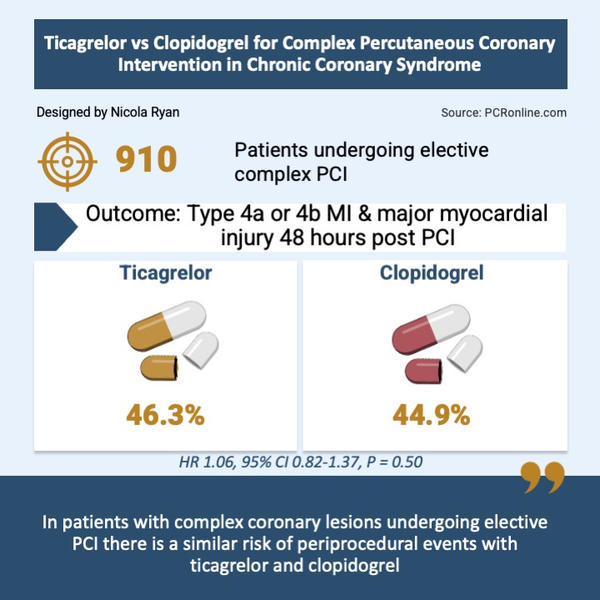
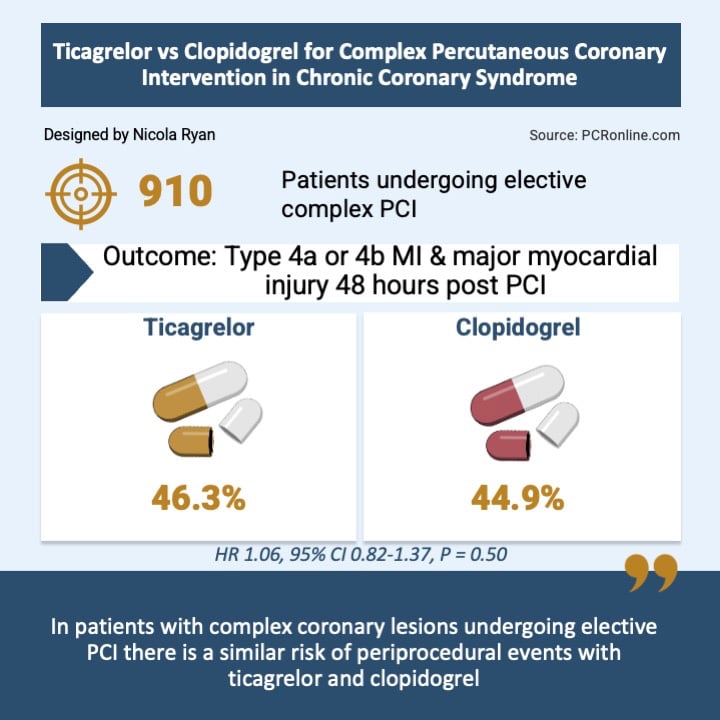
Ticagrelor vs Clopidogrel for complex percutaneous coronary intervention in chronic coronary syndrome
Selected in JACC: Cardiovascular Interventions by S. Iwanczyk , N. Ryan
The results of this sub-analysis of the ALPHEUS trial show that complex PCI criteria are present in a large percentage of patients with chronic coronary syndrome and are associated with higher rates of both periprocedural events and MACE than non-complex PCI.
References
Authors
Benoit Lattuca, Cedric Mazeau, Guillaume Cayla, Grégory Ducrocq, Paul Guedeney, Mikael Laredo, Raphaëlle Dumaine, Mohamad El Kasty, Petr Kala, Mohammed Nejjari, Ota Hlinomaz, Olivier Morel, Olivier Varenne, Florence Leclercq, Laurent Payot, Christian Spaulding, Farzin Beygui, Grégoire Rangé, Zuzana Motovska, Jean-Jacques Portal, Eric Vicaut, Jean-Philippe Collet, Gilles Montalescot, Johanne Silvain, and on behalf of the ALPHEUS Investigators
Reference
J Am Coll Cardiol Intv. 2024 Feb, 17 (3) 359–370
Published
17 February 2024
Link
Read the abstractReviewers
Our Comment
Ticagrelor is a more potent P2Y12 inhibitor than Clopidogrel, and has been shown to significantly reduce ischaemic events in patients presenting with acute coronary syndrome1.
The ALPHEUS (Assessment of Loading with the P2Y12 inhibitor ticagrelor or clopidogrel to Halt ischaemic Events in patients Undergoing elective coronary Stenting) trial failed to demonstrate superiority of Ticagrelor above Clopidogrel to reduce periprocedural events in patients undergoing elective PCI2.
In this sub-analysis, the authors analysed the outcomes of patients undergoing complex PCI and the relative efficacy of ticagrelor and clopidogrel.
Designed by Nicola Ryan
Why this study – the rationale/objective?
Prasugrel and Ticagrelor are recommended by the current European Society of Cardiology (ESC) guidelines as first-line therapy in patients with acute coronary syndrome, reducing significantly the rates of cardiac events when compared to Clopidogrel3.
So far, no benefit has been demonstrated from the use of Prasugrel and Ticagrelor in chronic coronary syndrome2. However, as the complex percutaneous coronary intervention (PCI) subgroup usually requires a more aggressive approach and may be associated with a higher risk of periprocedural complications and a worse long-term prognosis, Prasugrel and Ticagrelor are frequently used off-label among these patients, despite the lack of robust evidence.
