Association of medication adherence with health outcomes in the ISCHEMIA Trial
Selected in JACC : Journal of the American College of Cardiology by M. Alasnag , H. Naung Tun
This sub-analysis of ISCHEMIA has shown that implementation of a simple protocol of optimal medical therapy is a key factor to improve health outcome and practical in real-world settings.
References
Authors
R. Angel Garcia, John A. Spertus, Mary C. Benton, Philip G. Jones, Daniel B. Mark, Jonathan D. Newman, Sripal Bangalore, William E. Boden, Gregg W. Stone, Harmony R. Reynolds, Judith S. Hochman, David J. Maron, and on behalf of the ISCHEMIA Research Group
Reference
J Am Coll Cardiol. 2022 Aug, 80 (8) 755–765
Published
August 2022
Link
https://www.jacc.org/doi/full/10.1016/j.jacc.2022.05.045Reviewers
Our Comment
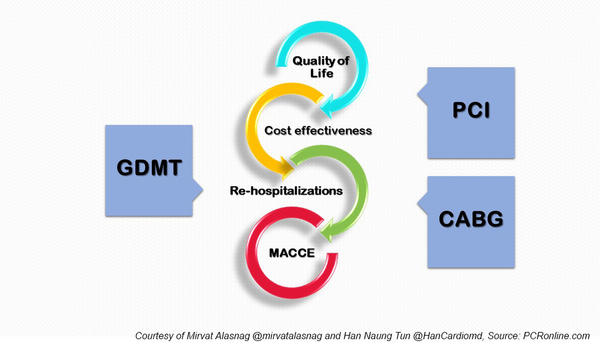
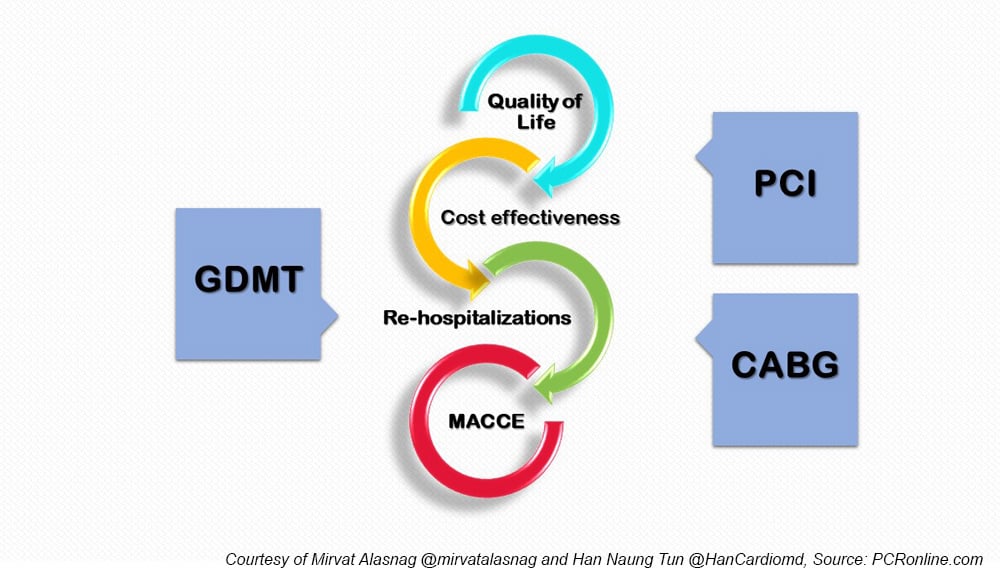
Endpoints for patients with stable coronary artery disease - figure courtesy of Mirvat Alasnag and Han Naung Tun
Why this study – the rationale/objective?
Several landmark interventional trials have been published in recent years guiding clinical practice, including the Cardiovascular Outcomes Assessment of the MitraClip Percutaneous Therapy for Heart Failure Patients with Functional Mitral Regurgitation (COAPT) trial, and the Objective Randomised Blinded Investigation With Optimal Medical Therapy of Angioplasty in Stable Angina (ORBITA) trial1-2.
Such studies have informed practice in the interventional space with respect to cardiovascular outcomes. A cornerstone of such trials is guideline directed medical therapy (GDMT), which is too often overlooked when analyzing practice-changing trials.
Even the historic studies evaluating the role of coronary artery bypass grafting (CABG) versus percutaneous coronary intervention (PCI) such as Medicine, Angioplasty, or Surgery Study (MASS-2) did so on a background of GDMT3.
However, over the decades, medical therapy for both risk factor modification and heart failure has evolved remarkably, making those trials obsolete.
A more contemporary landmark study is the renowned International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial4. This trial assessed patients with stable coronary disease and moderate or severe ischemia. The investigators noted no advantage of an initial invasive strategy compared with an initial conservative strategy with respect to the risk of ischemic cardiovascular events or death from any cause over a median follow-up of 3.2 years.
