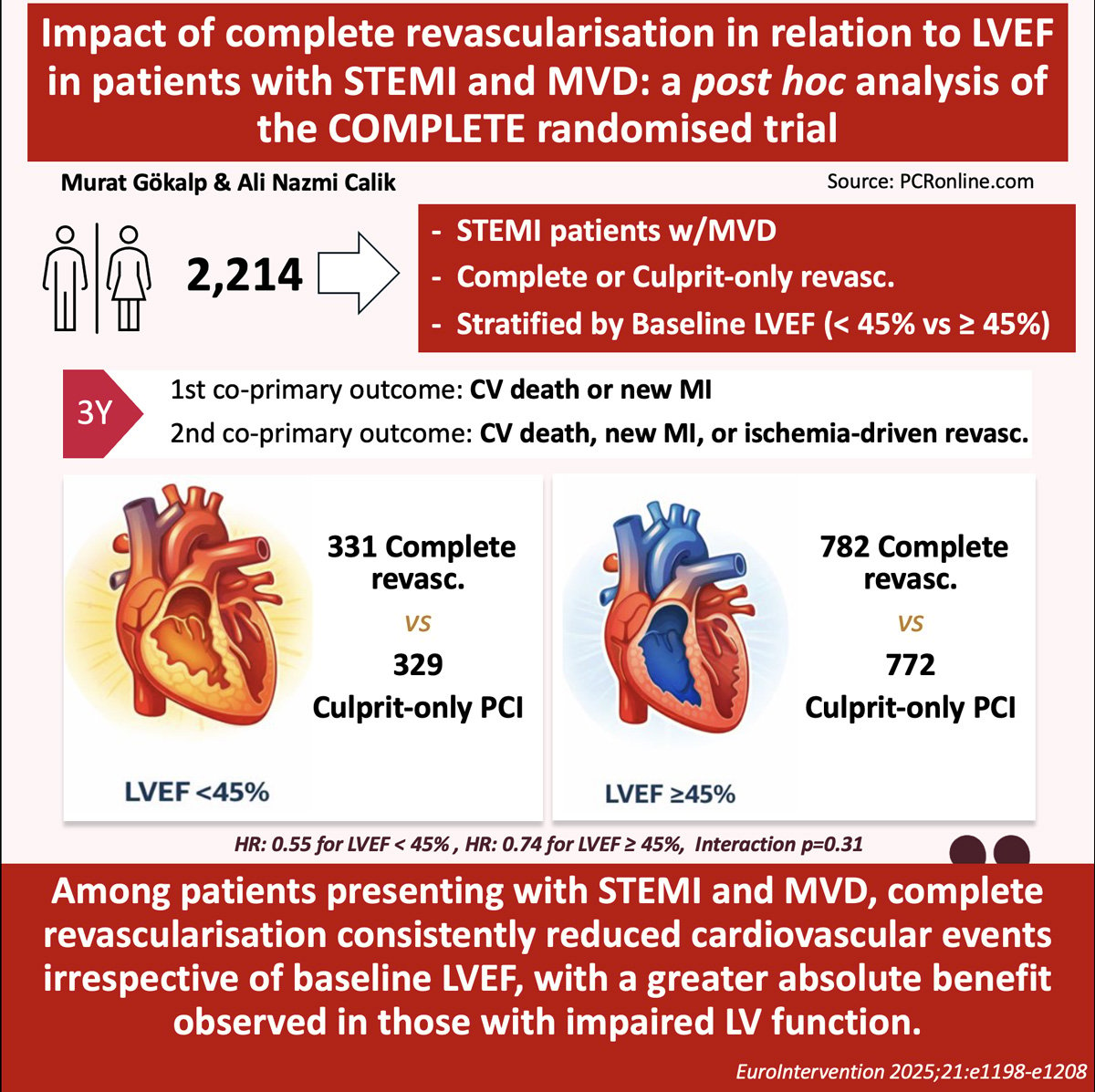
Impact of complete revascularisation in relation to left ventricular function in patients with ST-segment elevation myocardial infarction and multivessel disease: a post hoc analysis of the COMPLETE randomised trial
Selected in EuroIntervention Journal by M. Gökalp , A. N. Calik
This study represents a prespecified subgroup analysis of the COMPLETE randomised trial, a large, international, randomised controlled study comparing a strategy of complete revascularisation with culprit-only percutaneous coronary intervention (PCI) in patients presenting with ST-segment elevation myocardial infarction (STEMI) and multivessel coronary artery disease (MVD).
The present analysis specifically examines the impact of complete versus culprit-only revascularisation according to baseline left ventricular ejection fraction (LVEF). Among the overall study population, baseline LVEF data were available for 2,214 patients, who were included to assess whether left ventricular function modifies the clinical benefit of a complete revascularisation strategy.
