Impella percutaneous ventricular assist device malrotation in social media: a call to action
The data from this study suggest that, from a SoMe perspective, correct Impella orientation is often overlooked, and that Impella malrotation is a common issue in real-world clinical practice, potentially associated with relevant complications.
Among percutaneous left ventricular assist devices (pVADs), the Impella (Abiomed, Danvers, MA, USA) trans-aortic, axial-flow pump is increasingly used for mechanical circulatory support (MCS) in several clinical scenarios1.
Correct device positioning is pivotal to ensure proper functioning, avoiding suboptimal unloading and device-related complications2.
Optimal positioning results from a multiparametric assessment, encompassing:
- pressure and motor current waveforms,
- device depth across the aortic valve,
- orientation of the inflow tip within the left ventricle (LV).
However, among these parameters, device orientation might be often overlooked, particularly considering that Impella is frequently positioned without echocardiography, in the absence of a standardized protocol for fluoroscopic implantation. Recent data suggest that Impella malrotation within the LV has relevant clinical implications, leading to increased risk of ischemic stroke, ARC MCS 3b to 5 bleeding events and worsening of aortic and mitral regurgitation during support3.
Increasingly used by physicians to share and discuss clinical cases, tools and techniques with colleagues, social media (SoMe) provide a unique perspective on real-world clinical practice, and are increasingly used as a primary source of education4-6.
We performed a systematic search in Twitter website through the “search Twitter” tool. Using “advanced search” options under “videos” category, the keyword “Impella” was searched (under “any of these words” domain) to identify all the posts in English language with video contents, published on the platform between June 1, 2021 and June 1, 2022. A screening of the videos was performed by an interventional cardiologist (AB), excluding all the posts containing only promotional videos, animations or bench testing, those not showing images of the Impella catheter in place, and those demonstrating only the Impella RP device. We systematically identified 56 videos, published by 50 different users (Supplementary Table 1). All the videos were reviewed by an interventional cardiologist (AB) and by an intensive care cardiologist (LB) to assess device orientation. For the purpose of this analysis, Impella orientation was considered evaluable in 45 cases, based on:
- fluoroscopic landmarks provided by coronary angiography or coronary guidewires in major epicardial vessels, allowing the assessment of device orientation related to LV major axis, and/or
- transthoracic echocardiography (TTE) or transesophageal echocardiography (TOE) images showing the orientation of the device inside the LV cavity. Device malrotation was defined as catheter inflow orientation away from LV apex and towards mitral valve apparatus and LV infero-lateral wall (Figure 1).
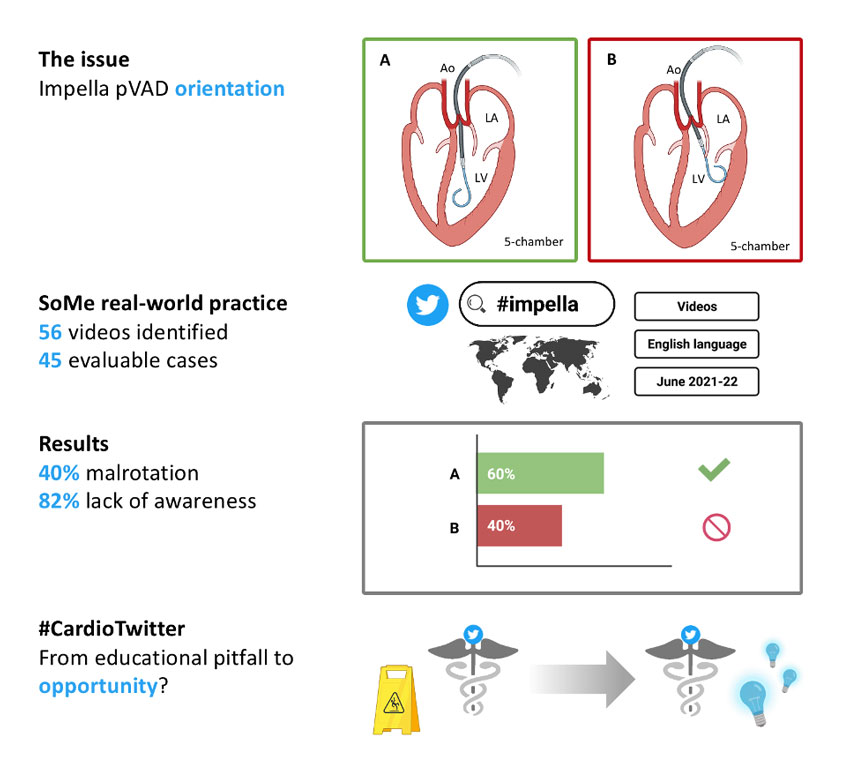
Figure 1. Overview of the study findings with representation of correct (A) and incorrect (B) Impella pVAD orientation in 5-chamber view. Created with BioRender.com
All the comments were reviewed for any reference to device positioning.
