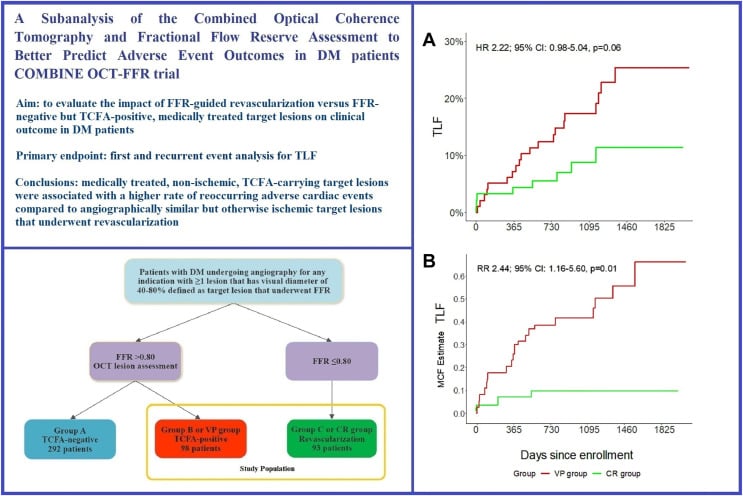
Medically treated nonischemic thin-cap fibroatheroma lesions versus fractional flow reserve-guided complete revascularization in diabetic patients
Selected in JSCAI (Journal of the Society of Cardiovascular Angiography & Interventions) by M. Alasnag
This sub-analysis denotes that medically treated diabetic patients with FFR-negative, TCFA-carrying target lesions were associated with a higher rate event rate compared to angiographically similar ischemic target lesions that underwent revascularization.
References
Authors
Tobias M. Hommels, Renicus S. Hermanides, Enrico Fabris, Krzysztof P. Malinowski, Balázs Berta, Tomasz Roleder, Fernando Alfonso, Giuseppe De Luca, Rohit M. Oemrawsingh, Wojciech Wojakowski, Arnoud W.J. van ‘t Hof, Elvin Kedhi
Reference
DOI: https://doi.org/10.1016/j.jscai.2023.101256
Published
December 12, 2023
Link
Read the abstractReviewer
My Comment
Why this study – the rationale/objective?
The COMBINE OCT-FFR study was a prospective, double-blind, international study evaluating the impact of optical coherence tomography (OCT)-detected thin-cap fibroatheroma (TCFA) on clinical outcomes in diabetic patients with fractional-flow-reserve(FFR)-negative lesions. The trial noted that, among diabetic patients with ≥ 1 FFR-negative lesions, TCFA-positive lesions constituted 25 % of those enrolled, and were associated with a five-fold higher rate of major adverse cardiovascular events (MACE), even in the absence of ischemia.
These findings are concerning and warrant reconsideration of how we currently stratify risk in diabetic patients. Is anatomic risk more important than ischemia? The ISCHEMIA trial demonstrated a lower rate of spontaneous myocardial infarctions (MI) in the ischemia-guided revascularization arm, suggesting that those without ischemia and treated medically were in fact vulnerable and prone to future events.
Is epicardial stenosis more predictive than TCFA in diabetic patients or are they complementary? The COMPLETE OCT sub-study noted that obstructive lesions were more commonly harboring vulnerable plaques than non-obstructive lesions.
How was it executed – the methodology?
In this pre-specified sub-analysis of the COMBINE OCT-FFR trial, Hommels et al. evaluate the role of medically treated target lesions. Diabetic individuals with ≥ 1 FFR-negative, TCFA-positive medically treated target lesions are deemed vulnerable plaque (VP group). These were compared to patients with exclusively FFR-positive target lesions undergoing complete revascularization (CR group). TCFA was defined as any coronary target lesion with a predominantly lipid-rich plaque in which the thinnest part of the atheroma cap measured ≤ 65 μm and lipid arc > 90°. The OCT assessment was performed by 2 investigators.
The primary endpoint was target lesion failure (TLF), a composite of cardiac death, target vessel myocardial infarction (TV-MI), or clinically driven target lesion revascularization (TLR). TLR was clinically driven.
The secondary endpoint was a composite endpoint of cardiac death, TV-MI, TLR, or hospitalization due to unstable angina. Periprocedural and spontaneous MI and TV-MI were also reported as a safety endpoint for the trial.
What is the main result?
