21 Dec 2022
Distal radial artery access for recanalization of radial artery occlusion and repeat intervention: a single centre experience
Selected in Journal of Clinical medicine by A. Cader , A. N. Calik
This pilot study aimed to investigate the feasibility, safety, and efficacy (long-term patency) of the recanalization of chronic RAO via DRA7.
References
Authors
Alexandru Achim, Kornél Kákonyi, Zoltán Jambrik, Dorottya Olajos, Attila Nemes, Olivier F. Bertrand, and Zoltán Ruzsa
Reference
J. Clin. Med. 2022, 11(23), 6916
Published
23 November 2022
Link
Read the abstract
Reviewers
Our Comment
Why this study – the rationale/objective?
Radial artery occlusion (RAO) is the commonest complication of conventional transradial access (TRA)1. An occluded radial artery precludes its future use for percutaneous procedures, necessitating alternative access1.
The distal radial access (DRA) is an alternative access site for percutaneous procedures, with the advantage that it remains patent, even with forearm RAO due to its anatomical location2. First described as a means of accessing and recanalizing the occluded proximal radial artery segment, 3DRA thus provides an option to perform retrograde angioplasty of the occluded radial artery in the forearm.
While this has been reported in case reports and small case series, there is a need for larger registries to identify the prevalence of complications of radial angioplasty (perforation, hematoma, digital ischemia)4, and its long-term patency5,6.
This pilot study aimed to investigate the feasibility, safety, and efficacy (long-term patency) of the recanalization of chronic RAO via DRA7.
How was it executed? - the methodology
This proof-of-concept prospective study included 30 consecutive patients with RAO undergoing coronary angiogram via DRA7. Patients with hemodynamic instability (STEMI/NSTEMI or cardiogenic shock) and cases of hypoplastic radial artery were excluded. All procedures were performed by two operators experienced in DRA.
Recanalization procedure:
Ultrasound-guided DRA was performed in all participants, which also allowed the diagnosis of RAO during puncture preparation. Intraluminal access via a 21-gauge needle was confirmed by the ultrasound probe, followed by contrast injection directly through the needle visualising the occlusion.
If partial advancement of the standard puncture guidewire (0.018”) was possible (for more proximal occlusions), the 5- or 6-French sheath was partially inserted, and angiography performed through it. Otherwise, the guidewire was advanced through the 21-gauge needle or via the introducer needle inserted into the sheath valve.
Under fluoroscopy, dedicated polymer-jacket hydrophilic chronic total occlusion (CTO) coronary or peripheral guidewires were advanced through the occlusion, either by intraluminal tracking (true lumen, through CTO microchannels) or by subintimal tracking and reentry, which is easily performed with the Gladius knuckle. When the tip of the wire freely entered the brachial artery, a sheathless catheter was advanced over the wire through the occlusion by a push-and-rotate manoeuvre (similar to “dotterization”). After successfully achieving RAO recanalization by advancing the sheathless system without the need for balloon angioplasty, the procedure ended with patent hemostasis.
Endpoints:
The feasibility endpoint was procedural success, defined as successful flow restoration from the brachial artery all along the radial artery until the two palmar arches, assessed by angiography at the end of the procedure. Only stable, normal flow (the equivalent of TIMI III) was considered procedural success.
The efficacy endpoint was the radial artery patency at 30 days, verified by ultrasound Doppler signal.
The safety endpoint was a composite of the absence of (i) intra- or periprocedural major vascular complications such as haematoma EASY 3–4, digital ischemia, thrombus migration to brachial/ulnar artery, and compartment syndrome and (ii) major adverse cardiac and cerebrovascular events (MACCE) defined as transient ischemic attack, stroke, myocardial infarction, and cardiac-related death.
What is the main result?
Thirty consecutive patients with RAO were enrolled in the study, half of whom were women (n = 15). The mean age was 63 ± 11 years. The vast majority of the patients had asymptomatic RAO (n = 28, 93.3 %), with only two (6.6 %) reporting numbness of hands. 70 % received right DRA, while 30 % received left DRA.
