Structural cardiac interventions in patients with heart failure
Selected in Journal of the American College of Cardiology by A. Sticchi
The review aims to address the unmet needs in heart failure (HF) management, particularly in patients where structural heart disease coexists with HF and limits the effectiveness of guideline-directed medical therapy (GDMT).
References
Authors
Rebecca T. Hahn, JoAnn Lindenfeld, Scott D. Lim, Michael J. Mack, and Daniel Burkhoff
Reference
JACC. 2024 Aug, 84 (9) 832–847
Published
August 2024
Link
Read the abstractReviewer
My Comment
Why this study – the rationale/objective?
Visual designed by Alex Sticchi to illustrate how early, tailor-made structural interventions can improve heart failure management. Source : PCRonline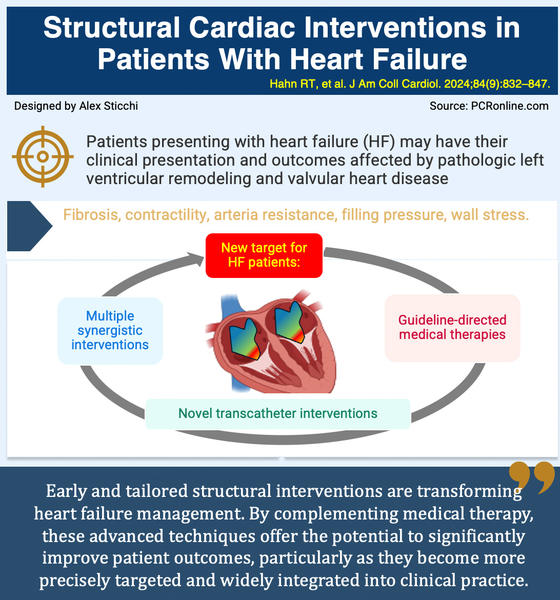
Purpose:
The review aims to address the unmet needs in heart failure (HF) management, particularly in patients where structural heart disease coexists with HF and limits the effectiveness of guideline-directed medical therapy (GDMT).
These structural abnormalities, including left ventricular (LV) remodeling and valvular heart disease, can exacerbate HF symptoms and contribute to poor outcomes, necessitating the exploration of advanced interventional strategies.
Objective:
The main objective is to critically evaluate and summarize the current and investigational transcatheter interventions that target these structural contributors to heart failure, with a focus on the potential for these therapies to enhance patient outcomes when traditional medical therapies are insufficient.
How was it executed – the methodology?
Scope:
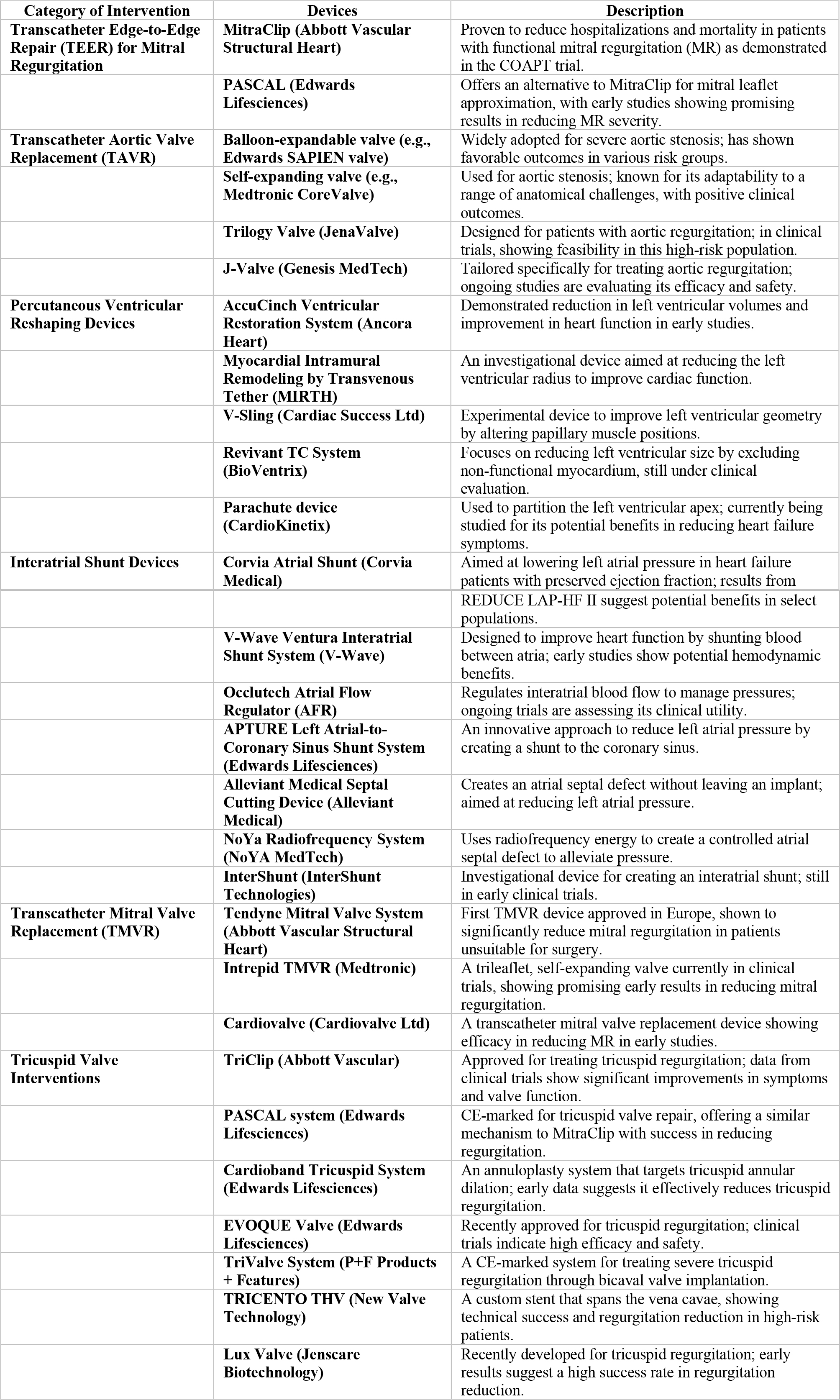
This review encompasses a broad range of interventions aimed at structural heart disease in HF, focusing specifically on LV remodeling and valvular heart diseases like mitral regurgitation (MR) and aortic stenosis (AS). The review includes both well-established therapies, such as TAVR and TEER, as well as novel devices that are still in the feasibility or early clinical trial phases.