Source: Journal of the Society for Cardiovascular Angiography & Interventions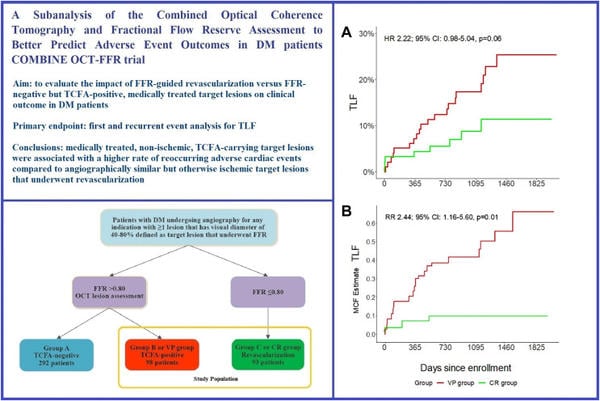
A total of 191 patients were included (98 in the VP group and 93 in the CR group). The mean age was 67 years old, and men constituted 66 %, and 74 % of each group respectively. These were well-controlled diabetic patients with a mean HbA1c of 57 mmol/mol and normal renal function. 24-36 % were on insulin.
Additional risk factors included hyperlipidemia in 62-66 %, and a smaller percent were smokers (17-22 %). Non-acute coronary syndrome was the predominant presentation, with 41-46 % having prior percutaneous revascularization.
The primary endpoint occurred more frequently in the VP group (20.4 % vs 8.6 %; P = 0.06). They also had a higher rate of the secondary endpoints (P < 0.01). A nonsignificant trend for more MIs in the VP group: any (11.2 % vs 7.5 %; P = 0.45), TV-MI (6.1 % vs 3.3 %; P = 0.42) and spontaneous TV-MI (6.1 % vs 1.1 %; P = 0.12).
Critical reading and the relevance for clinical practice
This sub-analysis denotes that medically treated diabetic patients with FFR-negative, TCFA-carrying target lesions were associated with a higher rate event rate compared to angiographically similar ischemic target lesions that underwent revascularization. Since acute coronary syndromes are considered pro-inflammatory and pro-thrombotic conditions, deferring revascularization on the basis of FFR guidance is associated with higher rates of adverse cardiac events in such patients. Yet, in this analysis, we note that the majority did not sustain an ACS, suggesting that diabetes per se may play a more direct role in the inflammatory process. Plaque morphology and composition may be a better predictor of future events, even in absence of ischemia in such patients.
Ongoing randomized trials such as the COMBINE-INTERVENE and INTERCLIMA will evaluate the role of OCT-detected vulnerable plaque-guided revascularization, either alone or in combination with FFR and may shed light into this hypothesis.
This trial does not, however, answer important questions: how predictive is plaque morphology in patients who are poorly-controlled diabetics, or those with end organ damage? We recognize that rapid plaque progression as well as silent plaque disruption and subsequent healing are common findings in diabetic patients’ intracoronary studies. Given the low HbA1C levels, what is the impact of the novel anti-diabetic and lipid lowering agents on plaque stabilization/healing and clinical outcomes?
As intriguing as this analysis may be, it remains hypothesis generating and unlikely to change practice soon. Streamlining the evaluation of thin cap plaques and the functional assessment of diffusely diseased vessels is the Achilles heel of the management of diabetic patients, and will limit the application in daily practice. In spite of such reservations, this is a paradigm shift in how we stratify and manage diabetic patients. Perhaps we need to perform more intracoronary imaging and assess plaque morphology rather than search for symptoms, percent stenosis or ischemia.
References
- Kedhi E, Berta B, Roleder T, Hermanides RS, Fabris E, IJsselmuiden AJJ, Kauer F, Alfonso F, von Birgelen C, Escaned J, Camaro C, Kennedy MW, Pereira B, Magro M, Nef H, Reith S, Al Nooryani A, Rivero F, Malinowski K, De Luca G, Garcia Garcia H, Granada JF, Wojakowski W. Thin-cap fibroatheroma predicts clinical events in diabetic patients with normal fractional flow reserve: the COMBINE OCT-FFR trial. Eur Heart J. 2021 Dec 1;42(45):4671-4679.
- Stone GW, Ali ZA, O'Brien SM, Rhodes G, Genereux P, Bangalore S, Mavromatis K, Horst J, Dressler O, Poh KK, Nath RK, Moorthy N, Witkowski A, Dwivedi SK, Bockeria O, Chen J, Smanio PEP, Picard MH, Chaitman BR, Berman DS, Shaw LJ, Boden WE, White HD, Fremes SE, Rosenberg Y, Reynolds HR, Spertus JA, Hochman JS, Maron DJ; ISCHEMIA Research Group. Impact of Complete Revascularization in the ISCHEMIA Trial. J Am Coll Cardiol. 2023 Sep 19;82(12):1175-1188.
- Pinilla-Echeverri N, Mehta SR, Wang J, Lavi S, Schampaert E, Cantor WJ, Bainey KR, Welsh RC, Kassam S, Mehran R, Storey RF, Nguyen H, Meeks B, Wood DA, Cairns JA, Sheth T. Nonculprit Lesion Plaque Morphology in Patients With ST-Segment-Elevation Myocardial Infarction: Results From the COMPLETE Trial Optical Coherence Tomography Substudys. Circ Cardiovasc Interv. 2020 Jul;13(7):e008768.





No comments yet!