Death and myocardial infarction following initial revascularization vs optimal medical therapy in chronic coronary syndromes with myocardial ischemia
Selected in JAHA
A systematic review and meta-analysis of contemporary randomized controlled trials published in the JAHA, interpreted using a standardized two-step approach: PICOT and SWOT
References
Authors
Andrea Soares, William E Boden, Whady Hueb, Maria M Brooks, Helen EA Vlachos, Kevin O’Fee, Angela Hardi, and David L Brown
Reference
Journal of the American Heart Association. 2021;10
Published
January 2021
Link
Read the abstractMy Comment
What is presented?
- A summary of the key evidence from a recent meta-analysis on revascularization vs. medical therapy in patients with chronic coronary syndrome by the PICOT method.
- Interpretation of this evidence in the light of its methodological constraints and practical generalizability by the SWOT method.
What is intended?
To provide guidance for the critical reflection on the effects of revascularization in chronic coronary syndromes by using a standardized two-step approach:
- capturing the facts of the study (PICOT) and
- assessing its strengths and weaknesses in terms of methodology and practical applicability (SWOT).
PICOT
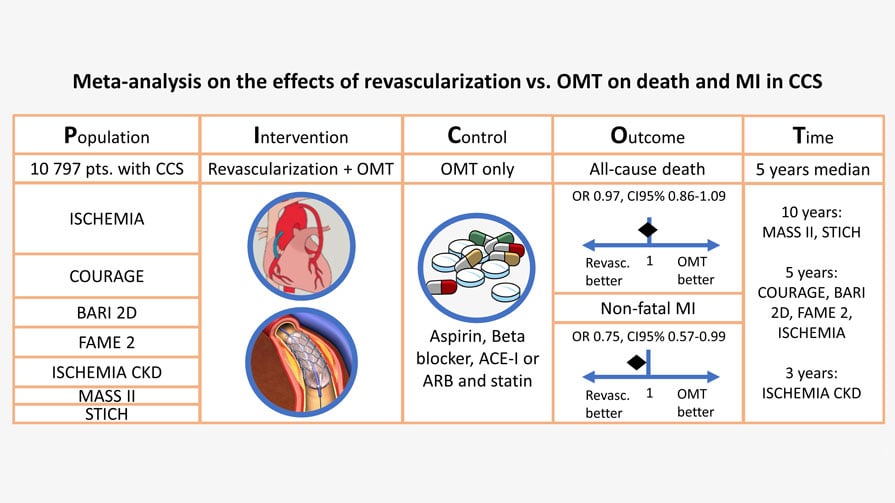
Key evidence on the effects of revascularization in stable coronary patients
Population:
- The analysis included 10,797 patients, from 7 trials, with CCS and no significant left main stenosis, randomized to either percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) plus optimal medical therapy (OMT) vs. OMT alone.
- To better reflect contemporary practice, only trials with at least 50% stent implantation, as opposed to POBA alone, in patients undergoing PCI and at least 50% statin use were considered.
- Importantly, all included patients had evidence of ischemia (non-invasive tests or FFR) prior to randomization.
- Included trials had heterogenous exclusion criteria (predominantly severe/refractory angina and severely reduced ejection fraction), however, LMS stenosis >50% was common to all as an exclusion criterion.
Intervention:
- The coronary revascularization + OMT and OMT alone group included patients undergoing PCI or CABG.
Control:
- The control group included patients treated with OMT (aspirin, beta-blockers, angiotensin-converting enzyme inhibitors and statins) alone.
- None of the trials in the analysis were (or indeed could be) blinded.
Outcomes:
- Death from any cause and nonfatal MI (analysed on an ITT basis).
- Mortality was similar in the revascularization (11.8%) vs. OMT alone group (12.0%).
- Nonfatal MI was less frequent in patients who underwent revascularization as compared with OMT (10.2% vs. 11.6%, p=0.04), albeit with significant heterogeneity between the trials.
- Subgroup analysis suggested that the beneficial effect of revascularization on the reduction of nonfatal MI was seen predominantly with surgical revascularization, as opposed to PCI (p for interaction 0.01). However, this result seems to mainly be driven by BARI 2D and STICH trials, which specifically enrolled patients with diabetes and reduced LVEF.
Time:
Median follow-up was 5 years across the trials.
SWOT
Strengths:
Highest-quality of evidence
- Included studies were prospective, randomized control trials.
‘Hard’ clinical endpoints
- All‐cause death and nonfatal MI reported.
Large (and diverse) patient population
- 10,797 patients from North & South America, Europe and Asia were included allowing for global representation.
- Inclusion of a wide range of ejection fractions (26-67%), diabetes (26-100%) and prior revascularization (16-75%) as well as those with chronic kidney disease.
Generally robust meta-analytical methods were employed
- Sensitivity analysis was performed
- Patient-level data sought where possible
Weaknesses:
Heterogeneity
- The inclusion criteria were heterogeneous between studies.
- The definition of nonfatal MI varied and became more precise in the more recent studies, with the diagnosis generally requiring appropriate symptoms, biomarker elevation, and/or electrocardiographic changes.
Not fully representative of contemporary practice
- Some studies such as MASS II and COURAGE are decades old and may not be representative of contemporary practices (including stent platforms, use of intracoronary imaging and OMT including PCSK9i).
