Effective techniques for performing DCB angioplasty
A problem-solving step by step tutorial
Drug-coated balloon (DCB) angioplasty has become a valuable alternative to drug-eluting stents in treating coronary artery disease. To achieve optimal outcomes, proper lesion preparation and techniques to minimise drug loss are crucial.
This article highlights key steps and best practices for performing DCB angioplasty, ensuring effective drug delivery and improving patient outcomes.
Frequency of the problem:
Expert level:
Summary
In recent years, interest in and use of drug-coated balloons (DCBs) have significantly increased in interventional cardiology. Long-term follow-up from registries and randomised trials has reported a 2 to 4 % annual rate of target lesion failure beyond the first year with second-generation drug-eluting stents (DES), largely due to the presence of a permanent metal scaffold. This scaffold impairs vasomotion, prevents late lumen gain, and triggers inflammation and neo-atherosclerosis.
Landmark randomised trials have shown the effectiveness of DCBs in specific populations, such as those with de novo lesions in small coronary vessels or in-stent restenosis (ISR) of DES. Several ongoing randomised trials are now investigating the safety and efficacy of DCBs for de novo lesions in comparison to DES1,2.
The problem
Drug-coated balloons (DCBs) are semi-compliant balloons coated with an active drug embedded in a matrix. Upon inflation, the drug is transferred to the vessel wall, where it exerts its anti-proliferative effect. DCBs deliver the drug acutely within minutes through direct contact between the balloon surface and the arterial lumen.
However, one limitation of current DCBs is the significant drug loss during preparation and delivery, with first-generation paclitaxel-coated balloons losing up to 80 % of the initial loading dose. Several procedural factors, such as lesion preparation, transit time, inflation duration, and the DCB-to-artery ratio, influence the efficiency of drug transfer and retention within the vessel wall.
Principal idea
Proper lesion preparation, following a step-by-step approach to achieve ≤ 30 % residual stenosis, has become a crucial factor in the success of DCB angioplasty3. Simple techniques to minimize drug loss and optimize drug transfer and retention are also key to enhancing treatment outcomes.
Material needed
- Guiding catheter
- 0.014’’ guidewire
- Semi-compliant balloon
- Non-compliant balloon
- Drug-coated balloon
Step-by-step method
Step 1
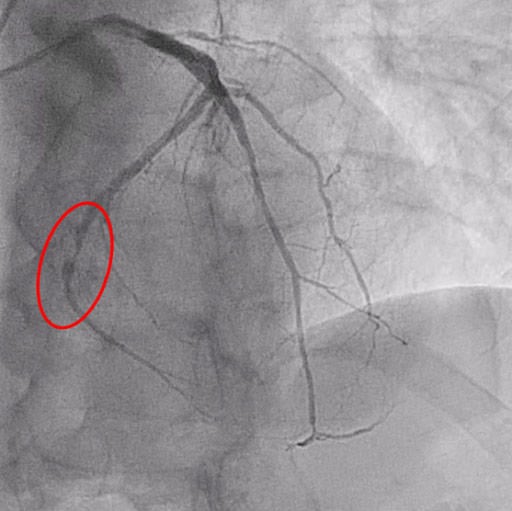
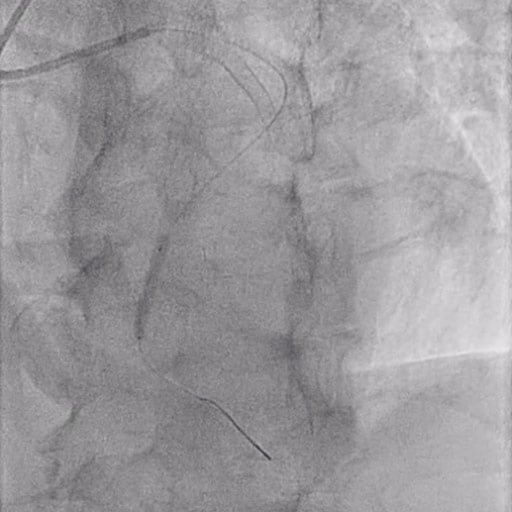
Figure 1: Critical PLCx stenosis
In the first phase, pre-dilatation is performed using semi-compliant or non-compliant balloons (vessel/device diameter ratio = 0.8-1) at nominal pressure.
A semi-compliant balloon 2.5 x 15 mm and a non-compliant balloon 3.0 x 15 were inflated up to 10 ATM and 12 ATM, respectively, to prepare the vessel.

