09 Mar 2023
Outcomes of medical therapy plus PCI for multivessel or left main CAD ineligible for surgery
Selected in JACC: Cardiovascular Interventions by M. Alasnag , P. M. Swamy
The OPTIMUM study evaluates the outcomes in patients with complex CAD, including significant LM disease, its equivalent, or MVD CAD, undergoing percutaneous revascularization in addition to guideline directed medical therapy (GDMT) versus GDMT alone.
References
Authors
Adam C. Salisbury, J. Aaron Grantham, W. Morris Brown, William L. Ballard, Keith B. Allen, Ajay J. Kirtane, Michael Argenziano, Robert W. Yeh, Kamal Khabbaz, John Lasala, Puja Kachroo, Dimitri Karmpaliotis, Jeffrey Moses, William L. Lombardi, Karen Nugent, Ziad Ali, Kensey L. Gosch, John A. Spertus, David E. Kandzari, and on behalf of the OPTIMUM Investigators
Reference
J Am Coll Cardiol Intv. 2023 Feb, 16 (3) 261–273
Published
13 February 2023
Link
Read the abstract
Reviewers
Our Comment
Why this study – the rationale/objective?
The 2021 ACC/AHA/SCAI joint committee practice guidelines support a heart team approach for the management of patients with complex coronary artery disease (CAD) including significant left main disease, its equivalent, or multivessel CAD1.
The SYNTAX score usually preordains the revascularization strategy for optimal and durable long-term outcomes in these patients. However, these patients may not have isolated coronary artery disease and have other comorbidities that deem them at a prohibitive risk for coronary artery bypass grafting (CABG) and are referred for ‘high risk’ percutaneous coronary intervention (PCI). These patients are also known to have high risk for post PCI mortality1,2.
There is paucity of literature investigating the outcomes of these patients. The OPTIMUM study was a step forward evaluating the outcomes in this growing subset undergoing various treatment strategies, namely percutaneous revascularization in addition to guideline directed medical therapy (GDMT) versus GDMT alone.
How was it executed? - the methodology
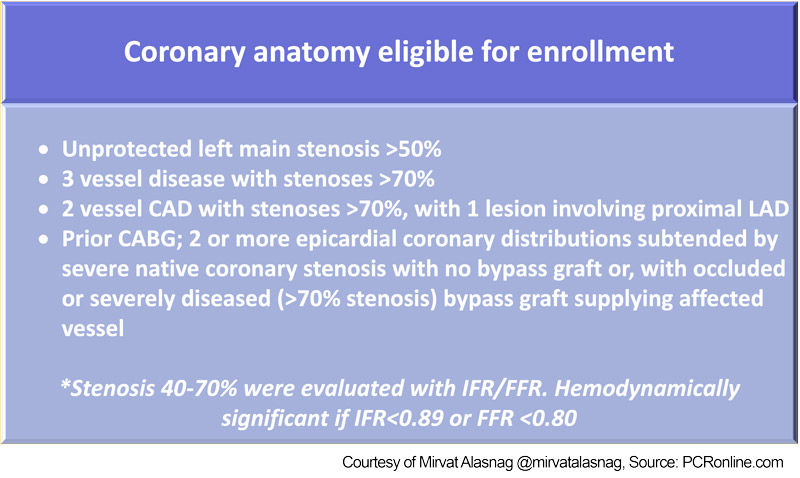
Between December 2016 and July 2019, 726 patients from 22 centers with complex multivessel or obstructive left main coronary artery disease (Table 1) deemed to have prohibitive risk for CABG, after a heart team discussion, were enrolled into a registry. Patients with ST elevation myocardial infarction (STEMI), cardiogenic shock/hemodynamic instability or electrical instability were excluded from this study.
Table 1: coronary anatomy eligible for enrollment, Source: PCRonline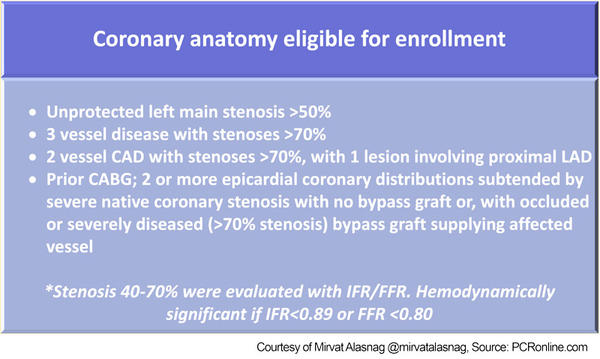
The initial design had patients treated with guideline directed medical therapy alone and those treated with GDMT and PCI. This was then modified to focus only on GDMT + PCI due to the limited enrollment of patients treated with medical therapy alone.
