26 Jan 2024
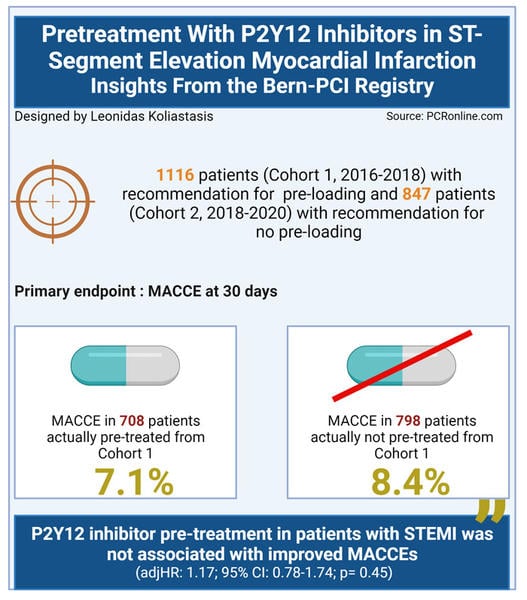
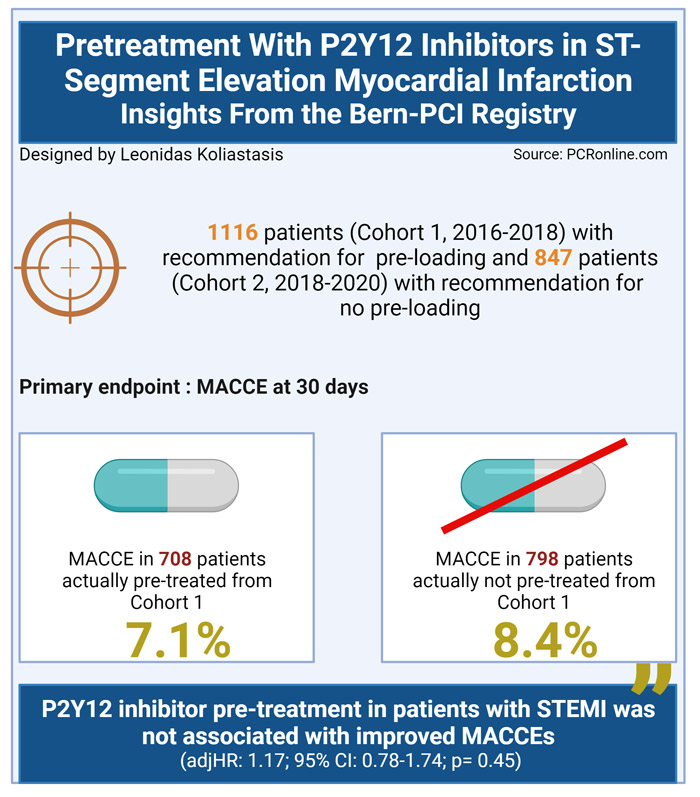
Pretreatment with P2Y12 inhibitors in ST-segment elevation myocardial infarction - insights from the Bern-PCI Registry
Selected in JACC: Cardiovascular Interventions by L. Koliastasis , P. Xaplanteris
This study sought to compare outcomes between patients presenting with STEMI before and after the recent ESC guidelines for the management of ACS recommend against pre-treatment with P2Y12 inhibitors in STEMI patients.
References
Authors
Miklos Rohla, Shirley Xinyu Ye, Hiroki Shibutani, Jolie Bruno, Tatsuhiko Otsuka, Jonas D. Häner, Sarah Bär, Fabrice Temperli, Raminta Kavaliauskaite, Jonas Lanz, Stefan Stortecky, Fabien Praz, Lukas Hunziker, Thomas Pilgrim, George CM. Siontis, Sylvain Losdat, Stephan Windecker, and Lorenz Räber
Reference
J Am Coll Cardiol Intv. 2024 Jan, 17 (1) 17–28
Published
January 2024
Link
Read the abstractReviewers
Our Comment
Why this study – the rationale/objective?
The recent ESC guidelines for the management of ACS recommend against pre-treatment with P2Y12 inhibitors in patients presenting with STEMI2. In the Bern-PCI Registry, local guidance changed in 2018, with pre-treatment no longer recommended.
This study sought to compare outcomes between patients presenting with STEMI before and after the recommendations changed.
How was it executed – the methodology?
All patients presenting with STEMI from 2016-2020, enrolled in the Bern-PCI Registry, were included in this study. From 2016 to 2018, 1,116 patients were included in the registry, of whom 708 were pre-treated with a P2Y12 inhibitor (Cohort 1). Following the recommendation not to pre-treat with a P2Y12 inhibitor, 847 patients were included from 2018-2020, of whom 798 were not pre-treated (Cohort 2).
All patients received 250 mg of iv aspirin, and 5,000 units of iv heparin as soon as a STEMI diagnosis was established. PCI techniques and use of GP IIb/IIIa inhibitors was left to the operators’ discretion. Prasugrel and ticagrelor were the preferred P2Y12 inhibitors, however choice of agent was left to the operators’ discretion.
