22 Oct 2019
An NSTEMI case due to a severe LM calcific sub-occlusive stenosis
Euro4C Case
Author
Let’s exchange opinions on this case. This could happen to you tomorrow…
Pre-hospital clinical history
- 85-year-old female
- 3 pregnancies and natural deliveries
- Negative previous medical or surgical history
- Hypertensive under medical therapy (diuretic and ACE-inhibitor)
- Calls EMS for chest pain and shortness of breath
- At FMC BP: 95/60mmHg HR: 80bpm
- ECG tele-transmitted to our ICU

ECG at admission at the ICU. Minimum ECG changes at presentation with slight ST segment depression in V5-V6 precordial leads and 1mm ST elevation in aVR (arrows)
At hospital admission
- eGFR 40 ml/min/m2; hemoglobin: 12.3mg/dL
- Echocardiogram: EF 45%, large area of inferolateral hypokinesia
- First troponin «T» measurement: 927
- GRACE risk score calculation: 228 (21.4% in hospital mortality)
- Ongoing chest pain despite medical therapy with nitrates, and heparin
- Decision for immediate angiography
- Medical therapy: UFH, ASA, ticagrelor pre-loading, mild sedation
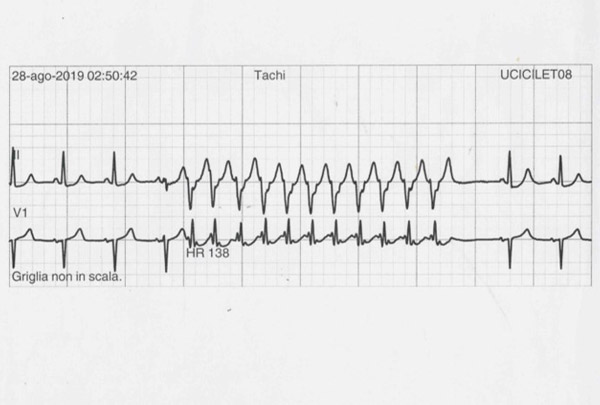
While waiting coronary angiogram

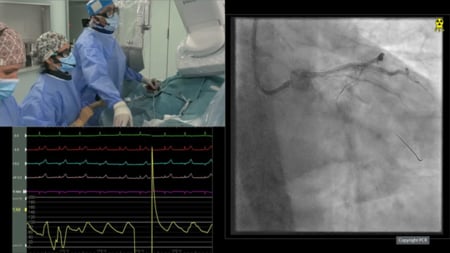
Invasive BP during coronary angiogram
Porcelain aorta and sub-occlusive stenosis of the ostial LM with bulky calcified plaque. CTO of the mid LAD.
Colateral circulation to the left coronary system from the RCA.
The radial access for the diagnostic angiography failed because of small artery, low pulse and spasm; therefore the operator converted to the femoral access.
Heart Team discussion in the cathlab
SYNTAX score: 39
SYNTAX SCORE II
- PCI
SYNTAX Score II: 51.6
PCI 4 Year Mortality: 35.1% - CABG
SYNTAX Score II: 43.0
CABG 4 Year Mortality: 18.9%
EuroSCORE-II: 18%
Logistic EuroSCORE: 27%
STS: 12
Hypokinesia of the postero-lateral wall (short axes) and apical-lateral (long-axes), that correlates with the lateral ischemia observed at the ECG.
Both, echo and ECG suggest the left circumflex territory as the most likely “acute culprit lesion”. The LAD territory appears to be well supplied by the collateral circulation
EBU 3.6 6F guiding catheter no MCS
Second RA with 1.75mm burr
NC balloon 3.0x20mm at 18 atm and Synergy EES 4.0x16mm in aorto-ostial LM position
Post procedural hospital course
- No peri procedural complications
- Peak troponin rise: 3475, (2992 the day after)
- Medical therapy at discharge: clopidogrel 75mg, ASA 90mg, bisoprolol 1.25mg, ramipril 5mg, pantoprazol 30mg.
- Clinical follow-up scheduled at 1, 6 and 12 months.
- One month follow-up obtained: asymptomatic, in NYHA class I