Since one arm of this randomized trial consisted of a conservative strategy, it is important to analyze a medical therapy and understand how adherence impacted outcomes. Therefore, ensuring access to providers across the continuum of invasive care and empowering patients to understand the treatment regimen, and its benefits are critical strategies to improve medication adherence.
How was it executed – the methodology?
Briefly, the ISCHEMIA trial enrolled after individuals with moderate or severe ischemia. A coronary computed tomography angiography was performed and those with significant left main coronary artery disease were excluded.
Other exclusion criteria were estimated glomerular filtration rate < 30 mL/min/1.73 m2, an acute coronary syndrome within 2 months of randomization, left ventricular ejection fraction < 35 %, New York Heart Association functional class III to IV heart failure, and unacceptable angina despite maximally tolerated GDMT.
Eligible patients were then randomized to an invasive strategy including GDMT with coronary angiography and possible revascularization (invasive therapy), or GDMT alone (conservative therapy) with coronary angiography and revascularization reserved for failure of medical therapy.
GDMT consisted of antianginal medications and secondary prevention with pharmacologic and lifestyle intervention applied equally to both groups using treat-to-target algorithms. Follow-up was conducted at 1.5, 3, 6, and 12 months, and every 6 months until the completion of the study protocol.
This was a pre-specified sub-analysis hypothesizing that nonadherent patients would register better outcomes randomized to an invasive strategy. Investigators captured self-reported medication-taking behavior at randomization, using a modified 4-item Morisky-Green-Levine Adherence Scale. A twelve-month health status was assessed with the 7-item Seattle Angina Questionnaire (SAQ-7) summary score (SS). The association of adherence with outcomes was subsequently evaluated using Bayesian proportional odds models, including an interaction by study arm (conservative versus invasive).
What is the main result?
A total of 4,480 completed the quality of life questionnaires and were included with only 1,245 (27.8 %) deemed nonadherent at the outset. Compared with adherent participants, nonadherent patients were younger (63.6 vs 64.7 years of age), more likely to be smokers (16.4 % vs 11.9 %), and more likely to have worse baseline health status: lower baseline scores on the SAQ-7 summary (71.9 ± 19.6 vs 74.9 ± 18.5), physical limitation (76.9 ± 24.4 vs 80.3 ± 23.1), and quality-of-life (58.9 ± 27.2 vs 62.9 ± 25.9 vs) scales.
In adjusted analyses, adherence was associated with higher 12-month SAQ-7 SS in both treatment groups (mean difference in SAQ-7 SS with conservative treatment = 1.6 [95 % credible interval: 0.3-2.9] vs with invasive management = 1.9 [95 % credible interval: 0.8-3.1]), with no interaction by treatment. The SAQ-7 domains of angina frequency, physical limitation, and quality of life were also consistent. A secondary analysis of the dose-response effect adherence on health status outcomes noted a graded effect of adherence scores, with higher scores of adherence being associated with higher SAQ-7 summary scores.
Nonadherence was associated with worse symptoms and decreased health status in both arms of the trial with indication that these patients extract greater benefit from an invasive strategy.
Critical reading and relevance for clinical practice
Adherence, or lack of, is an ongoing challenge in the field. Several studies have indicated the impact of nonadherence on outcomes in patients with coronary artery disease, including those who have undergone revascularization5. As such, it is tempting to consider an invasive approach for those less likely to adhere to medications. However, this sub-study clearly demonstrates a lack of benefit. Moreover, it makes one wonder whether the risk of stent thrombosis is higher in those who are less inclined to take a dual antiplatelet regimen. It would make more sense in that case to avoid PCI.
What is alarming, though, is the worse outcomes in both arms compared with those who were adherent indicating the critical role of up titrating medical therapy. The practical question remains how that is to be achieved. In the ORBITA and ISCHEMIA trials, investigators follow-up patients closely and intensified medical therapy. In real-world settings, these are burdensome and almost unrealistic expectations of modern-day healthcare systems suffering from staff shortages6. Whether the failure to optimize medical therapy is a precursor to poor outcomes remains unanswered by this study. Although this analysis is valuable, it does not shed light on reasons for lack of adherence where improvements can be made; for example, socioeconomic factors or education. Finally, adherence is not binary. Patterns of behavior wax and wane with patients being more inclined to adhere when symptoms intensify. Such patterns cannot be captured in a questionnaire.
The study by Garcia et al paves the way to many questions that we hope future landmark trials address, namely, quality of life and cost-effectiveness. These are particularly important as the evidence to date suggests that PCI in stable coronary disease does not improve cardiovascular outcomes. Perhaps more objective assessments of quality of life should be considered such as six-minute walk or repeat hospitalizations. These, in particular, may be valuable with increasing co-morbidity and age.
