31 Oct 2025
Stratified treatment of myocardial infarction with non-obstructive coronary arteries: the PROMISE trial
Reported from TCT 2025
Nicola Ryan provides her take on the PROMISE trial presented by Rocco Antonio Montone at TCT 2025, in San Francisco.
Designed by Nicola Ryan. Source: PCRonline.com
Why this study – the rationale/objective?
MINOCA is an umbrella term for patients who present with a clinical diagnosis of myocardial infarction with non-obstructive coronary arteries on coronary angiography. The underlying mechanisms for MINOCA are heterogenous and include unstable plaques (plaque rupture or erosion), coronary embolism, spontaneous coronary artery dissection and coronary vasospasm (epicardial or microvascular). Approximately 6-8 % of patients with MI have MINOCA however the most effective diagnostic and management strategy remains a dilemma.
The PROMISE trial aimed to evaluation the benefit of a stratified therapeutic strategy guided by the knowledge of MINOCA aetiology versus standard care on clinical outcomes. Read more about the study design and rationale (published in EuroIntervention) of the PROMISE Trial here.
How was it executed - the methodology?
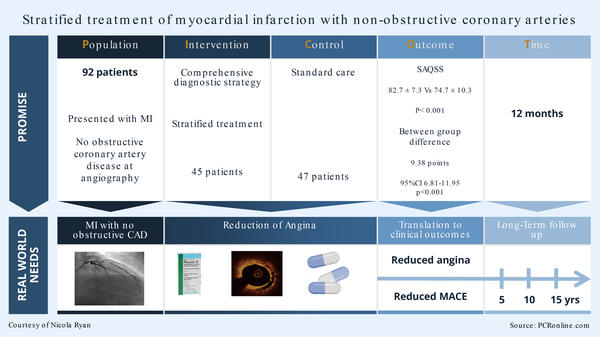
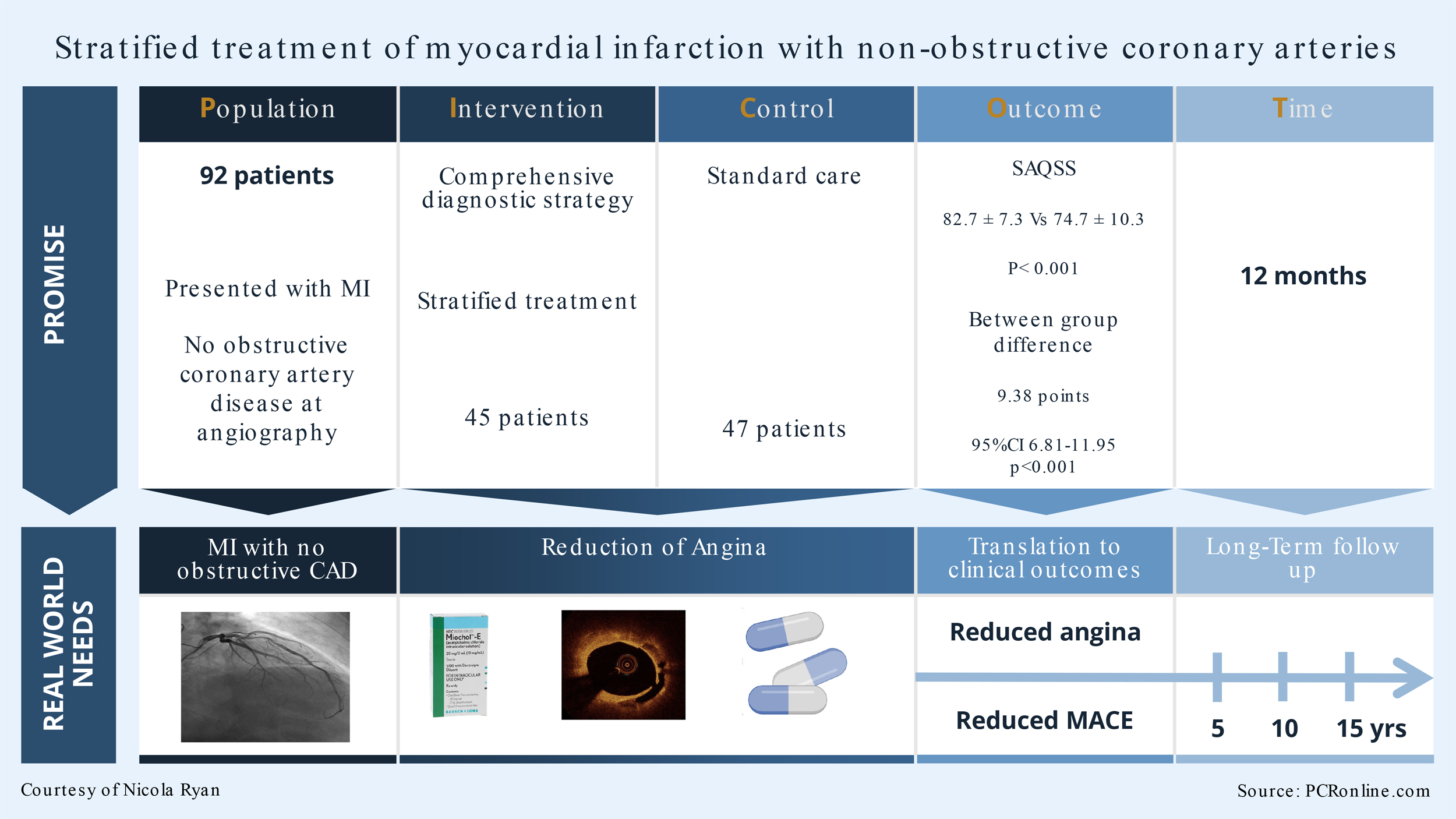
Patients with MINOCA were randomised to “stratified treatment” or standard of care. In the stratified treatment group, a comprehensive diagnostic workup aimed at identifying MINOCA aetiology including OCT, Acetylcholine provocation testing, transoesophageal and or contrast echocardiography and CMRI was carried out. If an underlying aetiology was not found after diagnostic work up, patients were classified as “undefined” MINOCA. Patients were managed based on the underlying aetiology of MINOCA. In the standard of care, patients received routine diagnostic workup without additional diagnostic tests (intracoronary imaging or functional testing). CMRI was carried out in the standard of care groups at the discretion of the treating clinician.
