Radial versus femoral access in ACS patients undergoing complex PCI is associated with consistent bleeding benefit and no excess of risk
Selected in Canadian Journal of Cardiology by A. Cader , A. N. Calik
In this paper, the authors investigated the comparative efficacy and safety of TRA versus TFA in ACS patients undergoing complex PCI in the Minimizing Adverse Haemorrhagic Events by TRansradial Access Site and Systemic Implementation of angioX (MATRIX)-Access trial1.
References
Authors
Antonio Landi, Mattia Branca, Pascal Vranckx, Sergio Leonardi, Enrico Frigoli, Dik Heg, Paolo Calabro, Giovanni Esposito, Gennaro Sardella, Carlo Tumscitz, Stefano Garducci, Giuseppe Ando, Ugo Limbruno, Paolo Sganzerla, Andrea Santarelli, Carlo Briguori, Jose M. de la Torre Hernandez, Giovanni Pedrazzini, Stephan Windecker, Marco Valgimigli, for theMATRIX Investigators.
Reference
10.1016/j.cjca.2022.06.014
Published
23 June 2022
Link
Read the abstract
Reviewers
Our Comment
Society guidelines recommend transradial access (TRA) as the default approach for the invasive management of acute coronary syndrome (ACS). However, the comparative effectiveness of TRA over transfemoral access (TFA) in ACS patients undergoing complex percutaneous coronary intervention (PCI) remains unclear.
Why this study – the rationale/objective?
Society guidelines recommend transradial access (TRA) as the default approach for the invasive management of acute coronary syndrome (ACS). However, the comparative effectiveness of TRA over transfemoral access (TFA) in ACS patients undergoing complex percutaneous coronary intervention (PCI) remains unclear.
Complex PCI patients incur higher risks of ischemic and bleeding complications due to the use of large bore catheters and the presence of more comorbidities.
In this paper, the authors investigated the comparative efficacy and safety of TRA versus TFA in ACS patients undergoing complex PCI in the Minimizing Adverse Haemorrhagic Events by TRansradial Access Site and Systemic Implementation of angioX (MATRIX)-Access trial1.
How was it executed? - the methodology
This is a post-hoc analysis of the MATRIX trial, a program of 3 independent randomized controlled trials in ACS patients undergoing invasive management. This analysis was undertaken in participants enrolled in the MATRIX-Access trial.
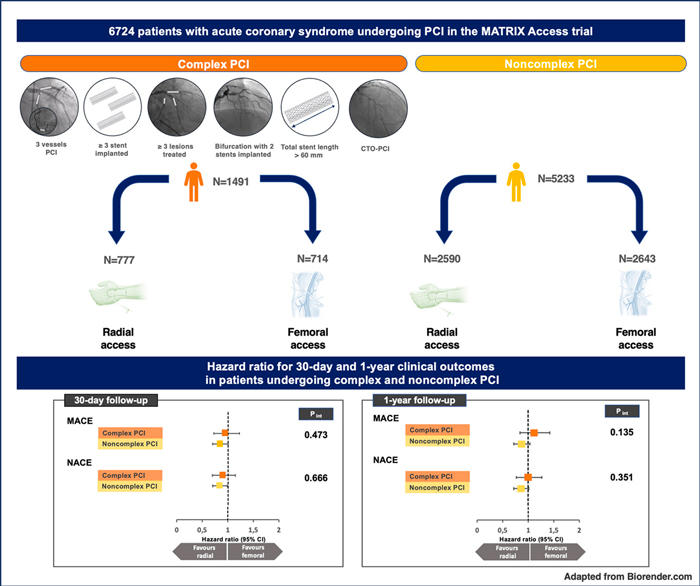
Complex PCI was defined as PCI with at least one of the following characteristics: three-vessels PCI, ≥ 3 implanted stents, ≥ 3 treated lesions, 2-stent bifurcation PCI, total stent length > 60 mm or chronic total occlusion (CTO)-PCI2. Patients without these criteria were classified as noncomplex PCI.