The reported indications for Impella use were cardiogenic shock in 44.4 % and protected high-risk percutaneous coronary intervention (PCI) in 53.4 % of cases. The Impella CP was the most frequently used pVAD (76.4 %). The pVAD was inserted via the femoral artery in 95.5 % of cases. Only in 1 case the initial device positioning technique was specifically described, being TTE-guided bedside implant.
Fluoroscopy images were available in 88.9 % of cases, with multiple fluoroscopic views being showed in 77.5 % of those videos, only for the purpose of coronary angiography or PCI. TTE or TOE were available in 6.7 % and 15.5 % of cases, respectively. Multimodality imaging (fluoroscopy plus TTE or TOE) was shown in 11.1 % of cases.
Impella malrotation was observed in 18 (40.0 %) cases. Among them, malrotation was identified and mentioned by either the author or commenting users only in 5/18 (27.8 %) cases, and adverse outcomes related to incorrect device position were reported in 4/18 (22.2 %) patients that included ineffective LV unloading with thrombus formation in a patient receiving VA-ECMO support, suction alarms, interference with mitral valve function, and device-related chordal rupture causing severe mitral regurgitation, respectively. In all the 5 cases in which malrotation was recognized, either TTE or TEE images were provided. The videos had a median number of views of 1093 (IQR 398 – 3121), potentially generating a large number of impressions (Supplementary Table 2).
Our data suggest that, from a SoMe perspective, correct Impella orientation is often overlooked and that Impella malrotation is a common issue in real-world clinical practice, potentially associated with relevant complications. In the reviewed cases, echocardiography appeared pivotal in recognition of malrotation, whereas the lack of a standardized fluoroscopic implantation protocol might hamper its identification. Despite a high number of visualization and potential interactions generated by these videos, the low recognition of the problem might hint at a general unawareness of correct device positioning and represents an important call to action.
Our study is limited by the nature of the information source: first, it lacks the inclusiveness of a systematic review; second, it could not infer if the malrotation was recognized and eventually managed during patient care.
From a SoMe outlook, Impella malrotation is a common and often overlooked issue. The analysis of SoMe data might capture emerging issues with novel devices by exploring real-world clinical practice from a different contemporary perspective.
Supplementary Table 1. Twitter posts included in the study.
Twitter Handle | User ID | Post ID | Post Date | Evaluable |
@MouhamedAmr1 | 1 | 1 | 04/06/21 | 1 |
@assiri99 | 2 | 2 | 07/06/21 | 1 |
@FabriziougoMD | 3 | 3 | 10/06/21 | 1 |
@MarioIannaccon8 | 4 | 4 | 16/06/21 | 1 |
@TheNarulaSeries | 5 | 5 | 07/07/21 | 1 |
@piccoloraf | 6 | 6 | 09/07/21 | 1 |
@alaa_gabi | 7 | 7 | 24/07/21 | 1 |
@karrowni | 8 | 8 | 30/07/21 | 0 |
@MarioIannaccon8 | 4 | 9 | 16/08/21 | 1 |
@MichaelMegalyMD | 9 | 10 | 17/08/21 | 1 |
@KAlaswadMD | 10 | 11 | 20/08/21 | 1 |
@MustafaAhmedMD | 11 | 12 | 22/08/21 | 1 |
@MusaSharkawiMD | 12 | 13 | 23/08/21 | 1 |
@mirvatalasnag | 13 | 14 | 31/08/21 | 1 |
@nyalborgesmd | 14 | 15 | 01/09/21 | 0 |
@markiewicz_md | 15 | 16 | 12/09/21 | 0 |
@atishmathurmd | 16 | 17 | 16/09/21 | 1 |
@cvespiritosanto | 17 | 18 | 25/09/21 | 1 |
@gtheodosmd | 18 | 19 | 06/10/21 | 1 |