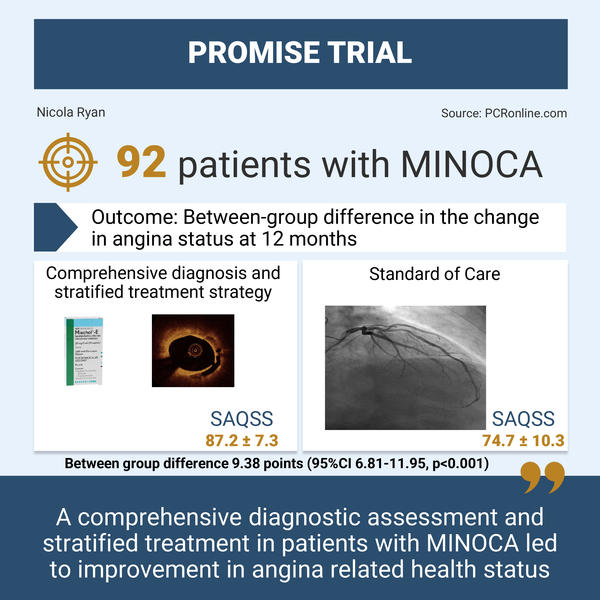
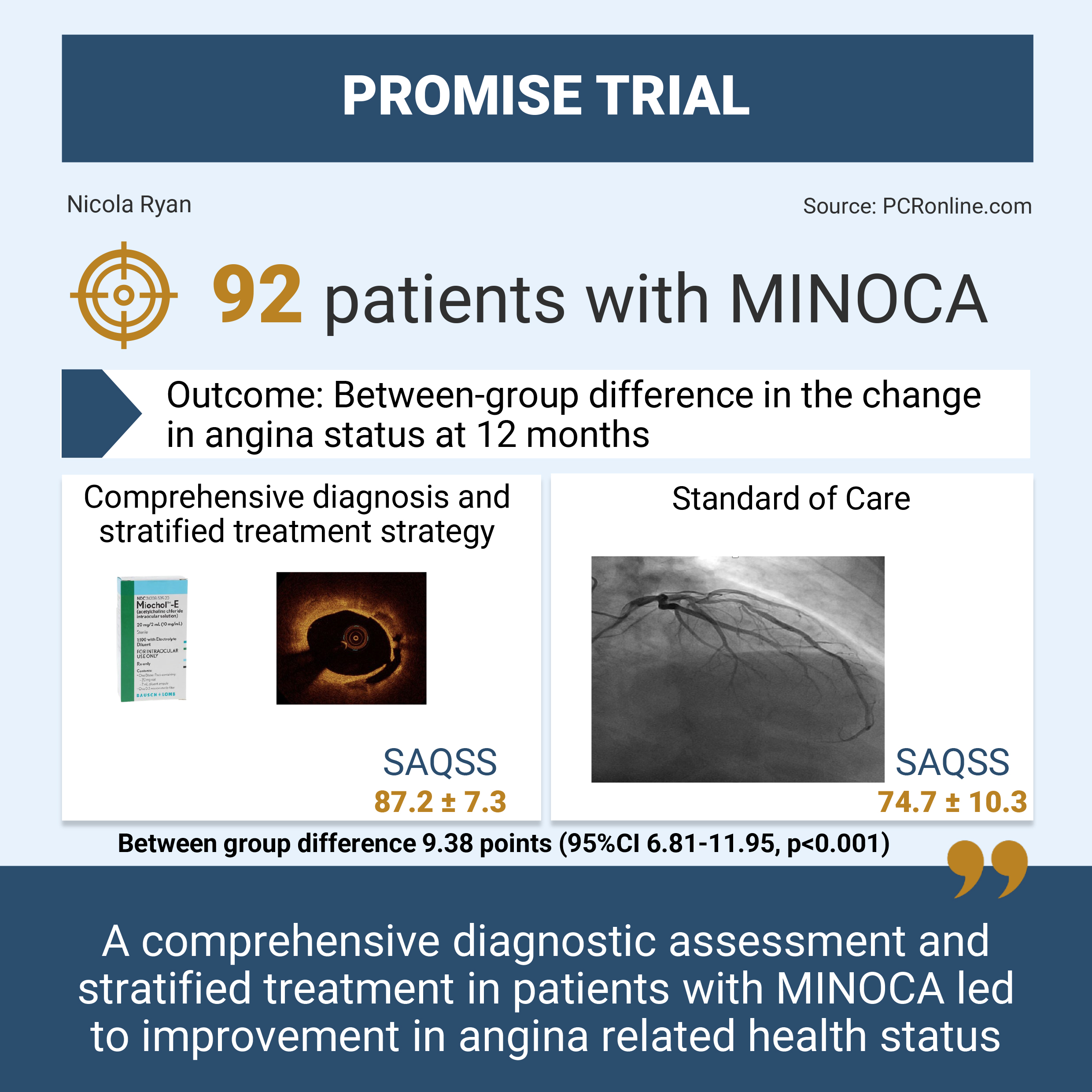
- The primary endpoint was the between-group difference in the change in angina status at 12 months assessed by the Seattle angina Questionnaire summary score (SAQSS)
- The secondary endpoint was MACE, a composite of all-cause mortality, non-fatal MI, stroke, rehospitalisation for heart failure, and repeated coronary angiography.
What is the main result?
Designed by Nicola Ryan. Source: PCRonline.com
From July 2021 to June 2024, 101 patients with an initial diagnosis of MINOCA were enrolled with 9 patients excluded due to an alternative diagnosis identified (takotsubo syndrome, n. = 4 and myocarditis, n = 5). Finally, 45 patients were randomised to stratified treatment and 47 to standard of care. There was a near 50:50 split of male and female patients with a high prevalence of common CVRF. Approximately a fifth of patients presented with STEMI with the majority having a preserved LVEF.
- The primary endpoint SAQSS was higher in the stratified treatment group than standard of care group (82.7 ± 7.3 vs. 74.7 ± 10.3, p < 0.001)
- Between group difference 9.38 points (95 %CI 6.81-11.95, p < 0.001)
- There was no difference in MACE between groups at 12 months (2.2 % stratified treatment vs. 8.5 % standard of care group, p = 0.186)
Critical reading and the relevance for clinical practice
The results of the PROMISE trial shows that a comprehensive diagnostic assessment and stratified treatment in patients with MINOCA led to improvement in angina related health status. Despite the advances in diagnostic technology, MINOCA remains a diagnostic dilemma in everyday clinical practice. Importantly, a diagnosis of MINOCA is associated with a high prevalence of persistent angina on discharge, thus appropriately identifying and treating the underlying aetiology has significant potential benefits for patients quality of life and ongoing health care utilisation.
