21 Dec 2021
Iatrogenic atrial septal defects following transcatheter mitral valve repair and implications of interventional closures
Selected in JACC: Cardiovascular Interventions by S. Brugaletta
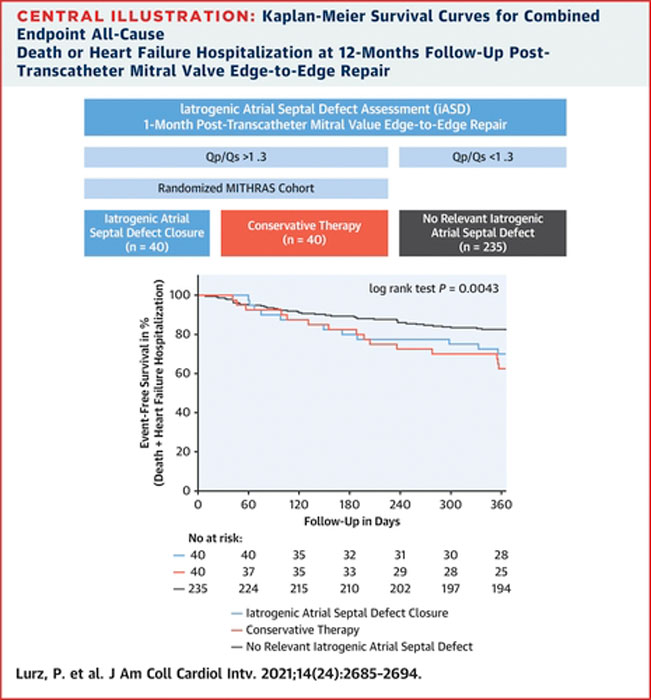
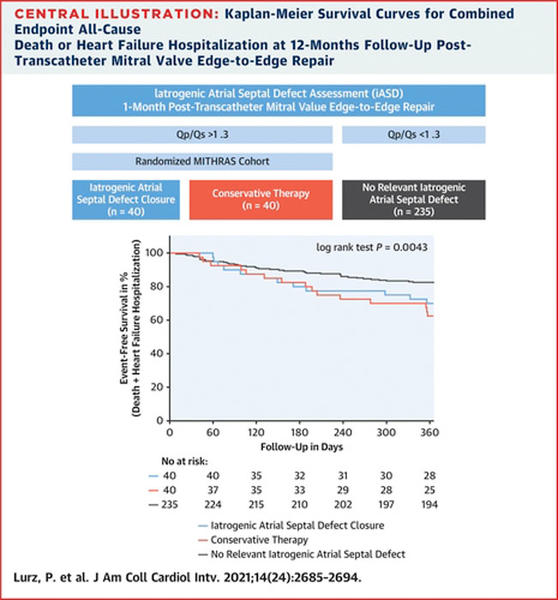
The authors investigated whether iatrogenic atrial septal defect closure post-transcatheter mitral valve edge-to-edge repair is superior to conservative therapy, and whether outcomes (death/heart failure hospitalization) differ between patients with and without an iASD post-TMVR.
References
Authors
Philipp Lurz, Matthias Unterhuber, Karl-Philipp Rommel, Karl-Patrik Kresoja, Tobias Kister, Christian Besler, Karl Fengler, Marcus Sandri, Ingo Daehnert, Holger Thiele, Stephan Blazek, and Maximilian von Roeder
Reference
J Am Coll Cardiol Intv. 2021 Dec, 14 (24) 2685–2694
Published
December 14, 2021
Link
Read the abstract
Reviewer
My Comment
Why this study – the rationale/objective?
Transseptal access for TMVR can create an iASD, which is associated with impaired outcomes. Controversially, the creation of an iASD in HF has been linked to improved hemodynamics.
The authors investigated whether iatrogenic atrial septal defect (iASD) closure post-transcatheter mitral valve edge-to-edge repair (TMVR) is superior to conservative therapy (CT), and whether outcomes (death/heart failure [HF] hospitalization) differ between patients with and without an iASD post-TMVR.
How was it executed? - the methodology
80 patients with an iASD and relevant left-to-right shunting (Qp:Qs ≥ 1.3) 30 days following TMVR were randomized to CT or interventional closure of the iASD (MITHRAS [Closure of Iatrogenic Atrial Septal Defect Following Transcatheter Mitral Valve Repair] cohort), and 235 patients without an iASD served as a comparative cohort.
What is the main result?
All patients of the MITHRAS cohort (mean age 77 ± 9 years, 39 % women) received their allocated treatment, and follow-up was completed for all MITHRAS and comparative cohort (mean age 77 ± 8 years, 47 % women) patients.
Twelve months post-TMVR, there was no significant difference in the combined endpoint of death or HF hospitalization within the MITHRAS cohort (iASD closure: 35 % vs CT 50 %; P = 0.26).
The combined endpoint was more frequent among patients within the MITHRAS cohort, as opposed to the comparative cohort (43 % vs 17 %; P < 0.0001), primarily driven by a higher rate of HF hospitalization (34 % vs 8 %; P = 0.004).
Source: JACC - Cardiovascular Interventions
Critical reading and the relevance for clinical practice
This interesting randomized controlled trial shows that patients with an iASD are at higher risk for HF hospitalization.
Closure of Iatrogenic Atrial Septal Defect Following Transcatheter Mitral Valve Repair, interventional closure of a relevant iASD 1 month after TMVR did not result in improved clinical outcomes at 12 months post-TMVR.
There are some important messages coming from this paper. First, it is of note to see that after transeptal access for TMVR, those patients need to be closely followed for evaluating the entity of the residual left-to-right shunt. In clinical practice, it is rare to see that Qp:Qs is measured in these patients: this is something that should be done because it is related to their outcomes and in particular with subsequent hospitalization for heart failure. Second, it is important to see that early percutaneous closure of such defect does not result in an improvement of patients' prognosis. This means that other kinds of treatment should be explored in order to overcome this Achilles' heel of the TMVR.