20 Apr 2022
Crash TAVI-in-TAVI complicated by coronary obstruction
Supported by the EuroIntervention Journal
Authors
Christopher J Allen1,2, Darshana Nair2, Martin John2, Tiffany Patterson 1,2
Case summary
A 54-year-old gentleman who underwent TAVI two years ago (26 mm Sapien 3 Ultra, Edwards Lifesciences, Irvine, CA, USA) presented with unstable angina and rapidly progressive breathlessness (New York Heart Association class IV) with ST-segment elevation in aVR and ST-depression in the lateral leads.
Coronary angiography demonstrated obstructive disease in the proximal left anterior descending (LAD) and circumflex arteries, alongside known right coronary artery (RCA) chronic total occlusion (CTO).
Despite successful two-vessel percutaneous coronary intervention, the patient progressively deteriorated into cardiogenic shock. Transthoracic echocardiography revealed a severely restricted aortic bioprosthesis (maximum velocity 4.0 m/s, peak gradient 65 mmHg, mean gradient 41 mmHg, aortic valve area 0.3cm2/m2) within the context of severe left ventricular systolic impairment (LVEF 15 %), with an akinetic RCA territory and severe hypokinesis elsewhere (Figure 1 A-B, Video 1), consistent with a diagnosis of severe structural valve degeneration1.
In view of the acute clinical course, including comparatively normal echocardiographic parameters three months prior, valve thrombosis was considered a potential aetiology, and systemic fibrinolysis commenced. His background, including porcelain aorta, critical arterial disease, with right below-knee amputation and end-stage renal failure requiring haemodialysis, rendered his surgical risk prohibitive (EuroSCORE II 72 %, STS-PROM 42 %).
After precipitous haemodynamic collapse requiring cardiopulmonary resuscitation (CPR), Heart Team's decision to salvage emergency TAVI was reached.
Multi-detector cardiac computed tomography (MDCT) planning was deemed unfeasible in view of the patient’s instability.
The patient entered the catheter lab on maximum ionotropic support with intermittent CPR ongoing. Valve-in-valve TAVI (26 mm Sapien 3 Ultra, Edwards Lifesciences, Irvine, CA, USA) was performed via right femoral arterial primary access, under transoesophageal echocardiographic (TOE) guidance (Figure 1C, Video 2).
Planned cerebral embolic protection from the right radial artery was abandoned due to acute vasoplegia.
Immediately post-deployment, the patient developed acute anterolateral tombstone ST elevation with angiographic evidence of dynamic, leaflet-related left main stem (LMS) obstruction (Figure 1D, Video 3).
The LMS was engaged with a 7Fr extra back-up coronary guide catheter with guide extension (Guideliner) and a balance middleweight wire positioned in the distal LAD.
After balloon pre-dilatation, overlapping 4.0 x 23 mm and 4.5 x 18 mm Zotarolimus-eluting stents were deployed from the proximal LMS extending proximally above the obstructing leaflet tissue (Figure 1E, Video 4) with restoration of coronary flow, immediate haemodynamic improvement and resolution of the ECG changes (Figure 1F, Video 5). TOE confirmed good valve function with no regurgitation (Video 6).
The post-procedure course was protracted, but the patient ultimately recovered with near-normalisation of left ventricular function and remains well.
Crash (emergency) TAVI-in-TAVI is feasible in patients with limited alternative options but demands vigilance for, and prompt management of complications.
Particular attention should be paid to native aortic valve leaflets when using balloon-expandable devices as, although initial TAVI did not cause coronary obstruction, placement of a second THV exerted further radial force likely resulting in annular deformation with native leaflet obstruction of the coronaries.
Supplementary Material
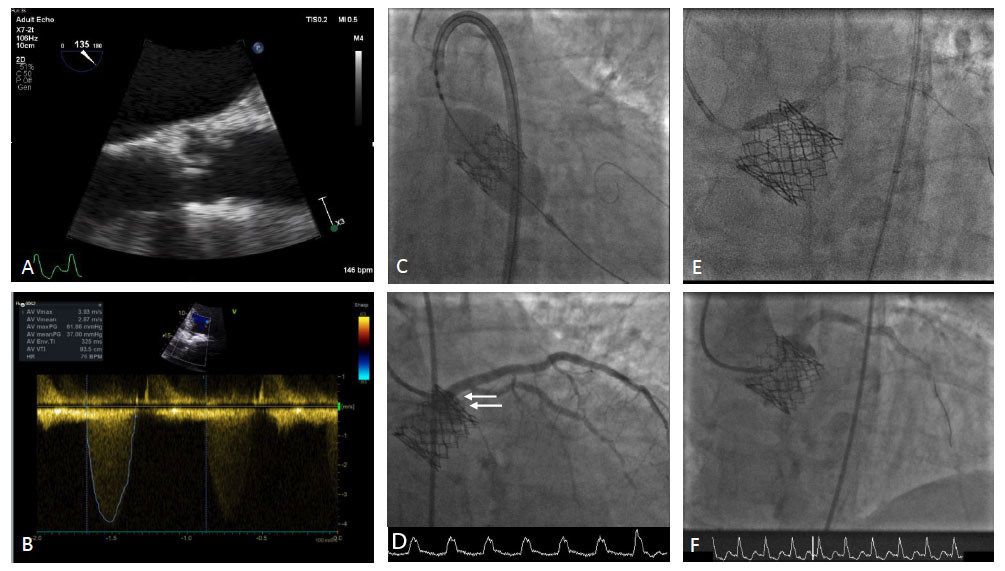
Figure 1 - A-B : Transthoracic echocardiography demonstrating severe degeneration of a 26 mm S3 Ultra transcatheter heart valve.
C : Treated with valve-in-valve deployment of a replacement 26 mm S3 Ultra.
D : Sub-occlusion of the LMS from dynamic leaflet obstruction, marked by radiolucent tissue external to stent frame (arrows) with resultant ST-segment elevation and haemodynamic deterioration.
E : Chimney stenting with overlapping 4.0 x 23 mm and 4.5 x 18 mm Zotarolimus-eluting stents.
F : Restoration of coronary flow with normalisation of ECG.
Conflict of interest statement
Dr Allen is supported by a British Heart Foundation Clinical Research Training Fellowship (FS/18/48/33745).
The other authors have no relevant conflicts of interest to declare.
References
- Capodanno D, Petronio AS, Prendergast B, et al. Standardized definitions of structural deterioration and valve failure in assessing long-term durability of transcatheter and surgical aortic bioprosthetic valves: a consensus statement from the European Association of Percutaneous Cardiovascular Interventions (EAPCI) endorsed by the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). European heart journal 2017;38:3382–3390.
Affiliations
- Cardiovascular Division, St. Thomas Hospital, King's College London, United Kingdom
- Department of Cardiology, Guys’ and St Thomas NHS Foundation Trust, United Kingdom







1 comment
Great save, so with all due respect to the difficult conditions you worked under: In hindsigt you might have expected this problem , as there seems to be a low sinus hight with the original Sapien at or just above the STJ, an issue that could have bee evaluated on the original pre TAVI CT, and coronary protected arranged prior to implantating second valve. Thus sinus sequestration as likely an explanation as problems with the old native valve leaflets. It is not clear if you stent though upper part of the first Sapien or externally to it, but would guess the latter, in order not to have stent struts impinging on the new Sapien valve material. Otherwise you must either have perforated the first Sapien valve that acts as a covered stent, or have been able to find a passage just above the original TAVI valve material though most cranial stent struts.?