In the stratified treatment group, the underlying aetiology of the MINOCA was identified in 80 % of patients, allowing therapy based on the specific aetiology. The treating clinicians were asked to specify their suspected underlying aetiology prior to comprehensive diagnostic assessment, following work up the final aetiology of MINOCA was reclassified in 75.5 % of patients. In this group, epicardial spasm (35.6 %) followed by unstable plaque (22.2 %) were the most common aetiology of MINOCA followed by SCAD (13.3 %), demonstrating the benefit of intracoronary imaging and functional testing in patients with unobstructed arteries who present with MI. Importantly, there were no complications associated with the use of functional testing or intracoronary imaging which can be a concern leading to underuse of these tests.
Despite advanced diagnostics, 20 % of the stratified treatment group remained undifferentiated beyond the original MINOCA label. This highlights the ongoing need for investigations into the potential aetiologies of MINOCA. There are ongoing limitations with regard to interpretation of functional testing and, in some cases, patients clinical conditions may preclude advanced testing with acetyl choline provocation or CMRI.
There is a number of important limitations to consider in the PROMISE trial, including the early termination on the recommendation of the DSMB due to numerically more MACE in the standard of care group. The overall number of patients enrolled was lower than initially predicted. Finally, the open label nature of the trial has potential patient and clinician bias with regard to treatment as well as investigation of further presentations with chest pain/angina.
Overall, the authors should be congratulated for the first randomised evidence supporting a comprehensive diagnostic evaluation and stratified treatment in this population. Further larger scale trials are required to validate this study in the general population, and ongoing training and education in intracoronary imaging and functional testing is required for the community at large.




1 comment
These are often clinically frustrating and challenging cases, however it seems simply and totally intuitive to me, to employ cath with or without pharmacologic testing and intracoronary physiologic measurements if needed, as well as advanced imaging to define the etiology of each patients problem when possible.