Treatment of coronary bifurcation lesions, part II: implanting two stents. The 16th expert consensus document of the European Bifurcation Club
Selected in EuroIntervention Journal by M. Alasnag
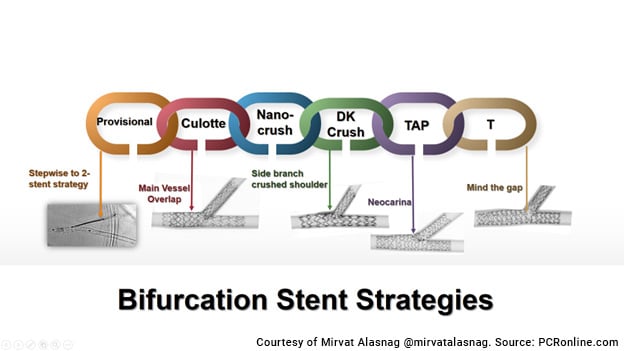
Although the default strategy remains a stepwise provisional strategy, the authors of the 16th expert consensus document recognize that up to 25 % of all single stent approaches eventually require a second.
References
Authors
Jens Flensted Lassen, Remo Albiero, Thomas W Johnson, Francesco Burzotta, Thierry Lefèvre, Tinen L Iles, Manuel Pan, Adrian P Banning, Yiannis S Chatzizisis, Miroslaw Ferenc, Vladimir Dzavik, Dejan Milasinovic, Olivier Darremont, David Hildick-Smith, Yves Louvard, Goran Stankovic
Reference
2022 May 15;EIJ-D-22-00166. doi: 10.4244/EIJ-D-22-00166. Online ahead of print.
Published
15 May 2022
Link
Read the abstractReviewer
My Comment
Historically, European Bifurcation Club (EBC) consensus documents have offered comprehensive overviews of percutaneous coronary bifurcation treatment strategies and have laid the foundation for a step-by-step approach to bifurcation PCI that is grounded in the idea to replicate the underlying bifurcation anatomy.
Such a systematic approach, while ensuring progress in understanding how to adapt different stenting strategies to the realities of bifurcation anatomy, has also resulted in a cumulative experience of potential pitfalls at each step along the way.
The 16th EBC consensus document is a precedent among other EBC consensus documents inasmuch as it, for the first time, provides an extensive list of pitfalls, solutions, and prevention strategies for each step of bifurcation PCI.
Part I of the document concentrates on implantation and optimization of the 1st stent, which is how a great majority of bifurcation PCI procedures are completed. Part II focuses on different techniques of the 2nd stent implantation when necessary and their respective optimization steps.
The 16th expert consensus document of the European Bifurcation Club (EBC) was a very technical review by the experts in the field highlighting the potential pitfalls of the different bifurcation strategies elaborated in the previously published EBC statements.
Although the default strategy remains a stepwise provisional strategy, authors recognize that up to 25 % of all single stent approaches eventually require a second. The subsequent 2-stent technique depends on significance of the side branch (SB), residual disease in the SB, and access & angle to the SB, which are all largely predetermined by the implantation of the initial single stent in the main vessel (MV).
- If the SB ostial scaffolding is optimal & the angle is wide with a clearly visible ostium, T-stenting may be attempted; otherwise, a TAP technique permitting minimal protrusion to avoid a geographic miss is recommended.
- Culotte or double kissing (DK)-culotte are an alternative depending on the operator's experience, size of the SB, and angle.
- An inverted DK-culotte, DK-crush & inverted T-stenting, and TAP are generally reserved for an upfront 2-stent strategy.
Nevertheless, these techniques are complex, and several pitfalls have been identified, and mechanisms to correct them have been described in the latest EBC document:
T/TAP-stenting:
Imprecise positioning with too distal or proximal implantation may require correction depending on the extent of the gap/protrusion.
Correction:
- Too distal: Further post dilatation to optimize scaffolding or placement of another stent
- Too proximal: conversion to mini-culotte or an internal crush
TAP stenting
Neocarina is the source of most pitfalls in this technique.