Individual predicted risk assessment for surgical mortality was performed using Society of Thoracic Surgeon (STS) and European System for Cardiac Operative Risk Evaluation II (EuroScore II) models, in hospital, and 30 day mortality of PCI was calculated using current National Cardiovascular Data Registry (NCDR) cath PCI risk model, and integer risk score with corresponding mortality rate was calculated utilizing a bedside risk prediction tool. This was then compared with observed mortality during the index hospitalization, 1 month and 6 months. Observed to expected ratios were then calculated.
Both the Seattle Angina Questionnaire (SAQ) and Kansas City Cardiomyopathy questionnaire (KCCQ) were administered at baseline, at 1 month and 6 month follow-up. The improvement in clinical symptomatology was further quantified as clinically important and moderate to large improvement.
What is the main result?
726 patients treated with PCI + GDMT were enrolled in this study of whom 83.2 % underwent a single PCI and the remaining 16.8 % had staged PCI procedures. The primary indication for revascularization
was ischemic symptoms (39.8 %), acute coronary syndrome (27.1 %) and ischemic cardiomyopathy (24.1 %).
- Completeness of revascularization was assessed with calculating baseline and post revascularization / PCI residual SYNTAX score. Of the enrolled patients, 682 (93.9 % of enrolled) had a baseline calculated SYNTAX score, 45.3 % had SYNTAX score of > 33, with baseline score of 32.4 +/- 12.2 points. Post PCI SYNTAX was calculated in 674 patients. A residual score of low SYNTAX score (< 22) was noted in 75.7 % patients with 34.3 % achieve < 8 residual SYNTAX score, 15 % had residual intermediate SYNTAX score (23-32) and 9 % had residual high SYNTAX score (>/ = 33). Residual SYNTAX score of < 8 to higher residual scores did not have statistically significant difference in clinical outcomes in terms of in hospital mortality and mortality at 30 days (3.9 % vs 6.3 % ; p = 0.19) and at 6 months (10.8 % vs 12.2 % ;p = 0.60). Symptomatically, based on SAQ and KCCQ, patient with lower residual score < 8 did not notice significant difference in symptoms compared to higher residual score. Therefore, completeness of revascularization did not have significant bearing on mortality or with significant change in symptomatology and health status at 6 months.
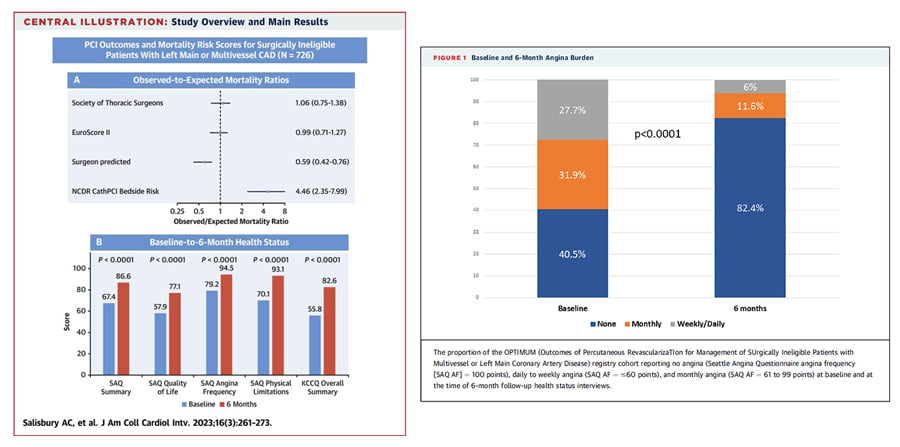
- A 30 day or in hospital mortality was noted in 41 patient (5.6 %) and in 89 (12.3 %) at 6 months. Expected mortality was estimated accurately with surgical risk prediction models – STS and EuroScore II, observed to expected mortality ratio was 1.06 (0.75- 1.38) with STS score and 0.99 (0.71-1.27) with EuroScore II. Surgeons upon their bedside prediction of mortality, observably overestimated the risk with an observed to estimated mortality ratio of 0.59 (0.42-0.76). Contrastingly, NCDR cath PCI risk prediction model undermined the potential risk of mortality with an observed to predicted mortality of 4.46 (2.35-7.99). The most common procedural complications were coronary perforation in 36 (5.0 %), access site hematoma in 36 (5 %) and non access site bleeding in 31 (4.3 %), and incidence of all other procedural complications was < 2 %.