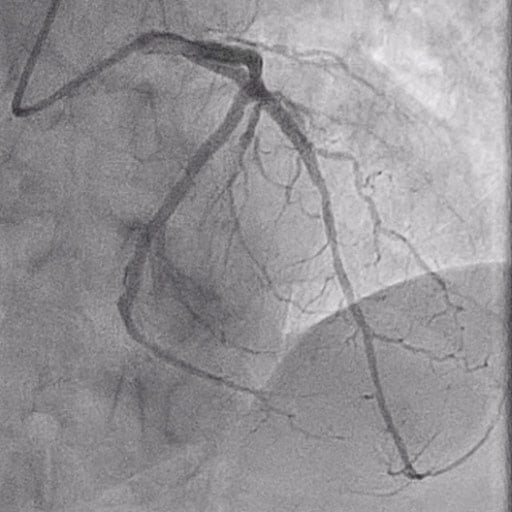
Figure 2: Lesion preparation
Step 2
In case of a sub-optimal result, further dilatations can be performed at higher pressures (16-18 ATM), or other devices such as scoring or cutting balloons, lithotripsy, and atherectomy may be used.
Step 3
Once a satisfactory result is achieved in lesion preparation (similar to stent-like outcomes), DCB angioplasty can be performed.
It is essential to handle the device carefully during preparation, avoiding contact with the balloon surface to prevent drug loss.
After positioning the device at the target lesion, inflate it to 6-8 ATM and maintain inflation for at least 1 minute.
In this case, a sirolimus drug-coated balloon catheter 3.0 x2 5mm was inflated for 1 min at 10 ATM.
If chest pain or ST-segment changes arise, consider performing two inflations of 30 seconds each, rather than a single inflation.
It's important to note that the DCB angioplasty phase is intended only for drug delivery, not for lesion dilation.
Therefore, the device should not be inflated at high pressures for dilating the lesion.
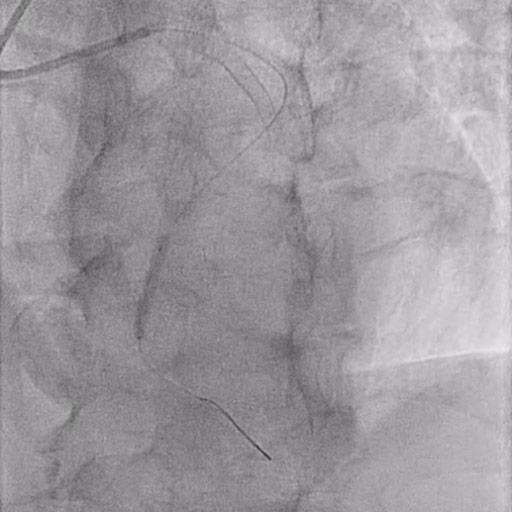
Figure 3: DCB inflation
Step 4
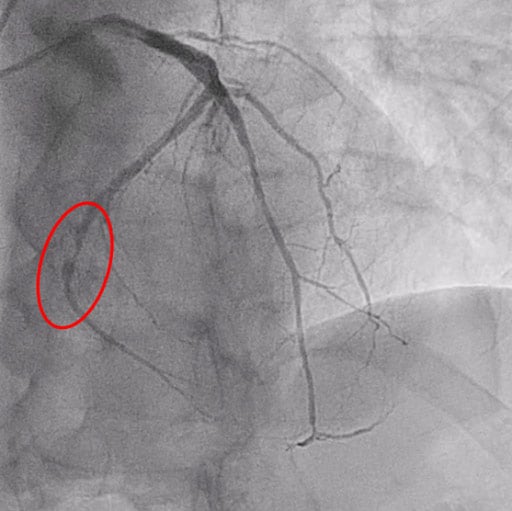
If the outcome is satisfactory, with no flow-limiting dissections, the procedure can be considered complete. However, if there is flow reduction and/or a significant dissection (type C or higher), vessel recoil > 30 % or fractional flow reserve ≤ 0.80, bailout stenting is recommended.
