Effect of wire jailing at side branch in 1-stent strategy for coronary bifurcation lesions
Selected in JACC: Cardiovascular Interventions by A. Shahin , K. De Silva
This study aimed to determine the effectiveness of jailing a wire in the side branch of a bifurcation lesion to prevent side branch compromise during provisional main vessel stenting when a one-stent in bifurcation PCI technique is adopted.
References
Authors
Yeon-Jik Choi, Seung-Jun Lee, Byeong-Keuk Kim, Sung-Jin Hong, Chul-Min Ahn, Jung-Sun Kim, Hyeon-Cheol Gwon, Hyo-Soo Kim, Woo Jung Chun, Seung-Ho Hur, Chang-Wook Nam, Seung Hwan Han, Seung-Woon Rha, In-Ho Chae, Jin-Ok Jeong, Jung Ho Heo, Junghan Yoon, Do-Sun Lim, Jong-Seon Park, Kwang Soo Cha, Doo-Il Kim, Sang Yeub Lee, Kiyuk Chang, Byung-Hee Hwang, So-Yeon Choi, Myung Ho Jeong, Ki-Hong Choi, Young-Bin Song, Soon-Jun Hong, Joon-Hyung Doh, Bon-Kwon Koo, Myeong-Ki Hong, and Yangsoo Jang
Reference
J Am Coll Cardiol Intv. 2022 Feb, 15 (4) 443–45
Published
15 February 2022
Link
Read the abstract
Reviewers
Our Comment
Why this study – the rationale/objective?
Bifurcation PCI is increasingly undertaken, frequently within complex lesion subsets, with calcification, tortuosity, and unfavorable side-branch angulation being common.
A provisional stenting approach remains the most common single stent strategy for bifurcation lesions, irrespective of the Medina lesion classification.
Trial data and guidelines affirm that a provisional approach portends improved mortality, lower major adverse cardiovascular events (MACE), stent thrombosis (ST), and target lesion failure (TLF), when compared to more complex two-stent bifurcation techniques, although these may be required, depending on individual anatomy and clinical context.
However, one unresolved procedural consideration is whether the routine placement of a wire in the side-branch (SB) of the bifurcation lesion prevents compromise to SB vessel flow, and whether this has any peri-procedural and/or longer-term clinical benefit, compared to when no wire is utilized prophylactically, and a wire is placed in the SB only when there is intra-procedural compromise to flow.
This study aimed to determine the effectiveness of jailing a wire in the SB of a bifurcation lesion to prevent SB compromise during provisional main vessel (MV) stenting when a one-stent in bifurcation PCI technique is adopted.
How was it executed? - the methodology
A retrospective analysis of data from the COBIS (Coronary Bifurcation Stenting) III registry was undertaken.
1,890 patients with bifurcation lesions who underwent the one-stent strategy using second-generation drug-eluting stents were identified and classified into two groups according to the use of SB wire jailing: wire jailing (n = 819) and non–wire jailing (n = 1,071).
The incidence of SB occlusion (Thrombolysis In Myocardial Infarction flow grade <3) and target lesion failure (TLF) (cardiac death, myocardial infarction, or target lesion revascularization) was compared between the two groups during a median follow-up of 52 months.
What is the main result?
