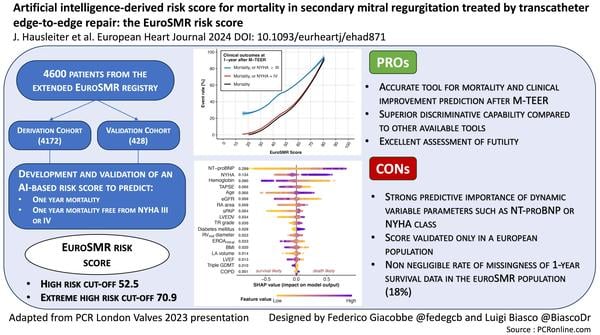
This study further points out the potential of artificial intelligence and provides clinicians with a particularly useful tool in defining the treatment pathway of patients with SMR, a matter of daily clinical discussion.
The EuroSMR risk score indeed represents an accurate tool for the prediction of mortality and clinical improvement after M-TEER that could be applied at least in the European context.
This score provided a superior discriminative capability as compared to all other currently applied tools and was associated with an excellent capability of detecting patients with scarce prognosis. This is of paramount relevance in a disease whose percutaneous treatment must always face the problem of high costs and risk of futility.
Despite the above mentioned pros of this score, some concerns regarding potential limitations have to be taken into consideration.
First, as the SHAP diagram shows, the score was derived from parameters (clinical, laboratory or echocardiographic criteria) with NTproBNP and NYHA class identified as the two most relevant variables in score definition. It is in fact well known that both NTproBNP and NYHA class might extensively fluctuate depending on loading conditions, that are rapidly impacted by medical therapy.
Moreover, assessment of those variables in a large timespan (collected at the index hospitalization or within 4 weeks prior to the M-TEER procedure) might introduce further biases impacting on prediction accuracy. As a matter of fact, for a shared decision-making process of such relevance, less dynamic parameters would be preferred.
Then, this score was obtained from real-world data acquired in European patients, hence this should be validated on different populations.
Finally, survival status at one year was unknown in about 18 % of patients. Even in the context of a retrospective registry, this is a relevant rate of missingness, that might rise concerns about the quality of data used to derive this score.
Despite these limitations, the EuroSMR score represents a valuable tool for improved prognostication of patients eligible for M-TEER procedures, as it may help clinicians in patients’ selection and avoid futility. Further analyses should focus on refining its predictive capabilities as well as to develop similar tools for the prediction of prognosis in patients with primary mitral regurgitation treated by M-TEER.






No comments yet!