Reynolds et al. also validated that ischemia severity was not associated with increased risk after adjustment for CAD severity and all-cause mortality at 4 years. Invasive management did not lower all-cause mortality in any ischemia or CAD subgroup7. Hence, medication non-adherence in CAD might be significantly associated with increased morbidity with hospitalization and all-cause mortality. This analysis also suggests that it is imperative to monitor and address medication adherence in patients with CAD in both invasive and non-invasive groups to reduce hospitalization, improve clinical outcomes and reduce healthcare costs.
Overall, this sub-analysis of ISCHEMIA has shown that implementation of a simple protocol of optimal medical therapy is a key factor to improve health outcome and practical in real-world settings, and it also generates new hypotheses and study methodology on how optimization with GDMT and medication adherence can be considered in further clinical studies with invasive approach.
References:
- Stone GW, Lindenfeld J, Abraham WT, Kar S, Lim DS, Mishell JM, Whisenant B, Grayburn PA, Rinaldi M, Kapadia SR, Rajagopal V, Sarembock IJ, Brieke A, Marx SO, Cohen DJ, Weissman NJ, Mack MJ; COAPT Investigators. Transcatheter Mitral-Valve Repair in Patients with Heart Failure. N Engl J Med. 2018 Dec 13;379(24):2307-2318. doi: 10.1056/NEJMoa1806640. Epub 2018 Sep 23.
- Al-Lamee R, Thompson D, Dehbi HM, Sen S, Tang K, Davies J, Keeble T, Mielewczik M, Kaprielian R, Malik IS, Nijjer SS, Petraco R, Cook C, Ahmad Y, Howard J, Baker C, Sharp A, Gerber R, Talwar S, Assomull R, Mayet J, Wensel R, Collier D, Shun-Shin M, Thom SA, Davies JE, Francis DP; ORBITA investigators. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial. Lancet. 2018 Jan 6;391(10115):31-40. doi: 10.1016/S0140-6736(17)32714-9. Epub 2017 Nov 2. Erratum in: Lancet. 2018 Jan 6;391(10115):30.
- Hueb W, Soares PR, Gersh BJ, César LA, Luz PL, Puig LB, Martinez EM, Oliveira SA, Ramires JA. The medicine, angioplasty, or surgery study (MASS-II): a randomized, controlled clinical trial of three therapeutic strategies for multivessel coronary artery disease: one-year results. J Am Coll Cardiol. 2004 May 19;43(10):1743-51. doi: 10.1016/j.jacc.2003.08.065.
- Maron DJ, Hochman JS, Reynolds HR, Bangalore S, O'Brien SM, Boden WE, Chaitman BR, Senior R, López-Sendón J, Alexander KP, Lopes RD, Shaw LJ, Berger JS, Newman JD, Sidhu MS, Goodman SG, Ruzyllo W, Gosselin G, Maggioni AP, White HD, Bhargava B, Min JK, Mancini GBJ, Berman DS, Picard MH, Kwong RY, Ali ZA, Mark DB, Spertus JA, Krishnan MN, Elghamaz A, Moorthy N, Hueb WA, Demkow M, Mavromatis K, Bockeria O, Peteiro J, Miller TD, Szwed H, Doerr R, Keltai M, Selvanayagam JB, Steg PG, Held C, Kohsaka S, Mavromichalis S, Kirby R, Jeffries NO, Harrell FE Jr, Rockhold FW, Broderick S, Ferguson TB Jr, Williams DO, Harrington RA, Stone GW, Rosenberg Y; ISCHEMIA Research Group. Initial Invasive or Conservative Strategy for Stable Coronary Disease. N Engl J Med. 2020 Apr 9;382(15):1395-1407. doi: 10.1056/NEJMoa1915922. Epub 2020 Mar 30.
- Spertus JA, Kettelkamp R, Vance C, Decker C, Jones PG, Rumsfeld JS, Messenger JC, Khanal S, Peterson ED, Bach RG, Krumholz HM, Cohen DJ. Prevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug-eluting stent placement: results from the PREMIER registry. Circulation. 2006 Jun 20;113(24):2803-9. doi: 10.1161/CIRCULATIONAHA.106.618066. Epub 2006 Jun 12.
- Riley RF, Alasnag M, Batchelor WB, Sharma A, Luse E, Drewes M, Welt FG, Itchhaporia D, Henry TD. The Ongoing National Medical Staffing Crisis: Impacts on Care Delivery for Interventional Cardiologists. J Soc Cardiovasc Angiogr Interv. 2022 May-Jun;1(3):100307.
- Reynolds HR, Shaw LJ, Min JK, et al. Outcomes in the ISCHEMIA Trial Based on Coronary Artery Disease and Ischemia Severity [published correction appears in Circulation. 2022 Jun 7;145(23):e1072] [published correction appears in Circulation. 2022 Jul 5;146(1):e3]. Circulation. 2021;144(13):1024-1038.






No comments yet!