Distal radial artery approach to prevent radial artery occlusion trial
Selected in JACC Cardiovascular Interventions by E. Asher
The aim of this study was to compare the rate of proximal RAO with Doppler ultrasound (DUS) between distal and conventional radial access 24 h after a transradial coronary procedure.
References
Authors
Guering Eid-Lidt, Agustín Rivera Rodríguez, Joaquín Jimenez Castellanos, Julio I. Farjat Pasos, Kathia E. Estrada López and Jorge Gaspar
Reference
J Am Coll Cardiol Intv. 2021 Feb, 14 (4) 378–385
Published
February 2021
Link
Read the abstractReviewer
My Comment
Why this study? – the rationale/objective
The radial artery has become the vascular access site of choice for performing diagnostic and percutaneous coronary intervention (PCI) procedures compared with femoral access. The most important benefit of the radial approach is the reduction of vascular complications such as bleeding related vascular access. Nevertheless, the most serious complication of radial approach is radial artery occlusion (RAO), with a 7.5% incidence during the first 24 h and a reduction up to 5.5% at 30 days of follow-up. The distal radial artery (snuffbox approach) has emerged in recent years as a new vascular access alternative for diagnostic procedures and PCI. The aim of the current study was to compare the rate of proximal RAO with Doppler ultrasound (DUS) between distal and conventional radial access 24 h after a transradial coronary procedure.
How was it executed? – the methodology
The DAPRAO (Distal Radial Approach to Prevent Radial Artery Occlusion) trial was a prospective, comparative, longitudinal, randomized, single-center study carried out at the Ignacio Chávez National Institute of Cardiology, Mexico City, Mexico.
- Primary objective: To determinate whether distal radial access was superior to proximal radial access in preventing proximal RAO at 24 h after a diagnostic or interventional coronary procedure evaluated using DUS.
- Secondary objectives:
- a) To compare proximal RAO rates at 30 days and access and fluoroscopy times between the groups.
- b) Safety criteria: The incidence of bruising and bleeding.
- Inclusion criteria:
- a) Patients older than 18 years old who were candidates for coronary diagnostic procedures or PCI via the radial access.
- b) The presence of a perceptible pulse from the radial artery in its proximal and distal segments.
- Exclusion criteria:
- a) Patients with ST-segment elevation myocardial infarction
- b) cardiogenic shock
- c) patients in whom the main operator did not perceive the arterial pulse
- d) patients in whom the operator decided to perform the procedure via the femoral route.
- Patients were randomly assigned.
- All patients received a “cocktail” of 5,000 IU unfractionated heparin [UFH], 2.5 mg Verapamil and 200 mg nitroglycerin. In cases of PCI, an additional dose of UFH was administered to complete a total dose of 100 IU/kg.
- A pneumatic band (TR Band, Terumo) was placed in both groups, at the site of the arterial Puncture. In case of distal radial artery puncture, the rigid plastic support was removed from the device.
- PRAO was defined as absence of flow on color DUS and absence of pulse wave on pulsed DUS.
What is the main result?
- A total of 286 patients were randomized into 2 groups, 144 to group 1 (proximal radial) and 142 to group 2 (distal radial). Two patients in each group were eliminated because post- procedural DUS studies were not performed.
- The average age of the patients was 62.0 (±10.8 years) while most were men (75.9%).
- The mean diameter of the proximal radial artery by DUS was 2.7 (± 0.4) mm and of the distal segment was 2.4 (± 0.5) mm.
- The number of attempts (more than 1) to puncture the artery was greater in the distal radial artery group (47.8% vs. 24.6%; p=0.001).
- Primary objective: PRAO at 24 h was 8.4% in the proximal group and 0.71% in the distal group (OR:12.8; 95% CI: 1.6-100.0; p=0.002). At 30 days, the rates of PRAO were 5.6% and 0.71%, respectively (OR: 8.2; 95% CI: 1.0-67.2; p=0.019).
- The incidence of hematoma was 9.8% in the proximal radial group and 7.8% in the distal radial group (p= 0.35).
- The incidence of spasm was similar in both groups (4.2% vs. 3.5%; p= 0.51).
- Crossover to the opposite forearm was more frequent when the initial allocated approach was distal radial access (13.3% vs. 0.7%; p=0.0001).
- The only independent predictor of PRAO at 24 h was proximal radial access (OR: 12.8; 95% CI: 1.6-100.0; p= 0.015). The relative risk reduction of PRAO at 24 h with distal radial access was 96%.
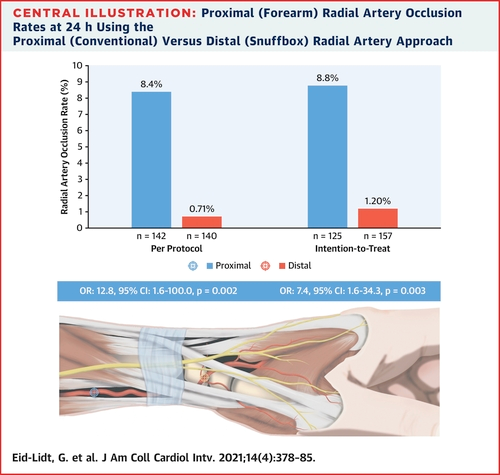
Proximal (Forearm) Radial Artery Occlusion Rates at 24 h using the Proximal (Conventional) Versus Distal (Snuffbox) Radial Artery Approach.
Source: JACC: Cardiovascular Interventions
Critical reading and the relevance for clinical practice:
In this prospective, randomized (although single center study) the rate of PRAO evaluated using DUS 24 h after the procedure was significantly lower in the group with distal radial access compared with the standard proximal radial access meeting criteria for superiority. Interestingly, there was an early PRAO rate of 8.4% (in line with what has been previously reported) but at 30 days, there was a significant reduction of 5.6% in the rate of PRAO. The fact that there was a low rate of PRAO (<1%) of the radial artery when distal radial access was used as the initial approach is very important. Moreover, the rate of bleeding and the vascular access and fluoroscopy times were similar in both groups.
Should common practice and guidelines be changed in favor of distal radial artery access?
The study had several limitations: First, it was a single center study. Moreover, it was a relatively small study. Lastly, the study did not include patients with STEMI or cardiogenic shock. Nevertheless, the execution of the study was simple and elegant.
What is your approach regarding the radial access for coronary procedures? Do you think one should change his/her common practice regarding radial access towards distal radial access?





No comments yet!