References
Authors
Denise Tiong, Natalia Pinilla-Echeverri, David A. Wood, Roxana Mehran, Robert F. Storey, Laurent Feldman, Raul Moreno, Sunil Rao, Warren J. Cantor, Robert Welsh, Kevin R. Bainey, Eric A. Cohen, Michael B. Tsang, Matthew Sibbald, Madhu K. Natarajan, Dilani Wijesena, Thenmozhi Mani, Helen Nguyen, John A. Cairns, Shamir R. Mehta
Reference
DOI: 10.4244/EIJ-D-25-00005 - 2025;21:e1198-e1208
Published
Published online e-edition - 20 October 2025
Link
Read the abstractReviewers
Our Comment
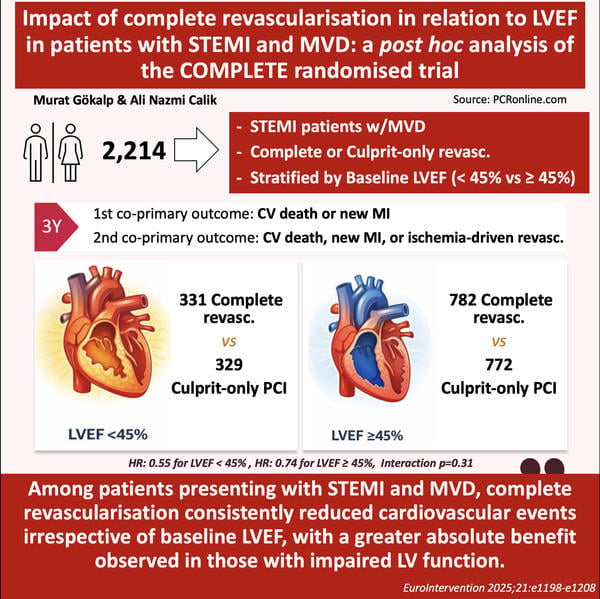
Infographic: key findings from the COMPLETE trial post hoc analysis
Why this study – the rationale/objective?
Left ventricular ejection fraction (LVEF) is among the strongest predictors of both short- and long-term outcomes after ST-segment elevation myocardial infarction (STEMI)1. Patients presenting with STEMI and multivessel coronary artery disease (MVD) who also have reduced LVEF constitute a particularly high-risk subgroup, with substantially higher rates of mortality, heart failure, and recurrent ischaemic events2.
Randomised trials, most notably the COMPLETE trial, have established that a strategy of complete revascularisation is superior to culprit-only percutaneous coronary intervention (PCI) in reducing cardiovascular death and myocardial infarction in STEMI patients with MVD3.
However, whether the magnitude of this benefit is modified by baseline left ventricular function has remained uncertain. In routine clinical practice, operators may be reluctant to pursue complete revascularisation in patients with impaired LVEF because of concerns related to procedural risk, haemodynamic instability, or limited myocardial recovery.
Given the limited evidence specifically addressing whether reduced LVEF alters the treatment effect of complete revascularisation, this pre-specified subgroup analysis of the COMPLETE trial was undertaken to determine whether the clinical benefit of complete versus culprit-only revascularisation is consistent across different levels of baseline LVEF, and to clarify whether patients with left ventricular dysfunction derive a similar or differential benefit from a complete revascularisation strategy.
How was it executed? The methodology
This analysis represents a prespecified subgroup evaluation of the COMPLETE randomised trial, a large, international, multicentre study enrolling patients with STEMI and multivessel coronary artery disease3. For the present analysis, only patients with documented baseline LVEF assessed during the index event were included.
In the parent trial, patients were randomly assigned after successful PCI of the infarct-related artery to either a strategy of complete revascularisation or culprit-only PCI. Complete revascularisation consisted of PCI of all angiographically significant non-culprit lesions, performed either during the index hospitalisation or shortly after discharge.
Eligible patients were required to have at least one significant non-culprit lesion suitable for PCI in a vessel with a reference diameter of at least 2.5 mm. Non-culprit lesions were considered significant based on angiographic severity or fractional flow reserve assessment. Patients with planned non-culprit intervention prior to randomisation, prior coronary artery bypass graft surgery, limited life expectancy, or factors precluding long-term follow-up were excluded.
Clinical outcomes were analysed according to baseline LVEF categories (< 45 % versus ≥ 45 %), with additional analyses using commonly applied LVEF strata (≤ 35 %, 36–49 %, and ≥ 50 %). The first co-primary outcome was the composite of cardiovascular death or new myocardial infarction, and the second co-primary outcome was the composite of cardiovascular death, new myocardial infarction, or ischaemia-driven revascularisation.
What is the main result?