- The primary endpoint was MACCE (all-cause death, recurrent MI, stroke or definite stent thrombosis) at 30 days.
- The secondary endpoints included the individual components of the primary endpoint, target vessel MI, and Bleeding Academic Research Consortium (BARC) 3 or 5 bleeding.
- A sensitivity analysis comparing cohort 1 vs cohort 2 excluding all patients for which the recommendations were not followed was carried out
What is the main result?
The majority of patients were male (76 %), with a mean age of 65.2 ± 12.5 years. Traditional cardiovascular risk factors were common, with 10 % of the population having prior PCI, and there were no differences between the groups. In keeping with the time frame, studied thrombus aspiration was performed more frequently in Cohort 1 (30 % vs 21 %, p < 0.01). Ticagrelor was the most frequently used second antiplatelet (77 %). The LAD was the most commonly treated vessel (46 %), followed by the RCA (36 %).
- There was no difference in the primary endpoint between groups (10.1 % vs 8.1 %; adjusted HR: 0.91; 95 % CI: 0.65-1.28; p = 0.59)
- When comparing patients who did versus did not receive pre-treatment as recommended during the respective time periods, there was no difference in MACCE (Pre-treatment 7.1 % vs No Pre-treatment 8.4 %; adjusted HR: 1.17; 95 % CI: 0.78-1.74; p = 0.45)
- There were no significant differences in secondary endpoints between cohorts or treatment strategies
- The mean difference in P2Y12 loading was 100 minutes between pre-loaded and no pre-loaded (p < 0.01).
Critical reading and the relevance for clinical practice
This study demonstrated that, in patients presenting with STEMI, MACCE rates were similar during time periods where pre-loading with a P2Y12 inhibitor was and was not recommended. Restricting the analysis to patients who were treated in line with recommendations, there was no difference in outcomes between pre-loading versus delayed loading with P2Y12 inhibitors in STEMI patients.
From an operator perspective, one of the key potential benefits of pre-loading is the reduction in risk of stent thrombosis. In this analysis, there was no differences in definite stent thrombosis between cohorts (0.8 % vs. 0.8 %, unadj HR 1.02, 95 % CI 0.38-2.73, adj HR 0.97, 95 % CI 0.29-3.46), or treatment strategies (pre-treatment 0.7 % vs. no pre-treatment 0.9 %, unadj HR 1.26, 95% CI 0.40-3.97, adj HR 1.17, 95 % CI 0.32-4.33).
A potential disadvantage of pre-treatment is increased bleeding risk. Whilst this study did not show differences between groups, there is a number of factors which may have contributed to this including, the pre-treatment with heparin in all patients, as well as the exclusion of patients who did not undergo PCI. From a technical point of view, thrombus aspiration was more common in the first cohort, however, given the shift in evidence away from routine thrombus aspiration, it is difficult to draw significant conclusions from this.
An important limitation of this study is that it only included patients who underwent PCI. Therefore, patients with spontaneous coronary artery dissection, aortic dissection, vasospasm, and those receiving conservative or surgical treatment were not included in the analysis. The outcomes in these populations would be of interest as they are subsets who potentially may have adverse events due to pre-treatment with P2Y12 inhibitors. Routine use of GP IIb-IIIa inhibition is not recommended in current guidelines, a potential increased use due to lack of P2Y12 inhibitor pre-loading was not borne out in this study.
This real-world study provides helpful evidence with regard to timing of P2Y12 inhibitor loading in patients who undergo PCI. Further evidence is required in the overall cohort of patients presenting with STEMI including those who do not undergo PCI either due to the requirement for CABG or presenting with a STEMI mimic.
References
- Rohla M, Ye SX, Shibutani H, Bruno J, Otsuka T, Häner JD, Bär S, Temperli F, Kavaliauskaite R, Lanz J, Stortecky S, Praz F, Hunziker L, Pilgrim T, Siontis GC, Losdat S, Windecker S, Räber L. Pretreatment With P2Y12 Inhibitors in ST-Segment Elevation Myocardial Infarction: Insights From the Bern-PCI Registry. JACC Cardiovasc Interv. 2024 Jan 8;17(1):17-28. doi: 10.1016/j.jcin.2023.10.064. PMID: 38199749.
- Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, Claeys MJ, Dan GA, Dweck MR, Galbraith M, Gilard M, Hinterbuchner L, Jankowska EA, Jüni P, Kimura T, Kunadian V, Leosdottir M, Lorusso R, Pedretti RFE, Rigopoulos AG, Rubini Gimenez M, Thiele H, Vranckx P, Wassmann S, Wenger NK, Ibanez B; ESC Scientific Document Group. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-3826. doi: 10.1093/eurheartj/ehad191. PMID: 37622654.





1 comment
The mean difference in P2Y12 loading was 100 minutes between pre-loaded and no pre-loaded, as patients are loaded with Tica I think thats not a long enough time to determine differences in outcomes. Should Clopidogrel be used as in many areas of the world, I think results would be different