Cardiac mortality in patients randomised to elective coronary revascularisation plus medical therapy or medical therapy alone: a systematic review and meta-analysis
Selected in European Heart Journal by E. Asher
The value of elective coronary revascularisation plus medical therapy over medical therapy alone in managing stable patients with coronary artery disease is debated. Hence, the authors reviewed all trials comparing the two strategies in this population to appraise whether revascularisation in addition to medical therapy affects cardiac mortality at longest follow-up. The results of this Late-Breaking Trial were released during EuroPCR 2021.
References
Authors
Eliano P Navarese, Alexandra J Lansky, Dean J Kereiakes, Jacek Kubica, Paul A Gurbel, Diana A Gorog, Marco Valgimigli, Nick Curzen, David E Kandzari, Marc P Bonaca, Marc Brouwer, Julia Umińska, Milosz J Jaguszewski, Paolo Raggi, Ron Waksman, Martin B Leon, William Wijns, Felicita Andreotti
Reference
10.1093/eurheartj/ehab246
Published
May 2021
Link
Read the abstractReviewer
My Comment
Why this study? – the rationale/objective
Coronary artery disease is the most prevalent medical condition worldwide in terms of disease burden, disability, or early death. Chronic coronary syndromes encompass clinically stable coronary artery disease patients, with or without coronary revascularization
In clinically stable patients with preserved or moderately impaired left ventricular systolic function, symptomatic benefit favouring revascularisation is well known, nevertheless, the value of elective coronary revascularisation plus medical therapy over medical therapy alone in managing stable patients with coronary artery disease is debated.
Hence, the authors reviewed all trials comparing the two strategies in this population to appraise whether revascularisation in addition to medical therapy affects cardiac mortality at longest follow-up.
How was it executed? – the methodology
Eligibility: studies had to enroll clinically stable coronary artery disease patients undergoing, randomization to elective revascularisation plus medical therapy or medical therapy alone.
No limits were set for age, comorbidities, study language, publication status, or publication date.
MEDLINE, EMBASE, Google Scholar, and other databases were searched for randomized trials comparing revascularisation against medical therapy alone in clinically stable coronary artery disease patients. Treatment effects were measured by rate ratios (RRs) with 95 % CI, using random-effects models.
Endpoints:
- Pre-specified primary endpoint - Cardiac mortality.
- Secondary endpoints - Spontaneous myocardial infarction (MI) and its association with cardiac mortality.
- Further endpoints – All-cause mortality, any MI, and stroke.
Events at longest reported follow-up were abstracted.
A pre-specified sensitivity meta-analysis was conducted for the primary endpoint, excluding trials that enrolled only post-ACS patients or only chronic total occlusions (CTOs) or trials with a percent use of CABG in the invasive arm > 30 %.
What is the main result?
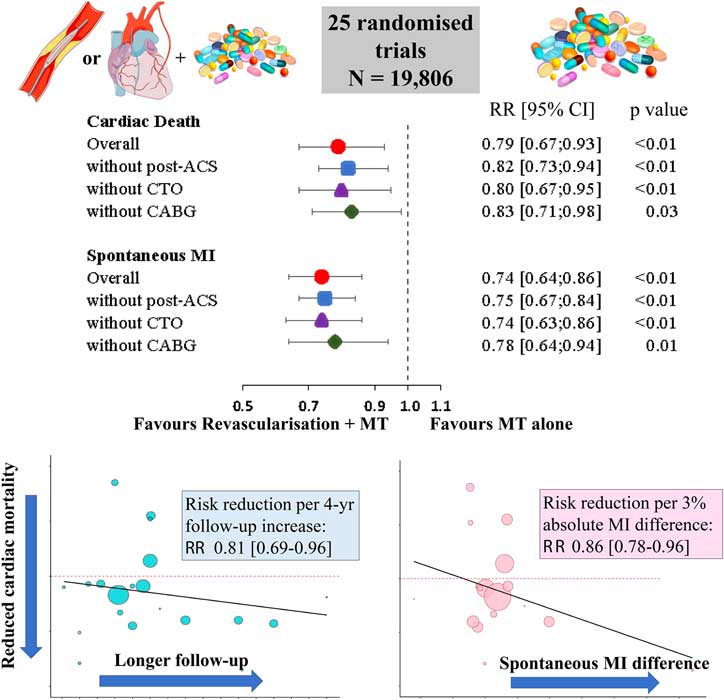
- A total of 25 trials were included in the meta-analysis involving 19,806 patients:
- 10,023 patients randomized to revascularisation plus medical therapy,
- and 9,783 patients to medical therapy alone.
- Compared with medical therapy alone, revascularisation yielded a lower risk of cardiac death [RR 0.79 (0.67–0.93), P < 0.01] and spontaneous MI [RR 0.74 (0.64–0.86), P < 0.01].
