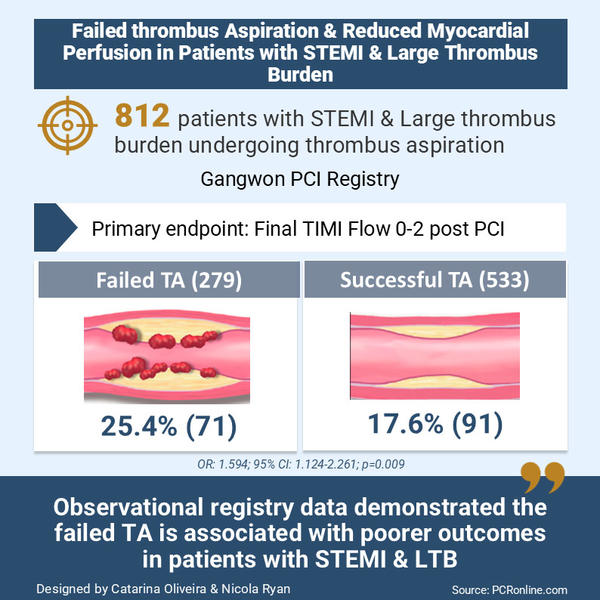
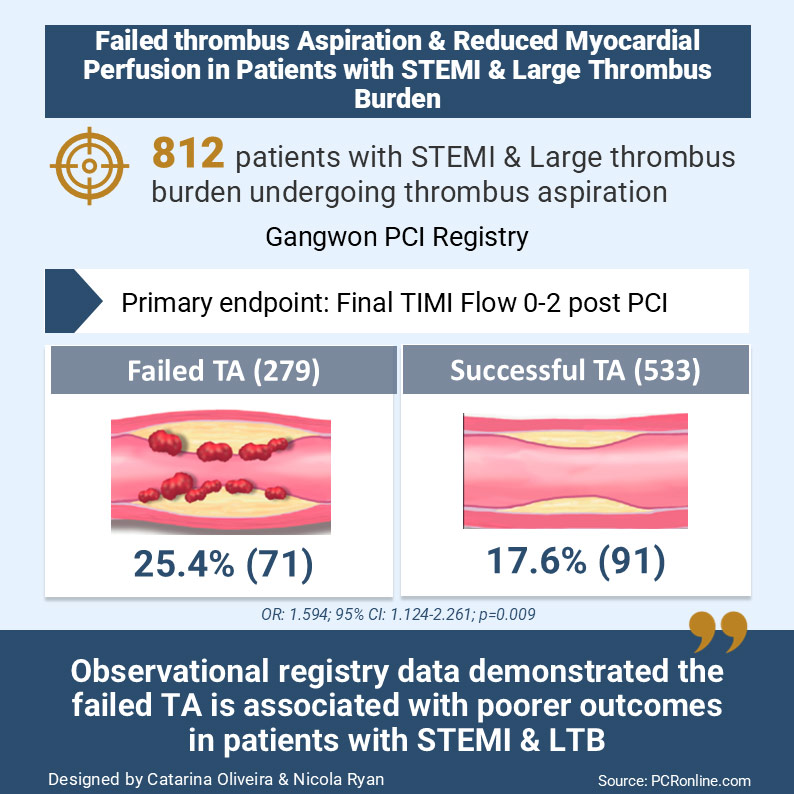
Failed thrombus aspiration and reduced myocardial perfusion in patients with STEMI and large thrombus burden
Selected in JACC: Cardiovascular Interventions by C. Oliveira , N. Ryan
This registry-based observational study demonstrated that, in patients with STEMI and LTB, TA failure was associated with reduced myocardial perfusion and increased all-cause and cardiovascular mortality.
References
Authors
Ho Sung Jeon, Young In Kim, Jung-Hee Lee, Young Jun Park, Jung-Woo Son, Jun-Won Lee, Young Jin Youn, Min-Soo Ahn, Jang-Young Kim, Byung-Su Yoo, Sung Min Ko, and Sung Gyun Ahn
Reference
J Am Coll Cardiol Intv. 2024 Oct, 17 (19) 2216–2225
Published
2024 Oct, 17
Link
Read the abstractReviewers
Our Comment
Designed by Catarina Oliveira & Nicola Ryan. Source: PCRonline.com
Why this study – the rationale/objective?
A large thrombus burden (LTB) is a risk factor for no-reflow and poorer outcomes in STEMI. Previous large trials have suggested that routine thrombus aspiration (TA) in STEMI is not beneficial1-4, and, therefore, not recommended in the current guidelines5, thrombus aspiration has declined but is still used in clinical practice.
The authors hypothesized that ineffective TA leads to reduced myocardial perfusion and poorer outcomes in STEMI patients with LTB. This study aimed to investigate the impact of TA failure on myocardial perfusion and clinical outcomes in STEMI patients with LTB undergoing primary PCI.
How was it executed – the methodology?
This is a sub-analysis of the prospective, multicenter, observational Gangwon PCI Registry.
Coronary angiography and primary PCI were conducted per local STEMI protocols. Manual TA was performed in coronary lesions, with visible thrombus or complete occlusion of the culprit artery. If the TA catheter could not cross the lesion, 8.2 % of the cases, predilation was performed. TA was repeated until the thrombotic debris was completely retrieved, or residual thrombus was negligible or not seen. If a visible thrombus remained after several attempts at TA when no further thrombus was retrieved, PCI was performed.
The primary outcome was:
- Final TIMI flow grade observed on angiography following primary PCI.