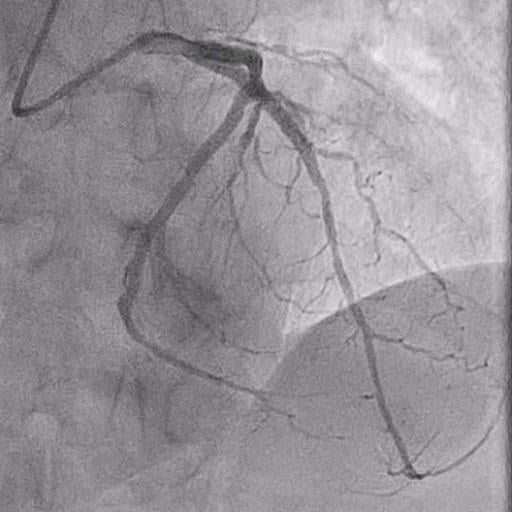
Figure 4: Final result
Points of specific attention
- The primary goal of DCBs is to deliver the drug to the affected vessel segment, making it essential to avoid drug loss during balloon preparation. It is important to prevent wetting, touching, or contact with other materials.
- To ensure optimal drug delivery to the lesion, the DCB should be the final device used. Avoid performing any post-dilatations after DCB angioplasty.
- The DCB is not designed to dilate the lesion. Inflate it to 4-6 ATM and maintain inflation for 1 minute, carefully avoiding dissections or other complications.
- Type A and B dissections generally indicate good lesion preparation and are typically not flow-limiting. However, a Type C or higher dissection should be treated with stent implantation.
References
- Greco A, Sciahbasi A, Abizaid A, Mehran R, Rigattieri S, de la Torre Hernandez JM, Alfonso F, Cortese B. Sirolimus-coated balloon versus everolimus-eluting stent in de novo coronary artery disease: Rationale and design of the TRANSFORM II randomized clinical trial. Catheter Cardiovasc Interv. 2022;100:544-552. doi: 10.1002/ccd.30358
- Spaulding C, Krackhardt F, Bogaerts K, Urban P, Meis S, Morice MC, Eccleshall S. Comparing a strategy of sirolimus-eluting balloon treatment to drug-eluting stent implantation in de novo coronary lesions in all-comers: Design and rationale of the SELUTION DeNovo Trial. Am Heart J. 2023;258:77-84. doi: 10.1016/j.ahj.2023.01.007
- Jeger RV, Eccleshall S, Wan Ahmad WA, Ge J, Poerner TC, Shin ES, Alfonso F, Latib A, Ong PJ, Rissanen TT, et al. Drug-Coated Balloons for Coronary Artery Disease: Third Report of the International DCB Consensus Group. JACC Cardiovasc Interv. 2020;13:1391-1402. doi: 10.1016/j.jcin.2020.02.043
A word from the reviewer - Ali Nazmi Calik
Effective lesion preparation is crucial for maximizing the benefits of drug-coated balloons (DCB). In calcified lesions where semi-compliant and non-compliant balloons may not yield satisfactory results, cutting or scoring balloons, along with adjunctive therapies like rotablation, laser or orbital atherectomy, and lithotripsy, is recommended to ensure optimal lesion preparation.
These ablative techniques can enhance the effectiveness of balloon angioplasty and improve the delivery of the drug to the vessel.
After lesion preparation, an optimal outcome before delivering the DCB should be confirmed by ensuring that:
- the predilatation balloon is fully inflated and appropriately sized for the vessel;
- the residual stenosis is < 30 %;
- the TIMI flow grade is 3; and
- there are no flow-limiting dissections (type C to F) or findings suggestive of thrombus.
When major dissections are suspected during an angiogram, intravascular ultrasound (IVUS) may be more effective than optical coherence tomography (OCT) in assessing the severity of the dissections while ensuring greater safety1.
Non-flow-limiting intimal dissections may not require intervention, but cases involving medial dissections, intramural hematomas, or extramedial injuries should be addressed with "bailout" stenting to ensure proper treatment.
Physilogical assessment following lesion preparation can provide valuable insights to support decision-making regarding the DCB-only approach.
While recognizing the limitations of the available data on the ideal FFR value after lesion preparation, FFR greater than 0.80 may serve as a reasonable threshold to proceed with DCB-only approach.
Finally, it is essential to remember that DCBs are generally more challenging to deliver than conventional balloons. This characteristic may necessitate enhanced catheter support to prevent delivery failures and the need to reinsert the same DCB.
Furthermore, most manufacturers advise against the reinsertion of the same DCB due to the loss of drug and carrier material that occurs upon contact with liquid.
- Kobayashi N, Mintz GS, Witzenbichler B, Metzger DC, Rinaldi MJ, Duffy PL, et al. Prevalence, features, and prognostic importance of edge dissection after drug-eluting stent implantation: an ADAPT-DES intravascular ultrasound substudy. Circ Cardiovasc Interv. 2016;9: e003553.
The Essentials - Drug-Coated Balloon
Authors






No comments yet!