- By meta-regression, the cardiac death risk reduction after revascularisation, compared with medical therapy alone, was linearly associated with follow-up duration [RR per 4-year follow-up: 0.81 (0.69–0.96), P = 0.008], spontaneous MI absolute difference (P = 0.01) and percentage of multivessel disease at baseline (P = 0.004). Trial sequential and sensitivity analyses confirmed the reliability of the cardiac mortality findings.
- All-cause mortality [0.94 (0.87–1.01), P = 0.11], any MI (P = 0.14), and stroke risk (P = 0.30) did not differ significantly between strategies.
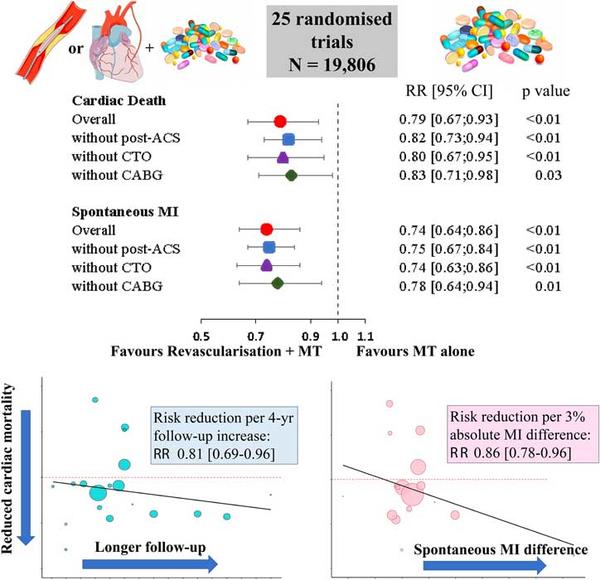
Major findings on cardiac mortality reduction with elective coronary revascularisation plus medical therapy vs. medical therapy alone.
Source: European Heart Journal
Critical reading and the relevance for clinical practice:
The main findings of the meta-analysis are:
- A significantly lower risk of cardiac death was observed among patients randomized to revascularisation plus medical therapy compared with medical therapy alone.
- The cardiac survival benefit of revascularisation plus medical therapy increased progressively over time, with an incremental RRR of 19 % for every 4 years of follow-up extension.
- There was an association between the reduced risk of cardiac death and the difference between treatment arms in spontaneous MI.
An interesting finding was that the magnitude of cardiac mortality reduction appeared to be a function of both revascularisation and follow-up duration.
Possible explanations for that are:
- durable benefits of revascularisation in contrast to attenuation of medical adherence over time;
- fewer spontaneous MIs,
- and temporal dilution of early procedural complications following revascularisation.
Moreover, the authors observed an association between reduction of spontaneous MI and reduced risk of cardiac death, that might explain the cardiac death reduction observed with revascularisation plus medical therapy compared with medical therapy alone.
The findings of this meta-analysis may be insightful when interpreting the results of the ISCHEMIA trial. Although in the ISCHEMIA trial revascularisation did not significantly improve the primary composite endpoint nor reduce cardiovascular mortality at a median follow-up of 3.2 years, the primary endpoint time-to-event curves for the two treatment arms crossed at ~ 2 years and then continued to diverge in favour of revascularisation plus medical therapy. Moreover, the authors claim that by pooling data at longest follow-up, expanding sample size, focusing on follow-up duration, extracting homogeneous modes of death from included trials, and exploring plausible causal relations, the present meta-analysis shows a robust and consistent reduction of cardiac mortality in favor of elective coronary revascularisation plus medical therapy, directly associated with duration of follow-up and with lower risk of spontaneous MI.
Should common practice and guidelines be changed?
The study had several limitations:
- trial-level data were included. However, consistency between the overall and the sensitivity analyses supports the robustness of the findings. Deleting each trial in turn did not produce significant deviations from the original overall estimate.
- Plausibility is supported by the meta-regressions associating cardiac mortality benefits with length of follow-up and with absolute risk difference for spontaneous MI.
- Crossover from medical therapy alone to revascularisations plus medical therapy may have diluted the effect of revascularization.
- Heterogeneity across studies in the % use and type of coronary stents,
- Lack of individual patient data prevents a precise characterisation of stent effects on outcomes.
This might highlight the importance of establishing clearer recommendations and standardized practices in this setting.
Further reflection
What is your approach regarding elective coronary revascularization in managing stable patients with coronary artery disease?
Do you think patients with stable coronary disease can benefit from elective revascularization?
Related content
View the slides of the Late-Breaking Trial presentation presented at EuroPCR 2021 here.





No comments yet!