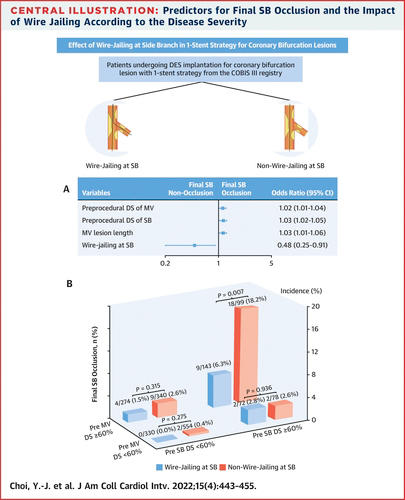
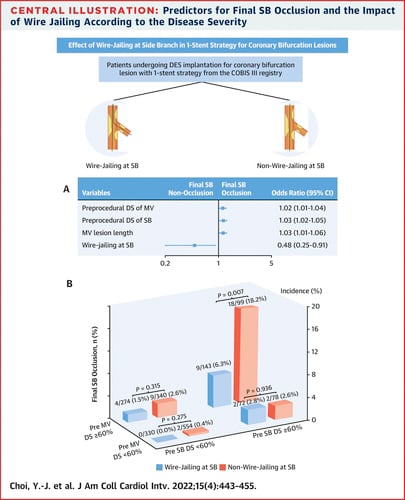
The authors concluded that the overall incidence of final SB occlusion with provisional stenting was not significantly different between wire jailing group vs non–wire jailing group (1.8 vs 2.9 % respectively; p = 0.133) across all-lesion subsets.
The incidence of abrupt SB occlusion during the procedure was found to be similar between both groups (3.5 % vs. 3.7 %, p = 0.257), however restoration of flow was more significantly observed in the wire-jailed group (1.7 % vs. 0.8 %, p = 0.037).
During a median follow-up of 52 months, the incidence of TLF was not significantly different between wire jailing and non–wire jailing (7.6 % vs 6.3 %; p = 0.343). However, multivariate analysis suggested that up-front SB wiring in those with a significant stenosis (DS > 60 %) in the SB (5.1 % vs 11.3 %; OR 0.42; 95 % CI: 0.19-0.89; p = 0.028) or MV (3.1 % vs 6.2 %; OR: 0.49; 95 % CI: 0.24-0.95; p = 0.039) reduced rates of procedural SB vessel occlusion after MV stenting.
There were a number of important anatomic and procedural characteristics that were considered in the analysis. Left main (LM) coronary bifurcation lesions (39.2 % vs 27 %, p < 0.001) and true bifurcations [Medina 1.1.1, 1.0.1, 0.1.1] (47.1 % vs 27.4 %, p < 0.001) were more prevalent in the wire-jailing group.
There was more extensive coronary disease within the wire-jailing group, with higher grade stenosis [(MLD) 1.6 mm ± 0.8 vs 1.8 mm ± 0.8, p < 0.01, DS 41.1% ± 25.6 vs 33.0 %± 24.3, p< 0.01] and longer lesion length (4.7 mm ± 6.0 vs 29.± 5.3 p< 0.001) observed in the SB. The lesion length in the MV was also greater in the jailed-wire group (19.5 mm ± 10.5 vs. 18.3 mm ± 9.7, p=0.008).
The use of IVUS was greater in the wire-jailing group (47.1 % vs 31.8%, p < 0.001).
Moreover, the presence of a jailed wire led to increased adoption of optimisation techniques in both the MV and SB. Within the MV, kissing balloon inflations (KBI) (26.1 % vs 6.1 % p <0.001), proximal optimization technique (POT) (37.1 % vs 24.2 %, p <0.001) and use of non-compliant balloon post-dilatation (19.7 % vs 15.2 %, p= 0.032) were undertaken more systematically in the jailed-wire group.
Similarly, SB interventions such as ballooning without KBI (4.8 % vs 2.5 %, p = 0.024), SB ballooning after MV stenting (30.9 % vs 8.6 %, p <0.001) as well as SB stenting (6.8 % vs 1.3 %, p < 0.001) occurred more frequently in the jailed-wire group.
Finally, there was no difference between the two groups in the degree of angiographic calcification (19.2 % vs 17.4 % vs 7.2 % vs 4.7 % p = 0.350).
The bifurcation angle between both groups was similar (72.2° ± 23.8° vs 71.0° ± 21.2°, p=0.232). Although the presence of thrombus was more frequently observed in the wire-jailing group (MV 2.4 % vs 3.1 % and SB 0.9 % vs 0.1 % p = 0.025).