The two co-primary outcomes were:
- Major adverse cardiac events (MACE): the composite of all-cause mortality, myocardial infarction (MI), or stroke
- Net adverse clinical events (NACE): the composite of MACE or major bleeding not related to coronary artery bypass grafting at 30-days.
Secondary outcomes included the composite of all-cause mortality, MI, stroke, urgent target vessel revascularization (TVR), or definite stent thrombosis, each component of the co-primary outcomes and cardiovascular mortality. The key secondary outcome was access site-related BARC type 3 or 5 bleeding at 30 days.
All analyses were performed by the intention-to-treat principle.
What is the main result?
Among 8,404 patients enrolled in the MATRIX-Access trial, 6,724 patients underwent PCI.
Of those, 1,491 (22.2 %) patients underwent complex PCI and 5,233 (77.8 %) underwent noncomplex PCI.
In the complex PCI group, 777 underwent TRA and 714 subjects TFA.
In the non-complex PCI group, 2,590 and 2,643 patients underwent TRA and TFA, respectively.
Patients undergoing complex PCI were older and more frequently had diabetes, previous MI, peripheral artery disease, and NSTE-ACS. They also had more frequent left coronary lesions (particularly the left main), longer fluoroscopy, and procedural times than the non-complex PCI group.
In both complex and non-complex PCI groups, those allocated to TRA had a more significant crossover to TFA. 6 Fr was the most used sheath size in both access sites. The prevalence of complex PCI features was well balanced between TRA and TFA.
Overall, complex PCI was associated with a higher risk of 30-day MACE (HR: 1.56; 95 % CI:1.33 to 1.82; P < 0.001) and NACE (HR: 1.54, 95 % CI: 1.32 to 1.79; p < 0.001), driven by an increased risk of all-cause mortality and MI.
As for access, in the complex PCI group, there were no significant differences in the rates of 30-day MACE (14.4 % vs 15.3 %; hazard ratio [HR]: 0.94; 95 % [CI]:0.72-1.22; p=0.643) or NACE (15.6 % vs 17.4 %; HR: 0.89; 9 5% CI: 0.69-1.14; p = 0.349) between TRA vs TFA.
In the non-complex PCI group, both 30-day MACE (8.8 % vs 10.5 %; HR: 0.84; 95 % CI: 0.70-1.00; p = 0.046) and NACE (9.9 % vs 11.9 %; HR: 0.83; 95 % CI: 0.70-0.98; p = 0.028) were lower with TRA, as compared to TFA. However there were no significant interactions for the treatment effects on co-primary outcomes between complex and non-complex PCI groups (Pint 0.473 and 0.666, for MACE and NACE respectively).
There were also no significant differences in co-primary endpoints between TFA and TRA for both complex and non-complex PCI at 1 year.
BARC type 3 or 5 bleeding was significantly lower with TRA in complex PCI patients (HR: 0.42; 95 % CI: 0.22 to 0.81; p = 0.01) and numerically lower in noncomplex PCI patient (HR: 0.72; 95 % CI: 0.49-1.06; p = 0.097).
Access-site BARC type 3 or 5 bleeding was lower with TRA, both among complex (HR: 0.18; 95 % CI: 0.05-0.63) and noncomplex (HR: 0.41; 95 % CI: 0.20-0.85) PCI patients. However, the complex PCI patients had a greater absolute risk reduction of 1.7 % (number needed to treat: 59) due to their higher absolute risk.
