Delayed hospitalisation for heart failure after transcatheter repair or medical treatment for secondary mitral regurgitation: a landmark analysis of the MITRA-FR trial
Selected in EuroIntervention by A. Beneduce , S. Brugaletta
The present study aimed at investigating a potential reduction of the HF hospitalization rate between 1 and 2 years after inclusion in the MITRA-FR trial.
References
Authors
Guillaume Leurent, Vincent Auffret, Erwan Donal, Hervé Corbineau, Daniel Grinberg, Guillaume Bonnet, Pierre-Yves Leroux, Patrice Guérin, Fabrice Wautot, Thierry Lefèvre, David Messika-Zeitoun, Bernard Iung, Xavier Armoiry, Jean Noël Trochu, Florent Boutitie, Jean-Francois Obadia
Reference
May 25, 2022 | 10.4244/EIJ-D-21-00846
Published
25 May 2022
Link
Read the abstract
Reviewers
Our Comment
Why this study – the rationale/objective?
The MITRA-FR and the COAPT trials were originally designed to assess transcatheter edge-to-edge repair (TEER) efficacy for secondary mitral regurgitation (SMR) compared to guideline-directed medical therapy (GDMT) alone at different follow-up times: 1 year for the MITRA-FR and 2 years for the COAPT trial.
Among several other factors, the shorter follow-up time has been claimed as responsible for the negative results of the MITRA-FR at 1 year. However, at 2 years, the rate of the primary composite endpoint was still similar between TEER and medical therapy (64.2 % vs. 68.6 %, HR 1.01; 95 % CI: 0.77 – 1.34), with only a non-significant trend toward lower hospitalization in the TEER group.
This observation is the leading hypothesis behind the present study, aimed at investigating a potential reduction of the HF hospitalization rate between 1 and 2 years after inclusion in the MITRA-FR trial.
How was it executed - the methodology
A landmark analysis of the MITRA-FR trial was performed to assess the potential delayed benefit of the TEER procedure in patients who did not experience any component of the primary endpoint at 1 year.
- Primary outcome: the annualised cumulative rate of HF hospitalization between 1 and 2 years after inclusion in the trial.
- Secondary outcomes: the composite of all-cause death and HF hospitalisation between 1 and 2 years after inclusion in the trial, and its individual components.
What is the main result?
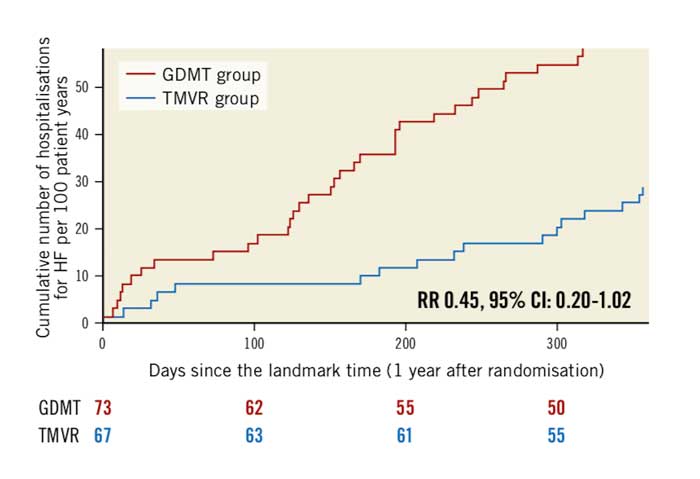
- Out of the 304 patients randomized in the MITRA-FR trial, 140 patients (67 from the TEER group vs. 73 from the GDMT group) did not experience any of the components of the primary endpoint at 1 year, representing the population of this landmark analysis.
- Patients included in this landmark analysis presented more favourable baseline clinical and echocardiographic characteristics than those who died or suffered from HF hospitalization within 1 year from the inclusion in the MITRA-FR trial.
- There was a trend towards lower cumulative HF hospitalization rate in the TEER group (27.6 vs. 60.0 events / 100 patient-year, HR 0.45; 95 % CI: 0.20-1.02; p = 0.057).
- The composite outcome of all-cause death or unplanned HF hospitalization occurred less frequently in the TEER group (20.1 % vs. 32.9 %, HR 0.55, 95 % CI: 0.28- 1.07; p = 0.08), mainly driven by a lower rate of HF hospitalization (16.4 % vs. 30.1 %, HR 0.47, 95 % CI: 0.23-0.97; p = 0.04).
Cumulative rates of recurrent hospitalisations for heart failure in the guideline-directed medical treatment (GDMT) and in the transcatheter mitral valve repair (TMVR) groups between 12 and 24 months after inclusion in the MITRA-FR trial. CI: confidence interval; HF: heart failure; RR: rate ratio
Source: EuroIntervention
Critical reading and the relevance for clinical practice
The present landmark analysis between 1 and 2 years of follow-up of the MITRA- FR study showed a trend towards cumulative HF hospitalization reduction after TEER as compared to GDMT.
However, several methodological aspects of the study deserve consideration. Performing a landmark analysis with an arbitrary timepoint introduces a selection bias towards a subgroup of patients with a favourable clinical profile, potentially hampering the benefits of the original randomized design of the trial.
The original study was not powered for the primary outcome of the current analysis, which was selected in order to allow data cross-comparison with the COAPT trial.
Finally, the lack of a predictive model for event-free survival at 1 year follow-up hampers the insights from this study into clinical practice, as fulfilling the baseline characteristics of the landmark population does not imply a long-term benefit from TEER, leading back to the problem of initial patient selection.
The conflicting results of the MITRA-FR and the COAPT trial highlight the complexity of SMR. Although several attempts have been pursued to reconcile these findings, the reality seems far more complex than what is captured by the two large-scale trials, and might go beyond the proportionate/disproportionate SMR dualism.
Therefore, future studies should aim at reducing this gap in knowledge, exploring the role of unidentified factors in determining clinical outcomes of these patients, such as myocardial fibrosis, contractile reserve, and potential for reverse remodelling.
The surgeon's perspective
I read with great interest this report, awaited since long time. the landmark analysis shows something somehow expected. Also the COAPT sub analysis showed that patients with MITRA-FR like characteristics (larger ventricles less severe MR) had a similar reduction of hospitalisation rate as those with smaller ventricles and more severe MR at baseline.
In addition, the improvement of symptoms and quantitative indexes of quality of life was similar in the two groups.
Obviously, survival is lower in patients with more remodelled ventricles. The current study is methodologically fragile, however is hypothesis generating. Those patients treated too late (too large ventricles) have not survived one year follow-up in either group (Mitraclip and control). After the elimination of the patients in whom the procedure was futile and in those who were too advanced also for the medical therapy, it appears clear that the mechanical treatment of FMR, in association with GDMT, is associated with more stable clinical conditions and protects from rehospitalizations.
Therefore this paper suggests an important message: TEER improves quality of life and prevents decompensation, in association to GDMT, unless the procedure is performed in end-stage patients. TEER is not an alternative to LVADs or to HTx. when offered early enough in patients surviving at least one year after the procedure, it offers protection from Hospitalization and a substantial clinical benefit (although not significative due to the small number of patients at risk.
This message, somehow new for the MITRA-FR like population, should suggest further efforts in improving patient selection, quality of interventions, and synergy with medical therapy. Ad hoc strategy trials should be designed to support a synergistic approach in drug and device therapies for HF.







No comments yet!