Assessment of the risk of periprocedural complications and long-term outcomes, as well as the relative efficacy of Ticagrelor and Clopidogrel among patients undergoing complex PCI compared to non-complex procedure, is essential to optimize treatment and improve prognosis.
How was it executed – the methodology?
All patients with chronic coronary syndrome, undergoing non-emergent PCI, enrolled in the ALPHEUS study, were divided into two groups: complex or non-complex PCI. The patients were randomized 1:1 to receive a loading dose of Ticagrelor or Clopidogrel before the PCI procedure, followed by a 30-day maintenance treatment.
Complex PCI was defined as a procedure including at least one of following criteria: multiple stents implanted, total stent length > 60 mm, 2-stent bifurcation technique, left main stenting, PCI of chronic total occlusion, use of atherectomy, and PCI of arterial or saphenous coronary graft. Based on this criteria, the population was divided into 4 groups: non-complex PCI, low-complexity PCI (1 criterion), intermediate-complexity PCI (2 criteria), and high-complexity PCI (3 or more criteria).
The primary endpoint was the composite of periprocedural myocardial infarction (MI) (type 4a, 4b) and major myocardial injury during the 48 hours after the PCI (or at discharge if this was earlier).
Secondary endpoints included major adverse cardiac events (MACE) at 48 hours and 1 month defined by the composite of any death, all types of MI, or stroke/transient ischemic attack; Any myocardial injury at 48 hours and 1-month, procedural complications; occurrence of coronary slow-flow, coronary no-flow, coronary dissection, and transient or permanent per-procedure coronary thrombus and major bleeding events evaluated by the BARC criteria (BARC 3 or 5) at 1 month.
What is the main result?
Of the 1,910 patients enrolled in the ALPHEUS trial, 910 (48.8 %) had one or more criteria for complex PCI, 460 in the Ticagrelor group, and 450 in the Clopidogrel group.
Multiple stents implanted and stent length > 60 mm were the most common criteria for complex PCI.
- The rate of primary endpoint of periprocedural MI and major myocardial injury was significantly higher in the complex PCI group than in the noncomplex population (46.6 % vs 26.6 %, P < 0.001) with 2.5-fold higher rate of periprocedural MI (type 4a or b) (12.2 % vs 4.8 %; P < 0.001).
- MACE occurred more frequently in the complex PCI group, at both 48 hours (12.7 % vs. 5.1 %, P < 0.005) and 30 days ( 13.4 % vs. 5.3 %, P < 0.05).
- The rate of angiographic complications was higher in the complex PCI group (19.3 % vs 8.6 %, P < 0.05).
- There was no significant interaction between antiplatelet randomization and complexity of PCI for the primary endpoint at 48 hours (P interaction = 0.47).
- There were numerically higher type 4a MI’s and major myocardial injury in the complex PCI group but without significant impact of the allocated treatment (P interaction = 0.07 and P interaction = 0.76, respectively).
- When the primary endpoints were analysed according to complex PCI criteria, there was a lower occurrence of the primary endpoint in patients with 2-stent bifurcation PCI treated with clopidogrel and in patients treated with Ticagrelor for LMS stenting.
Critical reading and the relevance for clinical practice
The results of this sub-analysis of the ALPHEUS trial show that complex PCI criteria are present in a large percentage of patients with chronic coronary syndrome, and are associated with higher rates of both periprocedural events and MACE than noncomplex PCI.
There was a stepwise increase in the primary endpoint, as the number of criteria for complex PCI increased, from 37.0 % for low PCI complexity patients to 62.7 % for high PCI complexity patients. Currently there are varying definitions of complex PCI, which limit the generalizability of any trial of complex PCI. It would appear crucial to standardize the criteria to stratify the risk and establish the therapeutic strategy appropriately before PCI appropriately.
The present study revealed that, despite its known stronger platelet inhibitor effect, Ticagrelor does not reduce the rate of periprocedural MI and major myocardial injuries. It may be hypothesized that, in complex PCI in patients with stable coronary artery disease, the more significant atherosclerotic disease and higher calcium burden is responsible for increased periprocedural events, rather than thrombotic complications which more potent P2Y12 inhibition may reduce. Given the benefit of Ticagrelor in acute coronary syndrome, where the thrombotic milieu plays an important role, this seems a potential mechanism.
As with any trial, there is a number of important limitations; this was a sub-analysis and patients were not stratified by PCI complexity though the characteristics were well balanced between groups. The trial was an open label trial, though the CEC evaluated all events in a blinded fashion. Importantly the major bleeding rates were low occurring in 1 patient in each group at 48 hours and 3 patients in the complex PCI group vs 4 in the non-complex PCI group at 30 days.
The results of this trial do not support the routine use of Ticagrelor in elective PCI consistent with the current guidelines. Presently, the evaluation of procedural complexity and mitigation of any potential risks, i.e. avoiding side branch loss, no-reflow etc seems essential for reducing the periprocedural risk and improving the prognosis of patients undergoing complex PCI.
References
- Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009 Sep 10;361(11):1045–57.
- Silvain J, Lattuca B, Beygui F, Rangé G, Motovska Z, Dillinger JG, et al. Ticagrelor versus clopidogrel in elective percutaneous coronary intervention (ALPHEUS): a randomised, open-label, phase 3b trial. The Lancet. 2020 Nov 28;396(10264):1737–44.
- Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, et al. 2023 ESC Guidelines for the management of acute coronary syndromes: Developed by the task force on the management of acute coronary syndromes of the European Society of Cardiology (ESC). European Heart Journal. 2023 Oct 7;44(38):3720–826.





No comments yet!