- Health status outcomes could be assessed through 6 months in 501 patients (78.6 %). Patients who were lost to follow up (4.2 %), unable to complete questionnaire (4.1 %), refused to complete assessment (13 %) and those who had mortality within 6 months were excluded. At 6 months, a significant improvement in SAQ angina frequency (mean improvement by 10 points; 6.7 +/- 17 points p < 0.0001), SAQ quality of life (mean improvement by 20 points; p < 0.0001) and KCCQ (mean > 30 points; p < 0.0001). Patients with more frequent reported angina symptoms at baseline benefitted most with ‘moderate to large’ reduction in symptoms at 6 months follow-up. While those without angina or minimal angina had moderate to large improvement in their health status based on KCCQ at 6 months.
Figure 2: OPTIMUM study main results, Source: JACC: Cardiovascular Interventions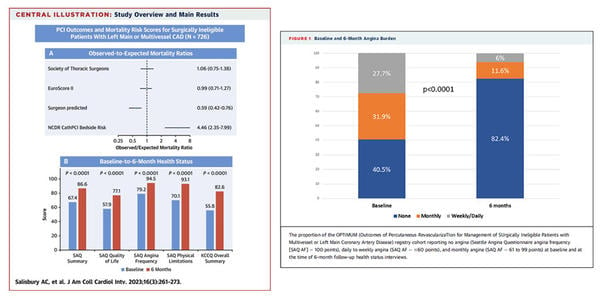
Critical reading and the relevance for clinical practice
- OPTIMUM, although was a prospective registry, paves way for randomized studies in the assessment of risk and outcomes in patients with complex coronary anatomy with high SYNTAX score (> 33) and lifestyle limiting symptoms.
- This study also highlights the importance of GDMT in addition to PCI in this cohort, however it is unknown whether there was an association between optimal GDMT with improvement in SAQ SS and KCCQ scores, especially when there was modest reduction in the post PCI SYNTAX score. Furthermore, optimal medical therapy doses are often unattainable in those with advanced heart failure. The extent of the maximally tolerated doses on outcomes can be determined. Often other co-morbidities limit the achieved doses and hence impact outcomes.
- Completeness of revascularization (SYNTAX < 8 vs > 8) perhaps had a role in mortality in these patients as observed in prior studies3,4. The extent of this impact remains to be determined.
- STS and EuroScore II were revalidated in estimating risk of mortality in this subset of patients. NCDR cath PCI risk prediction model undermined the risk of 30 day mortality in these patient and therefore may not be a relevant tool in risk assessment. Furthermore, future studies to re-evaluate the variables of the NCDR cath PCI risk model and their impact on risk assessment are necessary.
- Finally, the impact of individual co-morbidities as independent drivers of outcomes is yet to be determined.
References
- 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Jennifer S. Lawton, Jacqueline E. Tamis-Holland, Sripal Bangalore, Eric R. Bates, Theresa M. Beckie, James M. Bischoff, John A. Bittl, Mauricio G. Cohen, J. Michael DiMaio, Creighton W. Don, Stephen E. Fremes, Mario F. Gaudino, Zachary D. Gol. 2, s.l.: JACC, 2022 Jan, Vol. 79.
- Treatment of Higher-Risk Patients With an Indication for Revascularization: Evolution Within the Field of Contemporary Percutaneous Coronary Intervention. Ajay J Kirtane, Darshan Doshi, Martin B Leon, John M Lasala, E Magnus Ohman, William W O'Neill, Adhir Shroff, Mauricio G Cohen, Igor F Palacios, Nirat Beohar, Nir Uriel, Navin K Kapur, Dimitri Karmpaliotis. 134, s.l.: Circulation, 2016. 422-431.
- Outcomes With Complete Versus Incomplete Revascularization in Patients With Multivessel Coronary Disease Undergoing Percutaneous Coronary Intervention With Everolimus Eluting Stents. Sripal Bangalore, Yu Guo, Zaza Samadashvili, Edward L. Hannan. 3, s.l.: The American Journal of Cardiology, Feb 2020, Vol. 125.
- Characteristics and outcomes of surgically ineligible patients with multivessel disease treated with percutaneous coronary intervention. Mary C. Shields MD, Michelle Ouellette MD, Nicholas Kiefer MD, Luke Kohan MD, Angela M. Taylor MD, Gorav Ailawadi MD, Michael Ragosta MD. 7, s.l. : Catheterization and Cardiovascular Interventions, 2021, Vol. 98. 1223-1229.