Feasibility:
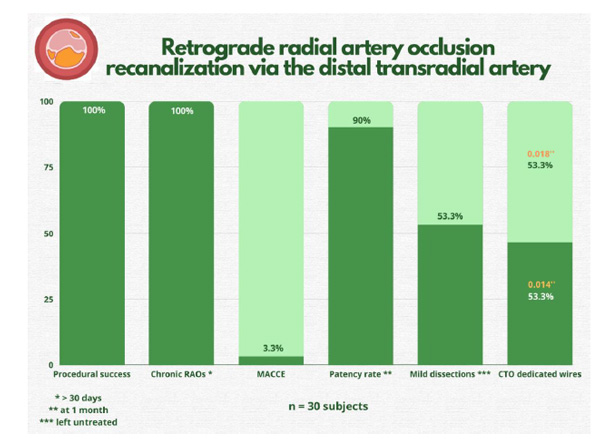
Procedural success through retrograde wiring was 100 % (n = 30), demonstrating feasibility of the technique. All cases were performed by the “dottering” technique with the sheathless system.
All occlusions were chronic (n = 30, 100 %). The majority (53 %) were recanalized using 0.018” hydrophilic guidewires. More than one type of guidewires were required in 23 % of cases. Gladius (Asahi Intecc, Nagoya, Japan) (either 0.018′′ or 0.014′′) was the most frequently used guidewire (63 % of cases). No cases required a local thrombolytic agent or mechanical thrombaspiration. The technique also did not require large amounts of contrast (mean 140 ± 28 mL) or procedure time (mean 41 ± 22 minutes) for entire intervention.
Safety:
There were no major vascular complications; one angiographically visible perforation (3 %) and only two EASY 1–2 hematomas (10 %) were observed. Despite several non-flow limiting dissections (n = 16, 53 %), all patients had a good flow at the end of the procedure, confirmed by upper limb angiography. A single case of periprocedural stroke was reported (3 %), with onset immediately after sheath removal and recovering 24 hours later, with no large vessel occlusion on urgent computed tomography angiography.
Efficacy:
Twenty seven of the radial arteries (90 %) remained patent at one-month follow-up, and three re-occluded.
Figure : Important study endpoints. RAO = radial artery occlusion; MACCE = major adverse cardiac and cerebrovascular events; CTO = chronic total occlusion.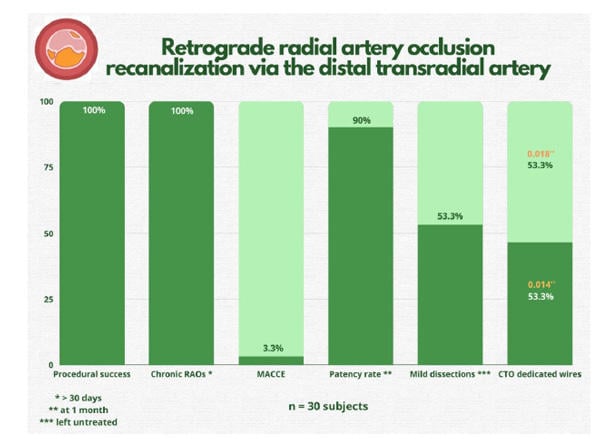
Source: Journal of Clinical Medicine
Critical reading and the relevance for clinical practice
This study offers preliminary evidence of the feasibility and efficacy of retrograde recanalization via DRA, as a treatment option for chronic forearm RAO7. There is increasing evidence of the safety of DRA, including reduced haemostasis time, less forearm RAO and no impairment of hand function8–10.
This pilot study provides some reassuring data in that the same coronary CTO techniques can be applied to reopen a radial CTO via retrograde DRA access, with no need for balloon angioplasty. Gasparini et al. described a similar balloonless technique of wiring directly through the needle (using only 0.014” polymer-jacket coronary guidewires with subintimal tracking and reentry technique used in 80 % of cases); their series of 7 patients demonstrated a 71 % success rate4. The safety of directly using a sheathless catheter over the 0.0018” CTO guidewire was also demonstrated, thus reducing radiation, procedure time and contrast injections which may have occurred due to repeated balloon dilatations.
It is also encouraging that 30-day patency rates in this study are high (90 %). In contrast, a single arm study of 44 patients in China, where balloon angioplasty was also used, had a procedural success of 88.6 %, and much lower radial artery patency rates of 48.7, 43.6, and 35.9 %, at 3, 6, and 12 months were respectively6.