Source = JACC: Cardiovascular Interventions
Critical reading and the relevance for clinical practice
The authors surmise that up-front placement of a SB wire in the setting of bifurcation PCI with a one-stent provisional approach does not lead to improved procedural or long-term outcomes. They also suggest that the overall occurrence of SB occlusion was not different between the two groups, although restoration of SB flow following abrupt occlusion was significantly higher in the wire jailing group.
This type of pragmatic data is a valuable addition to the literature within the bifurcation PCI space, however, due to the retrospective, observational nature of these data, there are a number of factors to consider in regard to external validity and generalizability to day-to-day interventional practice.
The wire-jailing group consisted of a higher risk population with more LM bifurcations and more extensive coronary disease, with a greater proportion of true (Medina classified) bifurcation lesions. These are all important anatomic and technical markers that would have prompted upfront wiring of the SB compared to the non-wire jailing group, which has led to marked confounding due selection bias within the study. As the two groups are so vastly different, defining the utility of systematic up-front wiring of SB’s is difficult to discern and translate into day-to-day interventional practice based upon these data.
Additionally, true bifurcation lesions, particularly involving the LM, are known to have higher risk of major adverse cardiac events (MACE). The loss of a SB (e.g. Circumflex), either temporarily or permanently, in the setting of a LM bifurcation is more impactful on the size of the periprocedural infarction and overall long-term clinical outcomes. The current data have combined LM and non-LM data when attempting to resolve the quandary of whether up-front wiring is of benefit when undertaken on a systematic basis. However, the LM setting is a unique one, and needs to be considered as such. Therefore, the data presented in this study lack the granularity to define the value of the SB wire when specifically undertaking PCI to LM bifurcations.
The study observed that SB wiring was more frequently undertaken in the presence of high-grade stenosis in the SB vessel which mirrors clinical practice. One key observation was that there was more rapid restoration of flow in those that had a SB wire placed up-front. This reaffirms that, in selected patients, with SB anatomy that may be more susceptible to SB closure during PCI, the use of an up-front wire may allow more efficient access to this branch, either as use as a marker wire for re-wiring, or used for abluminal ballooning behind the MV stent, which may prevent or reduce prolonged intra-procedural ischaemia and infarction.
Additionally, the degree of peri-procedural infarction between the two groups is not included in these data, but would be helpful to further define whether having access to a SB and potentially minimizing procedural ischaemia leads to a reduction in peri-procedural infarction, when undertaken on a routine basis.
In conclusion, this study suggests that systematic up-front wiring of a SB in a bifurcation is unlikely to reduce SB closure and TLF. However, there are important caveats to this, with a signal that suggests in the presence of a high-grade SB stenosis (> 60 %), wire placement may allow easier access and more brisk restoration of SB flow if reduced following main vessel stenting.
Moreover, due to the retrospective, observational nature of this dataset, there is marked selection bias which limits the generalisability of these data to different lesion subsets, specifically to left main bifurcations.
Further randomized trial investigation, particularly within left main anatomy, would be valuable to further define and elucidate the potential value of having a second wire in situ when undertaking a bifurcation PCI when the clinical jeopardy is high.
References:
- Burzotta F, Lassen JF, Lefèvre T, et al. Percutaneous coronary intervention for bifurcation coronary lesions: the 15th consensus document from the European Bifurcation Club. EuroIntervention J Eur Collab with Work Gr Interv Cardiol Eur Soc Cardiol. 2021;16(16):1307.
- Choi KH, Song Y Bin, Lee JM, et al. Prognostic effects of treatment strategies for left main versus non-left main bifurcation percutaneous coronary intervention with current-generation drug-eluting stent. Circ Cardiovasc Interv. 2020;13(2):e008543. doi:10.1161/CIRCINTERVENTIONS.119.008543
- Hahn J-Y, Chun WJ, Kim J-H, et al. Predictors and outcomes of side branch occlusion after main vessel stenting in coronary bifurcation lesions: results from the COBIS II Registry (COronary BIfurcation Stenting). J Am Coll Cardiol. 2013;62(18):1654-1659.








No comments yet!