MitrAI score: machine learning models to predict mortality at 12, 24, 36 and 48 months in patients with primary and secondary MR treated by TEER
Reported from ESC Congress 2024
Jonathan Curio provides his take on the MitrAI score study which was presented by Luigi Biasco at ESC Congress 2024 in London.
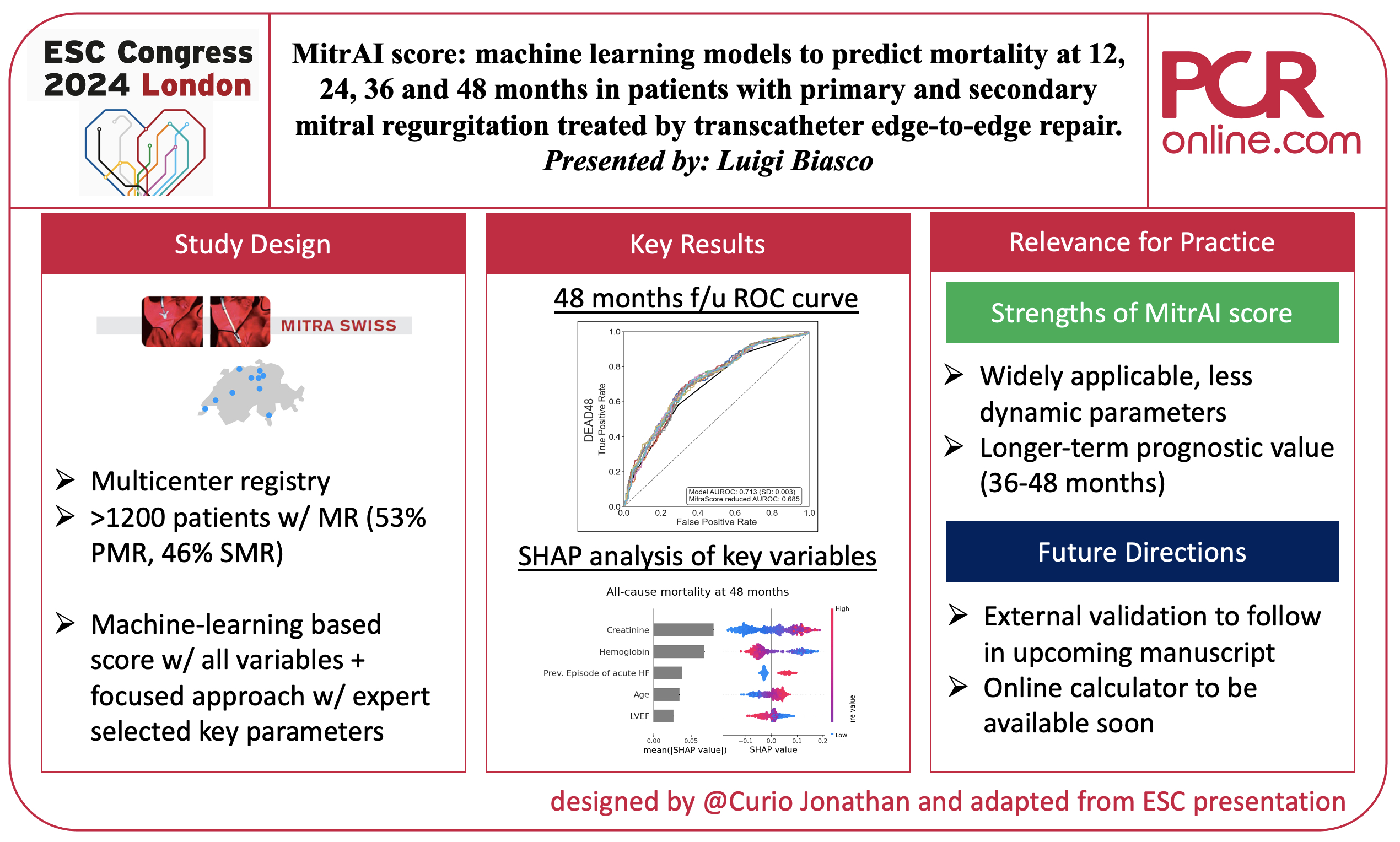
Graphic summary of key aspects of the MitraAI score study. Courtesy of Jonathan Curio. Source: PCRonline.com
Why this study? – The rationale/objective
Transcatheter mitral valve edge-to-edge repair (M-TEER) has been established as a safe and effective treatment modality in patients suffering from primary or secondary mitral regurgitation (MR) and at an increased risk of surgical mortality (1).
Several prediction tools have been developed, based on landmark trials such as COAPT or based on large real-world registries such as EuroSMR, to predict outcomes and stratify patients according to their likely clinical benefit following M-TEER (2,3). However, these tools included mostly patients with secondary MR and did predict outcomes only up to a maximum of 2 years.
Thus, the aim of the present study, using a machine learning approach, was to derive and validate a compact score predicting all-cause mortality after M-TEER in patients with either primary or secondary MR, also beyond the timeframe of only 12 months.