ECG at discharge






14 comments
Great case! 1/ In my opinion surgery is not a reasonable option, we would certainly choose PCI for this 85 yo lady 2/ This case has to be treated ad hoc, the situation has to be fixed when the patient leave the cath-lab 3/ A mechanical circulatory support should to be initiated before starting the procedure: we would choose IABP associated with continuous infusion of noradrenaline to achieve a systolic BP > 120 mmHg before beginning the PCI. Thus, we would implant the IABP and a central venous line in the left groin. IMPELLA would be probably a great option, but for cost reason, the use of this expansive and not reimbursed device, is in our institution limited to patient < 75 yo. ECMO seems not reasonable. 4/ Our strategy would be to focus on the culprit lesions (according to the culprit shock trial) treating LM and the Circumflex artery: We would use a 6 Fr 3.5 Extra Back Up guiding catheter with side holes, and advancing quickly distally in the circumflex artery a standard 0.014 guidewire in order to limit the drop pressure positioning the catheter at the ostium of the LM. 5/ We would start treating the left main, with a small semi-compliant balloon 2.5x12 mm to “test the lesion”. If the lesion cracks, we would pre-dilatate more aggressively the LM. Before stenting the LM, we would pre-dilate progressively and aggressively the Circumflex. If the small balloon does not cross the lesion of the LM, or if the balloons do not expand properly in the lesions of the LM or the circumflex, we would use RA with a 1.5 mm burr. For both lesions, we would choose stents with good radial force and post dilate the stents with NC balloon. As the LM lesion is ostial, it seems not necessary to treat the distal left main bifurcation. 6/ We would leave the chronic total occlusion of the LAD on medical treatment. 7/ If the patient is stable at the end of the procedure, we would remove the IABP and close both groins with Proglides.
Good night to everyone. First of all, despite the rates of calculated expected mortality with PCI and CABG, with the age of this woman, I don´t believe that too many of us will think in surgery. Second, if the anterior wall seems to be supplied by the collaterals from the RCA, I would focus in the left main and circumflex. The LM lesion is short and the vessel size is really large. My approach would be to advance the wire to the CX and a short inflation with a 2.5 mm balloon in the LM, given the severity of the lesion. After that I would use a 4 x 10 mm Wolverine or any other dedicated balloon to prepare the lesión and continue with the CX, performing predilatation and short 3.5 mm DES. Finally, I would use IVUS to see the size of the LM and use for example a 4 x 8 Synergy, Xicience Sierra o 4 x 9 Onix stent up to 5.75 mm, using postdilatation with an Emerge NV of 5.5 in case of need.
Good morning to everyone. First of all, despite the rates of calculated expected mortality with PCI and CABG, with the age of this woman, I don´t believe that too many of us will think in surgery. Second, if the anterior wall seems to be supplied by the collaterals from the RCA, I would focus in the left main and circumflex. The LM lesion is short and the vessel size is really large. My approach would be to advance the wire to the CX and a short inflation with a 2.5 mm balloon in the LM, given the severity of the lesion. After that I would use a 4 x 10 mm Wolverine or any other cutting balloon and continue with the CX, performing predilatation and short 3.5 mm DES. Finally, I would use IVUS to see the size of the LM and use a 4 x 8 Synergy stent ut to 5.75 mm, using postdilatation with an Emerge NV of 5.5 in case of need
Very interesting case. LM stenosis is tight, highly calcified and eccentric. My first treatment option is RA as with balloon lesion preparation probably the stent would not be well apposed and expandend at LM ostium. LVEF is 45% so MCS only if neeeded.
Nice result of a complex case. The lesion was even more difficult to cross than it might be expected, given the fact that it was not possible to advance a Corsair or 1,1 mm balloon. With this situation, the chances are limited to RA. Nice choice to start with a 1.25 and later to step up to a 1.75. Congratulations for the final result.
Did you think to do anything with LAD in a stage procedure?
Real life case! Thank you for sharing it with us. Some comments. 1/ Surgery? It´s an unstable patient with rest symptoms despite optimal medical treatment and you got it in your cath lab. 2/ Surgery? In my Institution surgeons do not treat acute NSTEMI patients. 3/ Surgery? Will surgeons perform complete revascualrization? With or without bump? 4/ MCS: I´ll not use it as patient has mild LV dysfunction. In our experience elderly patients with chronic disease tolerate these procedures. 5/ Initially RA? Not in this case because the baseline TIMI flow is impaired. If the small balloons do not cross (as in this case) then yes: Absolutely agree: small 1.25 mm burr and then step-up to a 1.75 mm. 6/ I will also use a cutting balloon becasuse is a large LM and bigger burr we can use never will really modify (break) completely the plaque to ensure the appropiate large stent deployment. 7/ Shockwave: it will not progress directly. I do not have experience in LM NSTEMI patients: could it compromise side branch (LCX)? 8/ LAD CTO: I´ll treat it in a staged procedure, surely at least 1 month later. It´s not a hurry: anterior wall motion is normal.
9/ I think once we open the LM and imove the flow an imaging technique will help us in our decisions; 10/ After restoring coronary flow, I´ll treat before mid LCX than ostial LM. Look forward Reading your comments
Congratulations, great case and great final result! Two questions: - why you didn't perform IVUS after RA? - did you use a 6 Fr. guiding catheter with 1.75 mm burr?
Thank you for your comments. This was certainly a demanding case... We "formally" showed the case to the surgeon, by heart team policy, but this is rather a PCI case in centers with adequate training and dedicated technology to afford all the expected challenges. In a different interventionakl setting, surgery may be the only option. No way to cross with ballon or even a microcatheter ! The only chance was RA, and being a left main, better always starting with a small one, then upsize to the 1.75. All the rest was quite easy. To answer yoru questions: YES, the 1.75mm burr goes smoothly throught the 6F guiding (Medtronic) from the radial access. We did not consider to implant MCS given the preserved LV function, but we did iliac angio because we considered it as a stand-by in case of deterioration. No way to cross with a lithotripsy balloon such a stenosis! It migth be an option after RA if balloons do not open fully. I agree that opening the CTO of the LAD may be not be the case in an old lady with preserved LV function. She did not complain from angina before the NSTEMI....! Embarking in a CTO after a left main like this in the acute NSTEMI setting might create more harm than benefits.... You are right, IVUS "should be performed" but the operator was confident with the final result afte RA and high pressure balloon dilatation and decided to spare some money.... Thanks a lot for your comments!!!
Great case! The treatment of a so tight, eccentric and calcified lesion of the ostial LM presenting with an acute coronary syndrome requires not only technical skills but also clinical judgment to "tailor" the treatment on the single patient, balancing harms and benefits.
Congratulations, very great case and final result!!! I agree with rota step up technique maybe followed cutting balloon. It would have been interesting to have IVUS image.
What’s about LAD?
congratulation, fantastic ...... for the final result if the patient was stable, no worsening of ECG, is it possible to give anticoagulant for five days, and do angiogram??