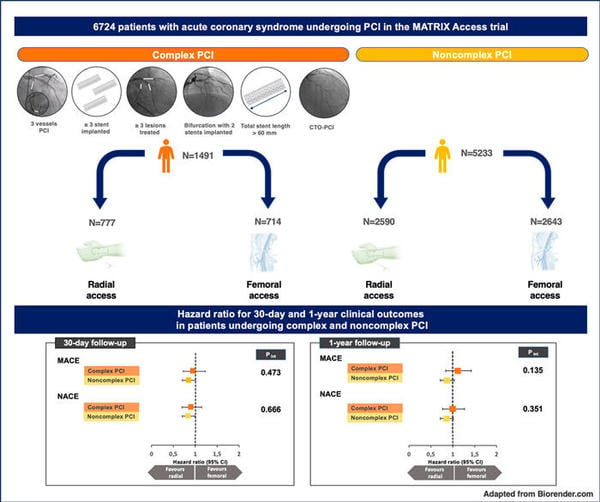
30-day and 1-year MACE and NACE following radial versus femoral access in ACS patients undergoing complex PCI.
Source: Canadian Journal of Cardiology
Critical reading and the relevance for clinical practice
There is increasing focus on access site in coronary revascularisation, especially as a means of reducing bleeding. In this large post-hoc analysis of MATRIX-Access specifically looking at the impact of access site in complex PCI patients (who are prone to higher risk of ischaemic events post-PCI), the main takeaway is that the complexity of PCI did not affect the comparative efficacy and safety of TRA versus TFA, which is supported by negative interaction testing for the co-primary (MACE and NACE) or major secondary endpoints.
While NACE, MACE, and mortality were lower with TRA among non-complex PCI patients, these outcomes showed no significant differences in patients who had undergone complex PCI. Despite numerically favouring TRA for both co-primary endpoints at 30 days, in the complex PCI group, a slight numerically higher rate of MACE did not favour TRA at one year and mortality at both 30 days and one year.
Importantly, though, TRA significantly reduced access-site-related BARC 3 or 5 bleeding across board, but with a more significant absolute and relative risk-benefit in the complex PCI group. Another interesting observation, albeit arising from subgroup analyses, is the numerical excess of mortality and higher fatal events (HR: 1.52; 95 % CI : 0.92 to 2.45) in TRA when a 6 French guide was used, but not among those who received > 6-French access sheath size. Also, there was a 3-fold less frequent use of large-bore access in TRA compared with TFA among complex PCI patients.
Limitations: these results must be interpreted in the background that this was a post-hoc analysis of MATRIX-Access, which was not powered to explore differences in outcomes across subgroups, and where randomization was not stratified by PCI complexity. Furthermore, a high level of operator expertise required for eligibility in MATRIX might limit the generalisability of outcomes results.
Also, the definition used for complex PCI2 has been validated in patients with chronic coronary syndromes (CCS), but not ACS, and some very complex subsets of coronary lesions (e.g. CTOs, calcified lesions, and graft interventions) may have been under-represented during enrolment in this study.
Furthermore, one needs to consider nuances related to each access and their volumes by centre, as well as operator expertise and de-skilling (in TFA). As also noted in the original MATRIX publication, events in both TRA and TFA arms were higher in centres with higher proportions of radial procedures3, and higher rates of NACE were seen in the TFA arm, among those attending centres using predominantly TRA as compared to those using predominantly TFA. The results of this analysis must therefore also be interpreted on this background.
References
- Landi A, Branca M, Vranckx P, et al; MATRIX Investigators. Radial versus femoral access in ACS patients undergoing complex PCI is associated with consistent bleeding benefit and no excess of risks. Can J Cardiol. 2022 3:S0828-282X(22)00394-4.
- Giustino G., Chieffo A., Palmerini T., et al. Efficacy and Safety of Dual Antiplatelet Therapy After Complex PCI. J Am Coll Cardiol 2016;68(17):1851–1864.
- Valgimigli M, Frigoli E, Leonardi S, et al; MATRIX Investigators. Radial versus femoral access and bivalirudin versus unfractionated heparin in invasively managed patients with acute coronary syndrome (MATRIX): final 1-year results of a multicentre, randomised controlled trial. Lancet. 2018;392(10150):835-848.






No comments yet!