Sources:
The review draws from randomized controlled trials, early feasibility studies, and observational studies, providing a comprehensive examination of both the safety and efficacy of these interventions.
Criteria:
The focus is on interventions that show promise in significantly altering the disease course for patients with structural heart disease who remain symptomatic despite optimal GDMT. The review emphasizes the need for robust clinical evidence to support the integration of these therapies into clinical practice.
What is the main result?
- Significance of early and targeted intervention: the review emphasizes the importance of early and precise intervention in managing heart failure due to structural heart diseases. For example, the COAPT trial, which evaluated the MitraClip device for transcatheter edge-to-edge repair (TEER) in patients with functional mitral regurgitation (MR), demonstrated a significant 47 % reduction in heart failure hospitalizations and a 38 % reduction in all-cause mortality over two years in patients who were symptomatic despite guideline-directed medical therapy (GDMT). These results were not possible in the MITRA-FR where the intervention occurred at a late disease stage.
- Complementary role of transcatheter Interventions: transcatheter interventions such as TEER and Transcatheter Aortic Valve Replacement (TAVR) are highlighted as essential complements to GDMT. These procedures have been shown to provide substantial benefits, especially in patients who remain symptomatic despite optimal medical management. The COAPT trial results for MitraClip underscore this point, showing that TEER can significantly improve outcomes when used alongside GDMT.
- Evolving evidence and expanding indications: the document discusses how indications for interventions like TAVR are expanding, driven by emerging evidence that suggests earlier use may prevent progression to more severe disease states. For example, ongoing studies are investigating the benefits of TAVR in patients with moderate aortic stenosis (AS) who exhibit early signs of left ventricular dysfunction, potentially leading to changes in clinical practice.
- Innovative technologies in the pipeline: several new devices are currently under clinical investigation, offering promising options for non-surgical heart failure management. The AccuCinch Ventricular Restoration System, for instance, has demonstrated a significant reduction in left ventricular end-diastolic volume (LVEDV) and improvements in functional capacity in early studies. These technologies represent a significant advancement in the treatment of structural heart disease and are likely to play a more prominent role in future care strategies.
- Challenges in patient selection and procedural success: the review highlights the critical role of patient selection in ensuring the success of structural interventions. For instance, the discrepancy in outcomes between the COAPT and MITRA-FR trials for TEER underscores the importance of selecting patients based on specific anatomical and functional criteria. This points to the need for advanced imaging and diagnostic tools to better identify candidates who are most likely to benefit from these procedures.
Table of Structural Cardiac Intervention Devices in Heart Failure
Critical reading and the relevance for clinical practice
The future of heart failure management is poised to be transformed by a series of technological advancements, shifting the focus towards personalized, minimally invasive interventions. Precision medicine will likely become a cornerstone in this evolution, leveraging genetic profiling, advanced imaging techniques, and artificial intelligence (AI) to tailor treatment strategies to individual patients. By integrating these technologies, clinicians will be better equipped to select the most appropriate structural interventions, such as TEER, TAVR, and TMVR, thereby optimizing outcomes and reducing the risk of complications.
Cardiac remodeling without the need for invasive surgery is expected to gain traction, as evidenced by the promising early results from devices like the AccuCinch Ventricular Restoration System. This device has shown the ability to significantly reduce left ventricular volumes, suggesting that future therapies may increasingly rely on such minimally invasive approaches to manage dilated cardiomyopathies. As these technologies mature, they could offer alternatives to traditional surgery, potentially leading to a paradigm shift in how heart failure is treated.
Another area of significant potential is the development of interatrial shunt devices aimed at addressing heart failure with preserved ejection fraction (HFpEF), a condition that remains difficult to treat effectively. Devices like the Corvia Atrial Shunt, which have been tested in clinical trials, highlight the potential for mechanical solutions to address the hemodynamic challenges associated with HFpEF. Although challenges remain, particularly in refining patient selection and optimizing device design, these innovations could eventually provide new hope for a population that has few effective treatment options.
In the realm of valve technology, advancements are being made with devices such as the Trilogy Valve and J-Valve, specifically designed for complex cases like aortic regurgitation. These next-generation valves are showing promise in terms of safety and efficacy, with early trials indicating their potential to reduce procedural risks and improve patient outcomes. As these technologies continue to develop, they are likely to become integral components of heart failure management, offering less invasive alternatives to open-heart surgery.
Overall, the future of heart failure management will likely be characterized by the integration of advanced technologies, personalized medicine, and a more profound understanding of cardiac pathophysiology. These developments promise to improve patient outcomes, reduce the invasiveness of treatments, and offer new solutions for patients with complex structural heart diseases.
As these innovations move from clinical trials into broader practice, they hold the potential to significantly alter the landscape of heart failure treatment, providing patients with more effective and less invasive options for managing their conditions.









No comments yet!