18 Sep 2019
How should I treat with rotational atherectomy a TAVI candidate
Euro4C Case
Author
Let’s exchange opinions on this case. This could happen to you tomorrow…
Patient history
- 84-year-old woman in good general condition
- Severe AVS on medical management
- Chronic atrial fibrillation
- Admitted with heart failure and chest pain
- Minimum troponin rise with no specific ECG changes
- Moderately impaired LV ejection fraction (EF 40%), Mean AG 48mmHg
- Moderate impairment of the GFR (40ml/m/m2)
Coronary angiography
Given the presence of coronary stenosis in the three coronary vessels, a physiological assessment of the severity of the lesion was performed in the three main arteries.
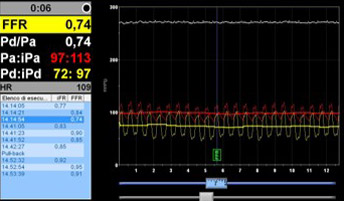
FFR in the LAD
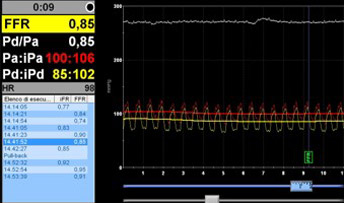
FFR in the LCx
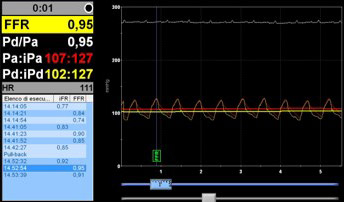
FFR in the RCA
How Should I treat?
Considerations before deciding to use PCI or Rotational Atherectomy (RA), in favor of RA: large amount of calcium, length of the long lesion, very tight MLD of the stenosis, presence of two important side branches
Immediately after the valve implantation (during the same procedure), the left coronary artery was selectively engaged with a 6Fr guiding catheter ….
After selective catheterization of the LM with a 6Fr guiding catheter (3.5 Medtronic EBU), a floppy Rotawire was positioned in the distal LAD. The 1.25mm rota burr was ussed. The lession was extremely resistant to cross.
It took more than 13 minutes to cross the lession with the burr, and in the end a burr speed 180.000 was used. Of note, neither bradicardia, nor hypotension occurred during RA.
After effective RA, a 2.5x20mm NC balloon was inflanted at 14atm
A 3.0x22mm ZES Resolute Onyx was positioned in the proximal LAD and subsequently post dilated with a NC balloon
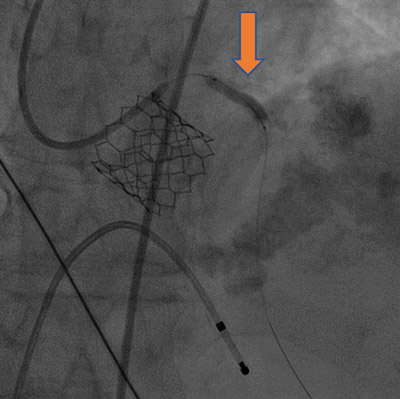
After stenting and post-dilatation the vessel showed a good angiographic aspect, and interestingly, both side branches - the diagonal and the septal - showed no impairment of flow despite the diffuse disease.
The favorable effect of RA on the side branches, reducing the risk of occlusion after stenting, is confirmed in this case.
The percutaneous vascular accesses were closed and the temporary PM removed after the procedure.
The patient was monitored during 48h and discharged on post-procedural day 3°.
Oral anti-coagulation was associated to DAPT with clopidogrel and ASA for one month. Then ASA was withdrawn and clopidogrel continued for other 5 months.
After six months only OAC was continued and after 2 years follow-up She is asymptomatic and in NYHA class I.
Key learning messages
Physiologic assessment of coronary lesions in AS has not been validated, but it makes sense as an alternative to extensive stenting in elderly patients. This is common practice in our Institution and is based on our previous and ongoing studies on this matter (1,2,3,4,5,6,7)
RA may facilitate PCI and provides a better result compared to balloon PCI in elderly patients with extensice coronary calcifications. Performing rotational atherectomy after TAVI -and not before- may be perceived as technically more challenging because of the catheterization of the coronaries through the valve, but this certainly reduces the hemodynamic risk of the potential complications of PCI in an aged patient with severe aortic stenosis.
For this reason our group -in the last 5 years- has performed RA generally after TAVI and not before, without complications (8).
"Thank you for your comments.
Indeed, there is absolutely NO evidence available on how to manage elderly patients with severe AS selected for TAVI and having associated coronary artery disease. The decision becomes even more difficult when the treatment of the coronary lesions is challenging because of the calcifications.
We have no answers to the most simple questions that you have raised in your comments: to treat or not to treat asymptomatic stenosis? to treat before or after TAVI? same procedure or deferred? rotational atherectomy as a first attempt or after balloon?
What we know is that CAD is often present in AS patients and that TAVI is being offered as an option to younger and more active patients, therefore the management of CAD is gaining more importance.
Our case provides a diagnostic alternative, based on the physiologic assessment of the lesion's significance, and demonstrated the feasibility of performing rotational atherectomy after valve implantation, in the same procedure.
