Fractional flow reserve to guide treatment of patients with multivessel coronary artery disease - the FUTURE trial
Selected in JACC by N. Ryan
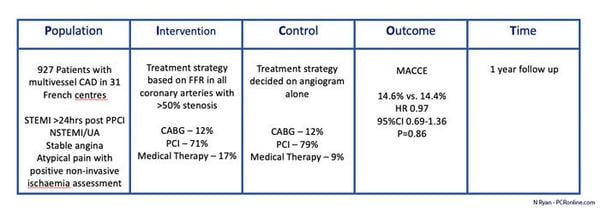
The FUTURE Trial is a prospective randomised, multicentre, open label superiority trial comparing an FFR guided treatment strategy to traditional angiography guided treatment strategy on clinical outcomes in an all-comer population with multivessel coronary artery disease.
References
Authors
Gilles Rioufol, François Dérimay, François Roubille, Thibault Perret, Pascal Motreff, Denis Angoulvant, Yves Cottin, Ludovic Meunier, Laura Cetran, Guillaume Cayla, Brahim Harbaoui, Jean-Yves Wiedemann, Éric Van Belle, Christophe Pouillot, Nathalie Noirclerc, Jean-François Morelle, François-Xavier Soto, Christophe Caussin, Bernard Bertrand, Thierry Lefèvre, Patrick Dupouy, Pierre-François Lesault, Franck Albert, Olivier Barthelemy, René Koning, Laurent Leborgne, Pierre Barnay, Philippe Chapon, Sébastien Armero, Antoine Lafont, Christophe Piot, Camille Amaz, Bernadette Vaz, Lakhdar Benyahya, Yvonne Varillon, Michel Ovize, Nathan Mewton, Gérard Finet, and FUTURE Trial Investigators
Reference
10.1016/j.jacc.2021.08.061
Published
November 2021
Link
Read the abstract
Reviewer
Latest contributions
Balloon lithotripsy added to conventional preparation before stent implantation in severely calcified coronary lesions Impact of pullback pressure gradient on clinical outcomes after percutaneous coronary interventions Validation of intravascular ultrasound-defined optimal stent expansion criteria for favorable 1-year clinical outcomesMy Comment
Why this study – the rationale/objective?
In stable patients FFR guided PCI has been proven beneficial compared to angiography alone and is guideline endorsed. The FUTURE trial aimed to assess the benefit of FFR guidance in determining treatment strategy (medical management, PCI, CABG) on clinical outcomes in an all-comer population with multivessel CAD.
How was it executed? - the methodology
Patients with ≥ 50 % stenosis in at least two vessels ≥ 2.5 mm in diameter or ≥ 50 % in the LMS were eligible for inclusion. All presentations of CAD were considered; if the initial presentation was STEMI the culprit artery was not included in the multivessel status whilst in NSTEMI/unstable angina the culprit artery was included and treated according to current guidelines. Patients were randomised 1:1 to an FFR guided treatment strategy (CABG, PCI, medical therapy) or Control group (treatment strategy guided by angiography and any prior non-invasive tests). Protocol recommended revascularisation of any lesions with an FFR < 0.80, CTO’s were eligible for inclusion if they supplied viable territory and were assigned an FFR of 0.50.
- The primary endpoint was MACCE a composite of death from any cause, nonfatal MI, stroke or any unplanned revascularisation at one year.
- Secondary endpoints were the individual components of the primary endpoint.
The power calculation for the trial estimated that 1,728 patients would be required to have an 80 % power to detect a 30 % reduction in risk in the FFR guided arm. The trial was prematurely stopped after enrolment of 941 patients due an interim safety analysis showing increased mortality in the FFR group.
What is the main result?
Overall 927 patients were included in the ITT analysis, the majority were male in their 60’s with a high prevalence of traditional CVRFs. Approximately 1/5 of participants had a prior MI and a quarter prior PCI with no significant differences between the groups.
- Almost half the population presented with an ACS (FFR 47 % vs. Control 46 %, p=0.64), of these 20% of the FFR group and 19 % of the Control group were enrolled post PPCI for STEMI.
- Comparing revascularisation strategies CABG rates were similar among the groups, in the FFR group more patients were treated with optimal medical therapy alone, with more PCI in the control group (p = 0.002)
- In the FFR group 43 % of lesions were FFR negative however 11.5 % underwent PCI and 16.9 % had bypass grafts placed.