Among the 4,041 patients enrolled in the COMPLETE trial, baseline LVEF was available in 2,214 patients and formed the population for this analysis3. Of these, 660 patients had an LVEF < 45 % and 1,554 had an LVEF ≥ 45 %. As anticipated, patients with reduced LVEF exhibited a higher overall risk profile and experienced substantially higher rates of cardiovascular events compared with those with preserved LVEF.
Complete revascularisation reduced the incidence of the first co-primary outcome in both LVEF groups. In patients with LVEF < 45 %, event rates were 3.0 % per year with complete revascularisation compared with 5.5 % per year with culprit-only PCI (hazard ratio [HR] 0.55, 95 % confidence interval [CI] 0.36–0.86). In patients with LVEF ≥ 45 %, corresponding rates were 2.4 % versus 3.2 % per year (HR 0.74, 95 % CI 0.52–1.04), with no significant interaction between treatment strategy and LVEF.
Consistent findings were observed for the second co-primary outcome, with a reduction in events across both LVEF categories. Additional analyses using finer LVEF strata (≤ 35 %, 36–49 %, and ≥ 50 %) similarly demonstrated no evidence of heterogeneity in treatment effect. While patients with reduced LVEF experienced higher absolute event rates, the relative benefit of complete revascularisation was preserved irrespective of baseline left ventricular function.
Critical reading and the relevance for clinical practice:
This prespecified subgroup analysis of the COMPLETE trial provides important insights into the role of baseline left ventricular function when determining revascularisation strategy in STEMI patients with multivessel disease. As expected, reduced LVEF was associated with markedly higher rates of mortality, heart failure, and recurrent ischaemic events. The central and clinically relevant finding, however, is that the relative benefit of complete revascularisation over culprit-only PCI was consistent across all LVEF groups, with no evidence that impaired ventricular function attenuates its effectiveness.
In daily practice, concerns regarding procedural risk and haemodynamic instability often lead to a more conservative, culprit-only approach in patients with reduced LVEF. The present analysis challenges this paradigm by demonstrating that impaired left ventricular function should not be considered a reason to withhold complete revascularisation. On the contrary, because of their higher baseline risk, patients with reduced LVEF derive a numerically greater absolute benefit from a complete strategy.
These findings are consistent with prior observations by Halkin et al., who demonstrated that reduced LVEF after acute myocardial infarction is associated with increased early and late mortality, particularly in the first months following the index event4. In the present analysis, an early excess of adverse events was similarly observed among patients with reduced LVEF when complete revascularisation was not achieved, especially in those with more severe ventricular dysfunction (≤ 35 %).
Comparison with the CULPRIT-SHOCK trial highlights important contextual differences. CULPRIT-SHOCK enrolled patients with cardiogenic shock and demonstrated improved short-term survival with a culprit-only strategy5. However, only a minority of patients in the multivessel PCI arm achieved complete revascularisation, and very high early mortality limited longer-term assessment. In contrast, COMPLETE enrolled haemodynamically stable STEMI patients, achieved complete revascularisation in the vast majority, and demonstrated that the benefit of a complete strategy emerged over longer follow-up. These differences underscore that findings from the shock setting should not be extrapolated to stable STEMI patients with multivessel disease.
Conclusion
This analysis reinforces complete revascularisation as the preferred strategy in haemodynamically stable STEMI patients with multivessel coronary artery disease, irrespective of baseline LVEF. Rather than identifying a subgroup in whom revascularisation should be limited, reduced left ventricular function identifies patients at higher absolute risk who stand to gain the greatest benefit from a complete revascularisation strategy.
References
- Halkin A, Singh M, Nikolsky E, Grines CL, Tcheng JE, Garcia E, et al. Prediction of mortality after primary percutaneous coronary intervention for acute myocardial infarction: the CADILLAC risk score. Journal of the American College of Cardiology. 2005;45(9):1397-405.
- Lansky AJ, Goto K, Cristea E, Fahy M, Parise H, Feit F, et al. Clinical and angiographic predictors of short-and long-term ischemic events in acute coronary syndromes: results from the Acute Catheterization and Urgent Intervention Triage strategY (ACUITY) trial. Circulation: Cardiovascular Interventions. 2010;3(4):308-16.
- Mehta SR, Wood DA, Storey RF, Mehran R, Bainey KR, Nguyen H, et al. Complete revascularization with multivessel PCI for myocardial infarction. New England Journal of Medicine. 2019;381(15):1411-21.
- Halkin A, Stone GW, Dixon SR, Grines CL, Tcheng JE, Cox DA, et al. Impact and determinants of left ventricular function in patients undergoing primary percutaneous coronary intervention in acute myocardial infarction. The American journal of cardiology. 2005;96(3):325-31.
- Thiele H, Akin I, Sandri M, Fuernau G, de Waha S, Meyer-Saraei R, et al. PCI strategies in patients with acute myocardial infarction and cardiogenic shock. New England Journal of Medicine. 2017;377(25):2419-32.





No comments yet!