When it’s (really) tight
#CardioTwitterCase originally published on Twitter
A 71-year-old woman was referred for coronary angiography. She underwent SAVR for AS related to bicuspidia 6 months before, and subsequently suffered from angina and increasing dyspnea 4 months after the intervention...
This case was originally published on Twitter by @nicolasamabile
Case description
A 71-year-old woman was referred to our center for coronary angiography.
She underwent SAVR for aortic stenosis related to bicuspidia 6 months before (Magna Ease 23 mm valve implantation)
The initial evolution was uneventful, but she subsequently suffered from angina and increasing dyspnea 4 months after the intervention.
Control TTE revealed dramatically decreased LV systolic function (LVEF = 25 %), with severe antero-apical hypokinesia (Video 1)
Other medical conditions included heparin‐induced thrombocytopenia and aspirin allergy.
Coronary angiography revealed de novo proximal LM sub-occlusion with Rentrop 3 collateral flow arising from the RCA (Videos 2-3).
The LM could not be correctly cannulated with the JL 3.5 diagnosis catheter. The cause of the stenosis appeared to be external vessel compression.
Cardiac CT scan confirmed the presence of a paraostial LM kink related to the presence of the aortic bioprosthesis (Figures 1, 2 and 3).
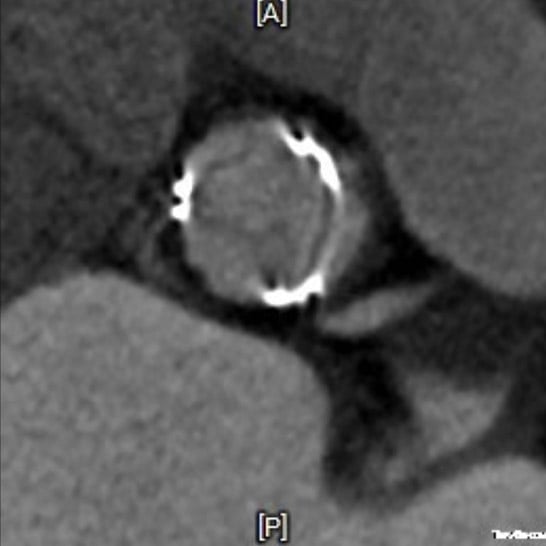
Figure 1
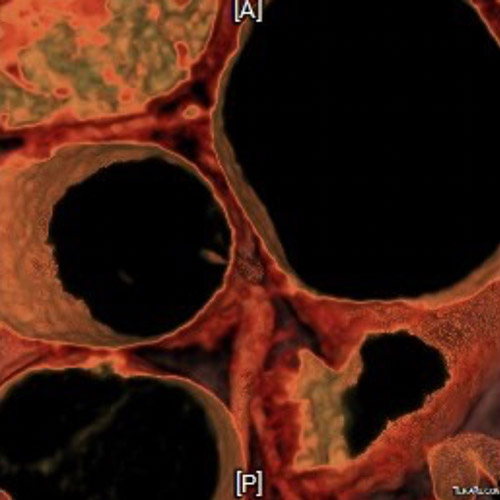
Figure 2

Figure 3
Cardiac MRI showed viable hibernating myocardium in the anterior and lateral walls, suggesting the interest of revascularization.
The heart team decided to propose the patient LM PCI with left ventricular assistance Impella® support given the very high risk of the procedure.
Aspirin desensitization was successfully conducted, and the use of heparin bolus during the procedure was allowed, as the anti-PFA antibodies dosage was negative.
The procedure was performed through a double-femoral access. Impella was inserted through the bioprosthesis, and LM was non-selectively catheterized with an EBU 3.5 7fr GC.
The lesion was crossed with a S shaped Sion blue wire (Figure 4).
Lesion preparation was performed using a 2.0 x 10 mm balloon: the stenosis was progressively dilated (Video 4) but showed immediate recoil (Figure 5).
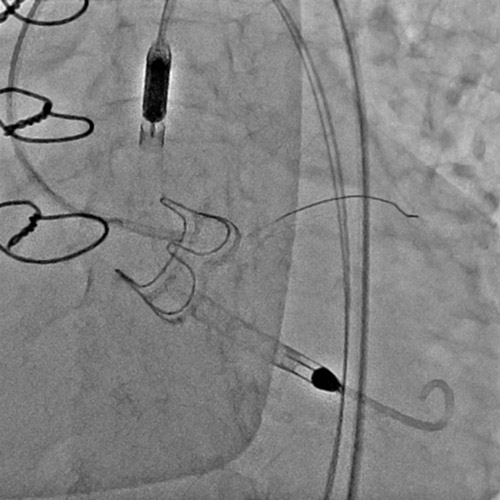
Figure 4

Figure 5
The post-predilation IVUS analysis showed external compression, potentially involving valve frame (Video 5), and no sign of atherosclerosis.
Thus, we performed a second predilation with a 4 x 12 mm balloon, and implanted a 5.0 x 16 mm SYNERGY MEGATRON EES (16 ATM / 30s) with minimal recoil (Video 6).
We post dilated the stent with repeated 5.0 x 12 NC balloon inflations (Figure 6).
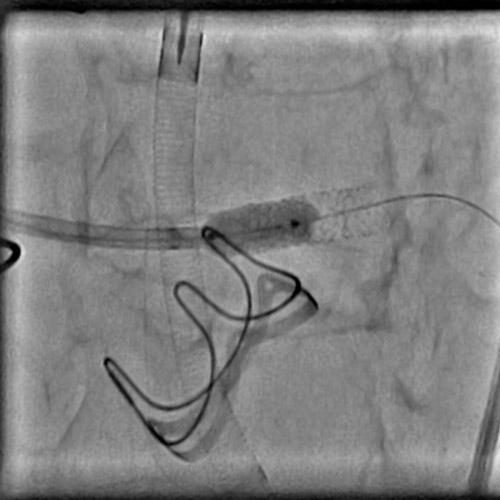
Figure 6
The final angio result (Video 7) and IVUS aspect were satisfactory; the left ventricular assistance was withdrawn at the end of the procedure.
Control TTE revealed LVEF improvement 4 days after PCI (LVEF = 40 %). Clinical signs disappeared in the following days, and subsequent evolution was uneventful.
Final remarks
External LM compression / kink remains an exceptional complication of surgical AVR. The progressive recovery of LV function post-revascularization supports the concept of hibernating ischemic myocardium.
PCI is an option in this situation, but remains a high-risk procedure. In this perspective, the therapeutical strategy should be discussed within the Heart Team. LV assistance could be proposed to minimize the risk of hemodynamic instability and allow longer inflations in the LM.
Original tweet and Twitter discussion
#talefromthechip 71 y-o woman / Uneventful SAVR 6 months before/ Recent severe dyspnea and LVEF=20% on control TTE (60% after surgery)@IMMontsourispic.twitter.com/FIwlCpaprH
— Nicolas Amabile (@nicolasamabile) February 26, 2023
Authors





No comments yet!