- Not all enrolled patients underwent stress testing and in some, it was limited to treadmill stress testing without objective quantification of ischemia.
- The trials included enrolled patients from 1997 to 2018 - inevitably leading to between-study heterogeneity in terms of the procedural techniques, most notably regarding the implantation of drug-eluting stents, with per-trial rates between 0% and 100%.
- Lack of blinding. Although the trials are randomized cohorts, they are not blinded thereby impacting the cross over rates.
- Cross over from OMT to revascularization varied from 19% to 51% across the trials.
- Measures of quality of life cannot be obtained from this analysis which is the primary driver for revascularization in those with CCS (i.e. angina relief).
Statistical limitations
- As the number of studies was <10 for both mortality and nonfatal MI endpoints, a funnel plot assessment for publication bias was not performed as the power of the tests is too low to distinguish chance from actual asymmetry.
- Follow-up time was inconsistent across trials introducing less accurate analyses and unbalanced trial-related contribution to summary estimates.
- Hazard ratio and 95% confidence interval would be the proper outcomes measure to account for both right censoring and available follow-up time trial by trial.
- By splitting comparison of multi-arm trials (i.e., MASS-II and BARI-2D, PCI vs. OMT and CABG vs. OMT), randomization was violated and estimates referred to two-group comparison with the same reference arm. This design of the analyses implied the methodological non-sense of having two times the same group of patients as comparator arm with duplication of OMT arm in the computation of the summary estimate. By using separated analyses, the variance of measured effects would be higher than a three-arm analysis.
Against this background, the only meaningful trade-off would be a three-node network meta-analysis. This design would enable also pooling PCI vs. CABG trials as indirect information for the comparisons PCI vs. OMT and CABG vs. OMT. However, randomization within trials would still be violated. Another simpler solution may be the use of separate analyses PCI vs. OMT and CABG vs. OMT.
Opportunities:
- This analysis serves as an opportunity to review clinically relevant definitions of MI with respect to the type of revascularization adopted, i.e. CABG or PCI.
- The 2 MIs of relevance are periprocedural (type 4a or type 5) and spontaneous (type 1 or type 2) with a higher number of periprocedural MI’s occurring post PCI with little prognostic importance, whilst spontaneous MI’s are more common in the OMT group.
- Future studies should specify the type of MI if it is an endpoint.
- The results of this meta-analysis reinforce that in patients with stable CCS cardiologists can take a stepwise approach to treatment.
- Exclude significant left main stem disease (ideally with CTCA)
- Optimise medical therapy
- Evaluate the extent and severity of ischaemia
- Plan an invasive strategy in patients with recurrent or intolerable symptoms despite OMT…or… offer patients revascularisation up front with a small procedural risk that may, in turn, afford an opportunity to reduce medication burden.
- All patients with CCS are at risk of spontaneous MI regardless of therapeutic strategy, therefore preventive therapies should be addressed in addition to revascularization. These would include colchicine, PCSK9i, etc.
- These data allow for clearer and greater patient involvement in revascularisation decision-making in CCS, promoting patient-specific treatment plans tailored to individual needs and expectations
- This data can be used to inform updated international revascularisation treatment guidelines, some of which continue to include ‘prognostic’ indications for revascularisation in CCS.
Threats:
- In all trials included in this meta-analysis, the patients were carefully selected therefore despite large numbers these patients only represent a small proportion of patients presenting with CCS and stable symptoms. Extrapolating these results to the wider population and suggesting that OMT alone is sufficient may deny potentially beneficial therapy to patients.
- All patients had anatomic evaluation to exclude LMS disease by angiogram or CTCA therefore these results cannot be applied to an unselected population with CCS or patients with known significant LMS disease.
- The number of women remains low in these trials making inferences on ischemia and outcomes after revascularisation difficult.
- LV dysfunction in CCS has been excluded from the majority of studies with the exception of STICH that suggested a survival benefit in those with viability. Therefore, denying this subgroup revascularization cannot be supported by this meta-analysis alone.
- Ischemia testing remains largely dependent on the technology, protocol and reader limiting analyses that rely strictly on ischemia testing without factoring in symptoms or anatomy. Discordant results of such tests further complicate interpretation and the decision-making process.
- Cross over rates from OMT to revascularization ranged from 17-51% in the included trials, given that the analysis was carried out on an intention to treat basis, therefore, the benefit of OMT alone may be overestimated.
- There may still be an inadvertent bias towards a generally healthier population undergoing surgical revascularisation versus revascularisation by PCI (i.e. ‘a good surgical candidate’). This is problematic when considering the mortality as an endpoint for PCI as such patients may be of higher general risk from unmeasured comorbidities
- Oversimplified messaging of trial data (e.g. by main stream media outlets) may erode patient confidence in revascularisation techniques and operators
- All included studies only consider epicardial coronary artery disease. Microvascular disease (e.g. INOCA) was not quantified in these studies and remains prognostically important. This is, therefore, an important confounding factor of all revascularisation trials but is rarely considered. Furthermore, OMT is likely an important modifier of microvascular disease. It is plausible that those who undergo revascularisation decrease or discontinue certain CV medications – this may bias against the optimal treatment of associated (but unmeasured) microvascular dysfunction, with potential implications for endpoints including death and MI.










No comments yet!