Correction:
- Shift or damage during kissing balloon inflation (KBI) or proximal optimization (POT) can be corrected by repeat KBI with simultaneous balloon deflation to reposition the neocarina centrally within the point of confluence.
- Restenosis following intimal hyperplasia & endothelialization of the neocarina can be treated with sequential kissing inflations to recenter the carina.
DK Culotte
Proximal rewiring and distal rePOT may preclude delivery of a second stent into the SB.
Correction:
- Distal rewiring, that may require the use of a microcatheter and confirmation with intracoronary imaging.
- Delivery of balloons after implantation of the second stent may be due to entangled wires which requires requiring with minimal torque, proximal strut rewiring which requires a third wire crossing into the SB closer to the carina, and/or use of an anchoring balloon, and finally the use of an undersized balloon for simply requires re-POT with an appropriately sized & accurately positioned non-compliant balloon at the shoulder proximal to the carina.
DK Crush
Several pitfalls are identified in this complex technique. Often one pitfall leads to several others in a domino effect.
For example, rewiring the SB through a “distal” stent cell before the KBI can result in an abluminal wire passage underneath the malapposed/crushed SB’s distal margin which ultimately can result in an uncorrectable gap at the distal SB margin or malapposition on the contralateral wall.
Correction:
- Proximal cell wiring before the KBI, SB ostial optimisation (Step 2) with high-pressure balloon inflation before the stent is crushed and POT of the MV stent facilitates the SB requiring and avoids abluminal wire passage.
- Simultaneous balloon deflation minimises the risk of double-layer metallic neocarina deviation which can occur if the deflation was not simultaneous or the re-POT was too distal.
- SB balloon crossing can be challengingand can be overcome by using an ultra-low profile balloon (diameter ≤1.5 mm), dilating the stent struts of the SB ostium, increasing the support by coaxial catheter alignment or use of guide catheter extensions, exchanging the wire for an extra-support guidewire using a microcatheter, or rewiring in the case of tangled wires or through a different cell.
Conclusion
What is also addressed very elegantly in this document is how to prevent complications and pitfalls. The authors recommend extensive education of operators, using modeling and further training.
It is imperative that operators grasp the finer details of 2-stent techniques before embarking on them, since they have a direct impact on outcomes such as immediate procedural success and target vessel revascularization.
They also discuss the role of enhanced x-ray imaging and intracoronary imaging to improve the visibility and permit execution of each step methodically.
Questions to the lead author
Jens Flensted Lassen agreed to answer Mirvat Alasnag's questions to go even further!
TAP is considered the least complex of the 2-stent strategies. However, errors in positioning the SB stent can occur & impact the metal carina. If the SB stent protrudes too much into the MV, how would you correct it?
If the side branch stent protrudes too much into the MV the easiest way to correct it and reach an acceptable result is to rewire distal through the metal carina and change the TAP to a Culotte and finalise with kissing and POT. If the long metal carina is left as it is it is of paramount importance not to POT to deep, because this will cause crushing of the metal carina towards the sidebranch.
The DK crush, on the other hand, appears to be one of the most complex. In particular, some struggle with recrossing into the crushed SB. How do you recommend we facilitate the recrossing?
I strongly recommend to introduce a POT after crushing the SB stent, (and maybe more than one POT) to make sure the stent is properly crushed and respect the anatomy, that will ease the access towards the SB and facilitate the first kissing. Then a new,POT after implantation the MB stent (before rewiring, and second kissing).
Most investigators in the landmark trials had extensive experience in bifurcation stenting. How do you recommend operators achieve the necessary level of expertise to perform these complex PCIs independently?
Recently simulators in bifurcation stenting have been increasingly available and makes it very close to the clinical setting to perform the simulated procedures. One way forward could be this type of “dry training” not only for fellows but also for trained professional for continuously training of their skills.
Twitter discussion
#EIJonAir 12 - The 16th EBC consensus document https://t.co/h2hxBpp3Ki
— EuroIntervention (@EuroInterventio) June 21, 2022






No comments yet!