Thus, while a recanalized RAO might allow the radial access for further procedures, in the absence of data, its use as a bypass conduit for CABG or as radial artery–cephalic vein arteriovenous fistula for dialysis is certainly not advised.
The single periprocedural stroke does remain a concern, albeit this being a series of chronic RAO. Prior literature reports the need for balloon dilatation in a case of hand ischaemia, with use of tissue plasminogen activator and thrombus aspiration11.
This study is limited in that it is a small, single centre, non-randomised pilot, and thus further data are warranted to support these preliminary results.
References
- Bernat I, Aminian A, Pancholy S, Mamas M, Gaudino M, Nolan J, et al. Best Practices for the Prevention of Radial Artery Occlusion After Transradial Diagnostic Angiography and Intervention: An International Consensus Paper. Cardiovasc Interv [Internet]. 2019 Nov 25 [cited 2022 Jul 19];12(22):2235–46. Available from: https://www.jacc.org/doi/10.1016/j.jcin.2019.07.043
- Sgueglia GA, Di Giorgio A, Gaspardone A, Babunashvili A. Anatomic Basis and Physiological Rationale of Distal Radial Artery Access for Percutaneous Coronary and Endovascular Procedures. JACC Cardiovasc Interv. 2018 Oct 22;11(20):2113–9.
- Babunashvili A, Dundua D. Recanalization and reuse of early occluded radial artery within 6 days after previous transradial diagnostic procedure. Catheter Cardiovasc Interv. 2011 Mar 1;77(4):530–6.
- Sanz-Sánchez J, Regazzoli D, Petriello G, Leone PP, Reimers B, Gasparini GL. The Last Broken Barrier: Retrograde Radial Artery Recanalization Prior to Transradial Coronary Interventions. Cardiovasc Revascularization Med. 2021 Jul 1;28:125–6.
- Li F, Shi GW, Zhang BF, Yu XL, Huang HM, Xiao JQ, et al. Recanalization of the occluded radial artery via distal transradial access in the anatomic snuffbox. BMC Cardiovasc Disord [Internet]. 2021 Dec 1 [cited 2022 Dec 13];21(1):1–4. Available from: https://bmccardiovascdisord.biomedcentral.com/articles/10.1186/s12872-021-01890-1
- Lin Y, Bei W, Liu H, Liu Q, Yuan J, Wu M, et al. Retrograde recanalization of radial artery occlusion via the distal transradial artery: A single-center experience. Front Cardiovasc Med [Internet]. 2022 Sep 23 [cited 2022 Dec 13];9. Available from: /pmc/articles/PMC9543139/
- Achim A, Kákonyi K, Jambrik Z, Olajos D, Nemes A, Bertrand OF, et al. Distal Radial Artery Access for Recanalization of Radial Artery Occlusion and Repeat Intervention: A Single Center Experience. J Clin Med [Internet]. 2022 Nov 23 [cited 2022 Dec 13];11(23):6916. Available from: https://www.mdpi.com/2077-0383/11/23/6916
- Ferrante G, Condello F, Rao S V., Maurina M, Jolly S, Stefanini GG, et al. Distal vs Conventional Radial Access for Coronary Angiography and/or Intervention: A Meta-Analysis of Randomized Trials. Cardiovasc Interv [Internet]. 2022 Nov 28 [cited 2022 Nov 29];15(22):2297–311. Available from: https://www.jacc.org/doi/10.1016/j.jcin.2022.09.006
- Aminian A, Sgueglia GA, Wiemer M, Gasparini GL, Kefer J, Ruzsa Z, et al. Distal versus conventional radial access for coronary angiography and intervention: Design and rationale of DISCO RADIAL study. Am Heart J. 2022 Feb 1;244:19–30.
- Yokota S, Shishido K, Tobita K, Hayashi T, Miyashita H, Yokoyama H, et al. Distal Transradial Access For Cardiac Catheterization in Patients Undergoing Hemodialysis. 2022;34.
- Ali S, Abdullah MS, Abdelrahman K, Ali A, Faisal F, Ali A. Total Radial Artery Occlusion Following Transradial Access: Complete Recanalization via the Anatomical Snuffbox. Methodist Debakey Cardiovasc J [Internet]. 2020 Oct 1 [cited 2022 Dec 13];16(4):314–7. Available from: https://journal.houstonmethodist.org/articles/10.14797/mdcj-16-4-314