3-year outcomes of the ULTIMATE trial comparing intravascular ultrasound versus angiography-guided drug-eluting stent implantation
Selected in JACC Cardiovascular Interventions by N. Ryan
ULTIMATE provides additional long-term randomised control data showing the benefit of IVUS guided PCI in an all-comers population.
References
Authors
Xiao-Fei Gao, Zhen Ge, Xiang-Quan Kong, Jing Kan, Leng Han, Shu Lu, Nai-Liang Tian, Song Lin, Qing-Hua Lu, Xiao-Yan Wang, Qi-Hua Li, Zhi-Zhong Liu, Yan Chen, Xue-Song Qian, Juan Wang, Da-Yang Chai, Chong-Hao Chen, Tao Pan, Fei Ye, Jun-Jie Zhang, Shao-Liang Chen, and for the ULTIMATE Investigators
Reference
J Am Coll Cardiol Cardiovasc Interv. 2021 Feb, 14 (3) 247–257
Published
February 2021
Link
Read the abstractReviewer
Latest contributions
Balloon lithotripsy added to conventional preparation before stent implantation in severely calcified coronary lesions Impact of pullback pressure gradient on clinical outcomes after percutaneous coronary interventions Validation of intravascular ultrasound-defined optimal stent expansion criteria for favorable 1-year clinical outcomesMy Comment
Why this study? – the rationale/objective
ULTIMATE was a randomised control trial comparing intravascular ultrasound (IVUS) versus angiography guided drug-eluting stent (DES) implantation in 1,448 all-comers.
The benefits of IVUS have been demonstrated at short term follow up (≤1 year) however there are limited data supporting persistence of this benefit in the longer term.
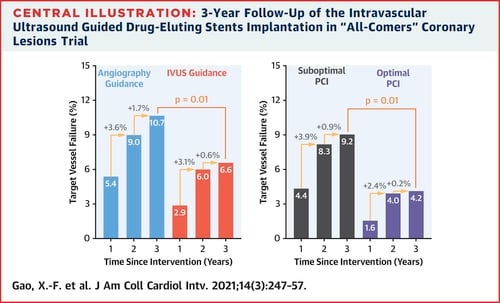
The ULTIMATE trial demonstrated that at one-year TVF (cardiac death, target vessel MI and clinically driven TVR) was significantly lower in the IVUS guided group compared to the angiography guided group (2.9% vs. 5.4% HR 0.530, 95%CI 0.312-0.901, p=0.019).
In this paper, the authors report the 3-year outcomes.
How was it executed? – the methodology
ULTIMATE was a randomised control trial in patients with silent ischaemia, stable or unstable angina or MI with de-novo coronary lesions undergoing PCI with DES implantation.
Patients were randomised, in a 1:1 fashion to IVUS or Angiography guidance.
- The primary endpoint was TVF (cardiac death, target vessel MI and clinically driven TVR) at 3 years
- Safety endpoint was definite or probable stent thrombosis
- Landmark analysis of events from 12 months to 3 years was carried out.
- Optimal PCI in the IVUS group required all three IVUS criteria (MLA >5mm or 90% of the MLA at the distal reference segments, plaque burden 5mm proximal or distal to the stent edge <50% and no edge dissection involving the media with length >3mm).
What is the main result?
ULTIMATE randomised 1,448 patients; 724 to the IVUS guidance and 724 to angiography guidance. 3-year outcomes were available for 98.6% and 97.9% of patients respectively.
Almost three-quarters of patients were male, the majority (78%) presenting with ACS. From an angiographic point of view >50% had a LMS or LAD lesion, with MVD common (>50%) and bifurcation lesions present in a quarter.
Mean stent diameter was larger in the IVUS arm (3.15±0.42 vs. 2.99±0.38, p<0.001)
- At three year follow up TVF was more common in the angiography guided group (10.7% vs. 6.6%, HR 0.60, 95%CI 0.42-0.87, p=0.01), mainly due to clinically driven TVR (6.9% vs 4.5%, HR 0.64 95%CI 0.41-1.0, p=0.05)
- There was no significant difference in the safety endpoint at three years however no definite or probably stent thrombosis occurred in the IVUS guided arm after 1 year with 3 further events in the angiography guided arm.
- Landmark analysis showed that 63 TVF’s occurred between 1 and 3 years with no differences between groups (IVUS 3.7% vs. Angiography 5.5%, HR 0.68, 95%CI 0.41-1.12, p=0.13)
- Of the IVUS group 53% met criteria for optimal PCI, patients with optimal IVUS guided PCI had a lower risk of TVF compared to those with suboptimal IVUS PCI (4.2% vs. 9.2%, HR 0.44, 95%CI 0.24-0.81, p=0.01).

Source: JACC: Cardiovascular Interventions
Critical reading and the relevance for clinical practice:
The results of this study show that the initial benefit in reducing TVF using IVUS guided PCI strategy compared to angiography guided persist at three year follow up in this all-comer study.
In the IVUS group there is an additional benefit in those in whom optimal PCI is carried out versus suboptimal by IVUS criteria.
This data complements the two-year outcomes from the ADAPT-DES study as well as the 5-year outcomes from IVUS-XPL showing the benefit of IVUS guided strategy.
A note of caution when interpreting the results, this was a trial carried out in a single country.
IVUS interpretation requires appropriate training and even in the context of this RCT IVUS defined optimal PCI was only achieved in 53% of patients.
In summary, ULTIMATE provides additional long-term randomised control data showing the benefit of IVUS guided PCI in an all-comers population.
The current guidelines recommend IVUS use in selected patients however this adds to the evidence for its more liberal use.
Given the improved outcomes with optimal versus suboptimal IVUS guided PCI it is important that IVUS images are carefully reviewed and stents optimised to gain most benefit from IVUS use.




No comments yet!