Secondary outcomes included:
- The final myocardial blush grade.
- ST-segment resolution on electrocardiography 60 to 90 minutes after primary PCI.
- Microvascular obstruction evaluated by cardiac magnetic resonance imaging.
- Infarct size assessed via CMR 3 to 5 days post-PCI.
- All-cause mortality, cardiac death, stent thrombosis, and target vessel revascularisation (TLR) at one month.
What is the main result?
A total of 812 patients with STEMI and LTB were included, 34.4 % (279) in the failed TA group, and 65.6 % (533) in the successful group.
Three quarters of patients were male, with a mean age of 66.1 ± 12.8 years (failed TA) and 63.1 ± 12.8 years (successful TA). The groups were comparable regarding cardiovascular risk factors, atrial fibrillation, and total ischemic time. However, a higher proportion of patients in the failed TA group presented with Killip class III or IV and were more likely to be prescribed Ticagrelor. TA failed more commonly in non-LAD arteries as well as in tortuous or calcified arteries.
- TIMI flow grade 0-2 at the end of the procedure was observed in 25.4 % of patients in the failed TA group vs. 17.6 % in the successful TA group (OR: 1.594, 95 % CI: 1.124-2.261, p = 0.009).
- Complete ST-segment resolution occurred more frequently in the successful TA group (35.8 % vs. 48 %, p = 0.001)
- Myocardial blush grade (19.7 % vs. 13.7 %; p = 0.0026) and infarct size on late gadolinium enhancement (35 % vs. 38 %, p = 0.015) were worse in the failed TA group.
- All-cause mortality (11.8 % vs. 7.1 %, p = 0.024) and cardiovascular death (11.1 % vs. 6.4 %, p = 0.018) were higher in the failed TA group.
Critical reading and the relevance for clinical practice
This registry-based observational study demonstrated that, in patients with STEMI and LTB, TA failure was associated with reduced myocardial perfusion and increased all-cause and cardiovascular mortality.
Initially, there was significant interest in the use of TA when small randomised trials showed a benefit in terms of improved angiographic and electrocardiographic predictors of myocardial reperfusion and one-year mortality with TA compared to PCI alone.
However, subsequent large-scale studies including almost 18,000 patients failed to confirm this advantage. Indeed in the TOTAL Trial4, there was an increased rate of stroke in the TA arm.
The authors hypothesise that the improved outcomes in this study may be related to the thrombus removal rate of 90 %, compared to 70 % reported in earlier studies. However, an important limitation of this suggestion and the paper as a whole is the non-randomisation. In general, patients with unsuccessful procedures have poorer outcomes than successful procedures. Furthermore, predictors of non-successful TA included elderly patients, non-anterior STEMI, longer time from symptoms, Killip Class > 2, moderate or severe tortuosity and calcification. These features are not easily mitigated for and one needs to be cognizant of the potential complications from TA, such as embolic stroke or distal embolization. In this study, stroke rates were not reported.
A prior individual patient meta-analysis has suggested that there is a potential sub-group of patients with high thrombus burden who may benefit from TA, though with the concomitant increased risk of stroke8. The results from this observational study suggest that there are patient features which are unfavourable for TA. Newer thrombus aspiration devices, such as those with continuous suction as well as stent retrievers, initially developed for the treatment of stroke, have shown potential beneficial effects in non-randomised small trials and case series.
Further large randomised controlled trials are necessary to clarify the role of TA, including that of newer potentially safer devices. Specific clinical scenarios where TA may be beneficial, such as in cases of LTB, alongside situations where it may be harmful, particularly in older patients with hemodynamic instability or in cases with unfavorable coronary anatomy, such as tortuosity and calcification require further clarification to provide the safest and most efficacious treatment for all patients.
References
- Svilaas T, Vlaar PJ, van der Horst IC, et al. Thrombus aspiration during primary percutaneous coronary intervention. N Engl J Med. 2008;358:557–567.
- Vlaar PJ, Svilaas T, van der Horst IC, et al. Cardiac death and reinfarction after 1 year in the Thrombus Aspiration During Percutaneous Coronary Intervention in Acute Myocardial Infarction Study (TAPAS): a 1-year follow-up study. Lancet. 2008;371:1915–1920.
- Frobert O, Lagerqvist B, Olivecrona GK, et al. Thrombus aspiration during ST-segment elevation myocardial infarction. N Engl J Med. 2013;369:1587–1597.
- Jolly SS, Cairns JA, Yusuf S, et al. Randomized trial of primary PCI with or without routine manual thrombectomy. N Engl J Med. 2015;372:1389–1398.
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40:87–165.
- Jeon HS, Kim Y, Lee JH, et al. Failed Thrombus Aspiration and Reduced Myocardial Perfusion in Patients With STEMI and Large Thrombus Burden. JACC: Cardiovascular Interventions 2024;17(19): 2216-2225
- Bhindi R, Kajander OA, Jolly SS, et al. Culprit lesion thrombus burden after manual thrombectomy or percutaneous coronary intervention-alone in ST-segment elevation myocardial infarction: the optical coherence tomography sub-study of the TOTAL (Thrombectomy Versus PCI Alone) trial. Eur Heart J. 2015;36:1892–1900.
- Jolly SS, James S, Džavík V, et al. Thrombus Aspiration in ST-Segment-Elevation Myocardial Infarction: An Individual Patient Meta-Analysis: Thrombectomy Trialists Collaboration. Circulation. 2017;135:143–152.




No comments yet!