- At one year, there was no difference in MACCE between the groups (FFR 14.6 % vs. control 14.4%, HR 0.97 95 % CI 0.69-1.36, p = 0.85).
- All-cause mortality was 3.7 % vs. 1.5 %, HR 2.34, 95 % CI 0.97-5.18, p = 0.06 and cardiovascular mortality 2.6 % vs. 1.5%, HR 2.37, 95 %CI 0.83-6.76, p = 0.11 in the FFR and control groups respectively.
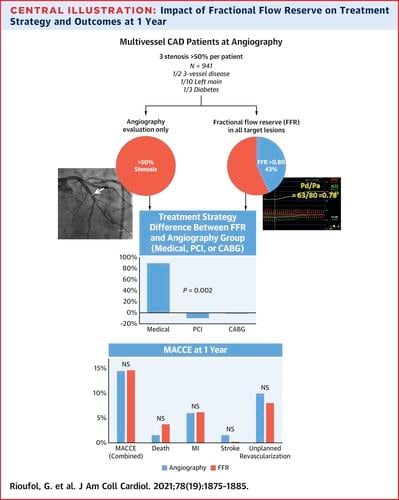
Source: JACC
Critical reading and the relevance for clinical practice
The results of this study fail to show that an FFR guided treatment strategy is superior to traditional angiography ± non-invasive assessment of ischaemia in an unselected group of patients presenting with multivessel coronary artery disease. A key limitation that must be acknowledged in any interpretation of this study is the early termination of recruitment due to a signal of increased mortality in the FFR guided group which ultimately did not reach statistical significance in the final analysis. The early termination led to the study being underpowered to determine any benefit for an FFR guided strategy on clinical outcomes.
The authors included a heterogenous group of patients ranging from those with recent STEMI and PPCI to atypical chest pain and positive ischaemia testing. The role of FFR in stable CAD is well established however trials of patients presenting with ACS have produced mixed results. Whilst subgroup analysis did not show any difference in the ACS versus stable populations in this trial the overall numbers in each group are low. Prior studies have shown higher MACE rates following physiologically guided deferral of PCI in patients with ACS compared to stable CAD, possibly due to microvascular dysfunction and adenosine resistance. The relatively high percentage of ACS patients included in this study once again raises the question of plaque vulnerability and inflammation in the context of ACS, the COMBINE-FFR study showed that high-risk plaque characteristics (i.e. TCFA) on OCT in non-culprit lesions were the strongest predictor of MACE despite negative FFR.
Whilst FFR guided PCI has been incorporated into the guidelines based on prior studies the role of FFR guidance in CABG is less well defined. In this trial despite a higher SYNTAX Score in the control group (26 ± 9 vs. 24 ± 6, p=0.034) there were no differences in the number of anastomoses or arterial anastomoses between the two groups. Despite protocol recommendations 16.9% of FFR negative lesions were treated with bypass grafts. Again, at subgroup analysis there were no statistically significant differences between groups based on treatment strategy however small numbers limit the conclusions that can be drawn from this.
Finally the complexity of the patients enrolled in the FUTURE Trial was relatively high with a mean SYNTAX Score of 19 ± 8, with LMS stenosis in 10% of patients and a third of patients diabetic. In these patients FFR may not be as valuable in determining revascularisation strategies as in those with anatomically less complex disease. Indeed at multivariate analysis LVEF < 40 % (HR 2.33, 95 % CI 1.07-4.64, p = 0.02) and SYNTAX Score > 32 (HR 3.36, 95 % CI 1.39-7.65, p < 0.001) were associated with increased MACCE. This suggests that the overall burden of CAD throughout the coronary tree may be more important than ischaemia at an individual lesion level in patients with complex coronary disease. Overall the rates of complete revascularisation were low in both the FFR and control groups, given that completeness of revascularisation influences longer term outcomes the outcomes of patients with complete versus incomplete revascularisation would be of interest.
Overall given the early termination of the trial and loss of statistical power along with the heterogeneity of the population it is difficult to draw definitive conclusions from the FUTURE trial. Whilst FFR increased the number of patients treated with medical therapy alone this did not translate into differences in clinical outcomes. The results of FUTURE suggest that routine use of FFR in an unselected patient population may not be as beneficial as its use in selected patients and lesion types. Finally ischaemia alone may not be the sole determinant of outcomes particularly in patients with unstable presentations where anatomical complexity and plaque phenotype contribute to clinical outcomes.
Source: courtesy of Nicola Ryan





No comments yet!