All the rest about the management of this fascinating clinical setting is to come…"
Flavio Ribichini for Euro4C
References
- Scarsini R, Cantone R, Venturi G, De Maria GL, Variola A, Braggio P, Lunardi M, Pesarini G, Ferdeghini M, Piccoli A, Feola M, Kharbanda RK, Banning AP, Ribichini F. Correlation between intracoronary physiology and myocardial perfusion imaging in patients with severe aortic stenosis. Int J Cardiol. 2019 Oct 1;292:162-165. doi: 10.1016/j.ijcard.2019.04.050. Epub 2019 Apr 17. PMID: 31029497
- Scarsini R, De Maria GL, Di Gioia G, Kotronias RA, Aurigemma C, Zimbardo G, Burzotta F, Leone AM, Pesarini G, Trani C, Crea F, Kharbanda RK, De Bruyne B, Barbato E, Banning A, Ribichini F. The Influence of Aortic Valve Obstruction on the Hyperemic Intracoronary Physiology: Difference Between Resting Pd/Pa and FFR in Aortic Stenosis. J Cardiovasc Transl Res. 2019 May 22. doi: 10.1007/s12265-019-09890-5. PMID: 31119562
- Scarsini R, Pesarini G, Zivelonghi C, Piccoli A, Ferrero V, Lunardi M, Gottin L, Zanetti C, Faggian G, Ribichini F. Physiologic evaluation of coronary lesions using instantaneous wave-free ratio (iFR) in patients with severe aortic stenosis undergoing transcatheter aortic valve implantation. EuroIntervention. 2018 Jan 20;13(13):1512-1519. doi: 10.4244/EIJ-D-17-00542. PMID: 28846545 Free Article
- Scarsini R, Pesarini G, Zivelonghi C, Piccoli A, Ferrero V, Lunardi M, Barbierato M, Caprioglio F, Vassanelli C, Ribichini F. Coronary physiology in patients with severe aortic stenosis: Comparison between fractional flow reserve and instantaneous wave-free ratio. Int J Cardiol. 2017 Sep 15;243:40-46. doi: 10.1016/j.ijcard.2017.05.117. PMID: 28610962
- Scarsini R, Pesarini G, Lunardi M, Piccoli A, Zanetti C, Cantone R, Bellamoli M, Ferrero V, Gottin L, Faggian G, Ribichini F. Observations from a real-time, iFR-FFR "hybrid approach" in patients with severe aortic stenosis and coronary artery disease undergoing TAVI. Cardiovasc Revasc Med. 2018 Apr - May;19(3 Pt B):355-359. doi: 10.1016/j.carrev.2017.09.019. PMID: 29113864
- Di Gioia G, Scarsini R, Strisciuglio T, De Biase C, Zivelonghi C, Franco D, De Bruyne B, Ribichini F, Barbato E. Correlation between Angiographic and Physiologic Evaluation of Coronary Artery Narrowings in Patients With Aortic Valve Stenosis. Am J Cardiol. 2017 Jul 1;120(1):106-110. doi: 10.1016/j.amjcard.2017.03.250. PMID: 28483203
- Pesarini G, Scarsini R, Zivelonghi C, Piccoli A, Gambaro A, Gottin L, Rossi A, Ferrero V, Vassanelli C, Ribichini F. Functional Assessment of Coronary Artery Disease in Patients Undergoing Transcatheter Aortic Valve Implantation: Influence of Pressure Overload on the Evaluation of Lesions Severity. Circ Cardiovasc Interv. 2016 Nov;9(11). pii: e004088. PMID: 27803040
- Mattia Lunardi, Gabriele Pesarini, Roberto Scarsini, Michele Pighi, Carlo Zivelonghi, Valeria Ferrero, Leonardo Gottin & Flavio Ribichini (2019) Coronary Rotational Atherectomy in Patients Treated with Transcatheter Aortic Valve Implantation, Structural Heart, 2019. DOI: 10.1080/24748706.2019.1646947








5 comments
I think Rota PCI before Tavi will be easier than Tavi then pci.
I would definitely choose PCI + TAVI, given the age and the excellent results of the percutaneous approach in aortic stenosis. The case is perfect for rotational atherectomy due to the calcium, length of lesion and the presence of a large diagonal branch. My choice would be 1,5 mm burr, dilatation with 2.5 mm along the whole lesion except the segment where the take-off of the diagonal to avoid plaque shift and finally deploy a 2,5 x 48 mm stent (in our center it would be Xience) with POT with a 3 x 12 mm balloon proximal to the diagonal. Finally I would program AAS 100 + 75 mg of Clopidogrel and 1-6 months of triple therapy with a NACO (depending on the HAS-BLED). I had recently a case with stent thrombosis with strategy PIONEER and besides that, in that study the subgroup of patients with complex PCI had a higher risk: the high limit of 95% CI for ischemic events in multivessel, bifurcation and long stents was 5.69, 11.48 and 6.41 (J Am Coll Cardiol Intv 2018; 11: 626–34) and in this case the lesion is long and with a bifurcation. If we had doubts about the vessel diameter we can use IVUS guidance.
I think I would prefer to perform PCI before TAVI due to concern about difficulties of left main engagement trought aortic prosthesis struts (but authors resolved this issue using a Sapien valve). On the other hand, a complex PCI of proximal LAD in presence of severe AS could have catastrophic complications. What if FFR positive even in LCX or RCA? Surgery? Step-by-step PCI before TAVI?
PCI and TAVI on the same procedure; Prepare all the set up for TAVI, rotablate the LAD (1.25mm and possibly 1.5 mm) and after stenting the LAD proceed with TAVI. The issue here is to be able to do the TAVI urgently if needed, so, have everything ready for the TAVI (i.e. measurement,access) before proceeding with the rotablation
Because of slightly decreased eGFR I would rather choose two separate procedures for complete treatment: first PCI and then TAVI. With AG of 48mmHg and EF of 40%, I would prefer PCI of LAD as a first intervention