How was it executed? – The methodology
The study was based on the prospective multicenter MitraSwiss registry. Key features of this registry are as follows:
- Investigator-initiated registry at 10 Swiss centers enrolling consecutive patients with moderate or severe primary or secondary MR
- Patients were treated using the MitraClip (Abbott) M-TEER device
- Between 2011 and 2019, 1268 patients were enrolled, mean age was 76 years, median STS score 3.7%, and median EuroScore II 4.1%; 40% of the patients were female.
A machine learning (ML) model was used to predict all-cause mortality at 12, 24, 36, and 48 months after M-TEER. Compact models were created based on expert-chosen widely available clinical variables, repeated cross-validation was performed, and two classification algorithms, Random Forest and Logistic Regression, were used. SHapley Additive ExPlanations (SHAP), a game-theory-based method allowing to rank different features by importance and how they drive a model’s prediction was used to interpret the models. Receiver operating characteristic (ROC) curves were used for internal validation of the models. The previous logistic regression based MitraScore was used as a comparative benchmark.
What is the main result?
Out of the 1268 patients in the MitraSwiss registry, 1142 had available data to be included in the study.
- Etiology of MR was well balanced between primary (52.8%) and secondary MR (45.4%); mixed etiology in 1.8%
- Median follow-up time was 36.6 months, follow-up was complete in 97.2%
- All-cause mortality at 12, 24, 36, and 48 months was 12.3%, 20.0%, 28.1%, 35.4%, respectively
First, four ML models to predict all-cause mortality at the different follow-up time points were derived from the entire set of 50 different variables available in the MitraSwiss registry. Internal validation showed good discriminative capacity with an area under the ROC curve of 0.74, 0.72, 0.75 and 0.71 at 12, 24, 36, and 48 months in the overall population, showing better discriminative performance than the MitraScore benchmark. Baseline hemoglobin, glomerular filtration rate, and creatinine showed the highest relevance according to the SHAP analysis, with age becoming continuously more relevant with the duration of follow-up. The distinction between primary or secondary MR was not correlated with prognostic relevance.
Second, to create widely adoptable ML models with high ease-of-use nine key expert selected features were included in a further analysis. These included:
- Laboratory parameters: hemoglobin, creatinine
- Comorbidities: diabetes, atrial fibrillation
- Clinical characteristics: age, BMI, NYHA class, number of HF hospitalisations prior to M-TEER
- Echocardiographic parameters: LVEF
These models showed good discriminative power (AUROC 0.73 at 12 months, 0.73 at 24 months, 0.75 at 36 months and 0.71 at 48 months), especially, these models performed equally to those derived from the whole set of available variables.
Critical reading and the relevance for clinical practice
The MitrAI score provides a compact easy-to-use ML-based tool to predict all-cause mortality after M-TEER in patients with either primary or secondary MR with a good discriminative power, especially at longer follow-up of 36-48 months.
Prediction of outcomes after M-TEER and identification of those patients who will most likely experience the largest benefit after intervention remains one of the key questions in the field of transcatheter therapies for MR. In this regard, a particular strength of this work is the implementation of widely available, and, especially less dynamic parameters. Other scores used parameters such as NT-proBNP levels, often highly variable over a short period of time or distinct echocardiographic parameters that show a high examiner dependency.
What is particularly interesting about this score, and this work in general, is the observation that beyond the time frame of two years, which has been covered in previous scores, once MR is reduced after M-TEER the etiology loses predictive power with longer duration of follow-up and other baseline parameters such as LVEF and also patient age become more relevant. This allows the score to be applied to both MR etiologies and may imply the ability of M-TEER to restore a patient’s prognosis to a level where outcomes are based on other general background parameters. To identify these patients who have their events at a later follow-up timepoint, then related to more general baseline parameters, and to better understand their characteristics might be a further interesting scope of research.
The data presented at the current meeting shows internal validation of this score only. However, the investigators have also performed an external validation which is said to be presented in an upcoming publication.
A further limitation to be noted may be the use of MitraClip as the only M-TEER device. Especially, when treating both etiologies, secondary as well as primary MR, there may be cases where based on the patients' anatomy other M-TEER devices with different technological features can bear the potential to further improve procedural outcomes, which could affect the reported outcomes.
Still, a high rate of MR grade ≤ 2 at the end of the procedure reflects the high experience of the involved centers, and this low number of cases with higher degrees of residual MR likely explains why there was no evident significant influence of post-procedural MR on later outcomes.
In conclusion, the MitraAI score promises to represent a handy tool to predict mortality after M-TEER, also for a longer follow-up of up to four years, in patients with both primary and secondary MR. An online calculator to make this prediction tool available to the community will be released soon.
References
- Vahanian A, Beyersdorf F, Praz F, Milojevic M, Baldus S, Bauersachs J et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J 2022;43:561-632.
- Shah N, Madhavan MV, Gray WA, Brener SJ, Ahmad Y, Lindenfeld J et al. Prediction of Death or HF Hospitalization in Patients With Severe FMR: The COAPT Risk Score. JACC Cardiovasc Interv 2022;15:1893-1905.
- Hausleiter J, Lachmann M, Stolz L, Bedogni F, Rubbio AP, Estévez-Loureiro R et al. Artificial intelligence-derived risk score for mortality in secondary mitral regurgitation treated by transcatheter edge-to-edge repair: the EuroSMR risk score. Eur Heart J 2024;45:922-936.




No comments yet!