@thiele_holger | 19 | 20 | 15/10/21 | 1 |
@aicardio | 20 | 21 | 15/10/21 | 1 |
@NMerke | 21 | 22 | 24/10/21 | 1 |
@AntoniousAttall | 22 | 23 | 28/10/21 | 0 |
@BruckelJeffrey | 23 | 24 | 01/11/21 | 1 |
@sjorge4 | 24 | 25 | 15/11/21 | 1 |
@KPujdak | 25 | 26 | 24/11/21 | 1 |
@beavaquerizo | 26 | 27 | 01/12/21 | 1 |
@aspergian1 | 27 | 28 | 06/12/21 | 0 |
@MagdyHannaMD | 28 | 29 | 08/12/21 | 1 |
@RajTayalMD | 29 | 30 | 11/12/21 | 0 |
@SRCathLab | 30 | 31 | 14/12/21 | 1 |
@mirvatalasnag | 13 | 32 | 22/12/21 | 0 |
@KU_CCM | 31 | 33 | 14/01/22 | 1 |
@AdrianMercadoMD | 32 | 34 | 05/02/22 | 1 |
@moiz_hafiz | 33 | 35 | 10/02/22 | 0 |
@de_clinico | 34 | 36 | 10/02/22 | 1 |
@Saar_Minha | 35 | 37 | 11/02/22 | 1 |
@KPujdak | 25 | 38 | 22/02/22 | 1 |
@klsharnagat | 36 | 39 | 25/02/22 | 0 |
@TTelila | 37 | 40 | 02/03/22 | 1 |
@KeithNguyenSAIF | 38 | 41 | 12/03/22 | 1 |
@BaoGTran | 39 | 42 | 13/03/22 | 1 |
@NeerajShahMD | 40 | 43 | 20/03/22 | 1 |
@DrJayMohan | 41 | 44 | 26/03/22 | 1 |
@Kabirjt | 42 | 45 | 27/03/22 | 0 |
@ESC_Journals | 43 | 46 | 29/03/22 | 0 |
@MCiardetti | 44 | 47 | 07/04/22 | 1 |
@luisnietor93 | 45 | 48 | 08/04/22 | 1 |
@SarasVallabhMD | 46 | 49 | 12/04/22 | 1 |
@jefftylermd | 47 | 50 | 20/04/22 | 1 |
@TSchneider0 | 48 | 51 | 25/04/22 | 1 |
@DrNaddi | 49 | 52 | 26/04/22 | 1 |
@BaoGTran | 39 | 53 | 01/05/22 | 1 |
@TTelila | 37 | 54 | 05/05/22 | 1 |
@BruckelJeffrey | 23 | 55 | 06/05/22 | 1 |
@TernacleJ | 50 | 56 | 19/05/22 | 1 |
Supplementary Table 2. Main study findings.
PCI: percutaneous coronary intervention; pVAD: percutaneous ventricular assist device; TOE: transoesophageal echocardiography; TTE: transthoracic echocardiography.
| Cases with available data | Value |
Indication for pVAD Cardiogenic shock, n (%) |
45 |
20 (44.4) |
Impella type CP, n (%) |
17 |
13 (76.4) |
Impella insertion route Femoral, n (%) |
45 |
43 (95.5) |
Imaging modality Fluoroscopy, n (%) |
45 |
40 (88.9) |
Malrotation, n (%) | 45 | 18 (40.0) |
Malrotation recognized, n (%) | 18 | 5 (27.8) |
Adverse outcome reported, n (%) | 18 | 4 (22.2) |
Tweet performance Views, median (IQR) |
45 |
1093 (398 – 3121) |
References
- Chieffo A, Dudek D, Hassager C, Combes A, Gramegna M, Halvorsen S, Huber K, Kunadian V, Maly J, Møller JE, Pappalardo F, Tarantini G, Tavazzi G, Thiele H, Vandenbriele C, Van Mieghem N, Vranckx P, Werner N, Price S. Joint EAPCI/ACVC expert consensus document on percutaneous ventricular assist devices. EuroIntervention. 2021;17:E274–86.
- Roberts N, Chandrasekaran U, Das S, Qi Z, Corbett S. Hemolysis associated with Impella heart pump positioning: In vitro hemolysis testing and computational fluid dynamics modeling. Int J Artif Organs. 2020;43:710–8.
- Baldetti L, Beneduce A, Romagnolo D, Frias A, Gramegna M, Sacchi S, Calvo F, Pazzanese V, Cappelletti AM, Ajello S, Scandroglio AM, Chieffo A. Impella Malrotation Within the Left Ventricle Is Associated With Adverse In-Hospital Outcomes in Cardiogenic Shock. JACC Cardiovasc Interv. 2023;16:739–41.
- Ladeiras-Lopes R, Baciu L, Grapsa J, Sohaib A, Vidal-Perez R, Bohm A, Silvola H, Gimenez MR, Muscoli S, Wallner M, Rakisheva A, Nagy VK, Cowie MR, Clarke SC, Achenbach S, the ‘Cardiologists of Tomorrow’ DH and MC of the ES of C. Social media in cardiovascular medicine: a contemporary review. Eur Hear J - Digit Heal. 2020;1:10–9.
- Brugaletta S. Moving fast towards the future: the role of #SoMe in learning cardiology. EuroIntervention. 2018;13:1874–5.
- Capodanno D. Twitterature. EuroIntervention. 2018;14:e959–61.
Authors








No comments yet!