Atrial functional tricuspid regurgitation: Importance of atrial fibrillation and right atrial remodeling and prognostic significance
Selected in JACC: Cardiovascular Imaging by E. Zancanaro
- When tricuspid regurgitation “begets” tricuspid regurgitation -
References
Authors
Soongu Kwak, Jaehyun Lim, Seokhun Yang, Tae-Min Rhee, You-Jung Choi, Hyun-Jung Lee, In-Chang Hwang, Heesun Lee, Yeonyee E. Yoon, Hyo Eun Park, Seung-Pyo Lee, Hyung-Kwan Kim, Su-Yeon Choi, Yong-Jin Kim, Goo-Yeong Cho, Jun-Bean Park
Reference
JACC: Cardiovascular Imaging, Volume 16, Issue 5, 2023
Published
May 2023
Link
Read the abstract
Reviewer
My Comment
Why this study? – the rationale/objective
Tricuspid regurgitation (TR) affects up to 80% of the general population, and significant TR, defined as at least moderate TR, confers a poor prognosis. Secondary or functional TR is caused by the geometric deformation of the tricuspid annulus, usually attributed to the right ventricular (RV) remodeling, and constitutes the predominant mechanism, whereas primary (organic) TR is relatively infrequent. Notably, an emerging population with atrial functional tricuspid regurgitation (AFTR) develops significant TR mainly related to right atrium (RA) remodeling without pulmonary hypertension or left-sided heart disease.
Atrial fibrillation (AF) is highly prevalent in patients with AFTR and is considered a major contributor to its development. However, it remains unclear whether AF causes AFTR or, conversely, whether AF is triggered by significant TR.
The tricuspid annular area was more highly correlated with RA size than with RV size in AF-related AFTR, highlighting the important role of RA remodeling.
The present study aimed to identify the role of AF in the TR development into AFTR without other causes and the principal predictors for significant AFTR. Finally, it aimed to show the outcomes for AFTR progression.1,2,3
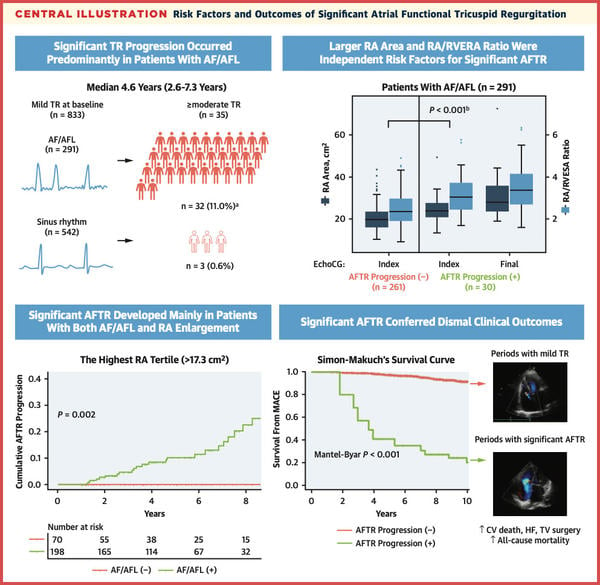
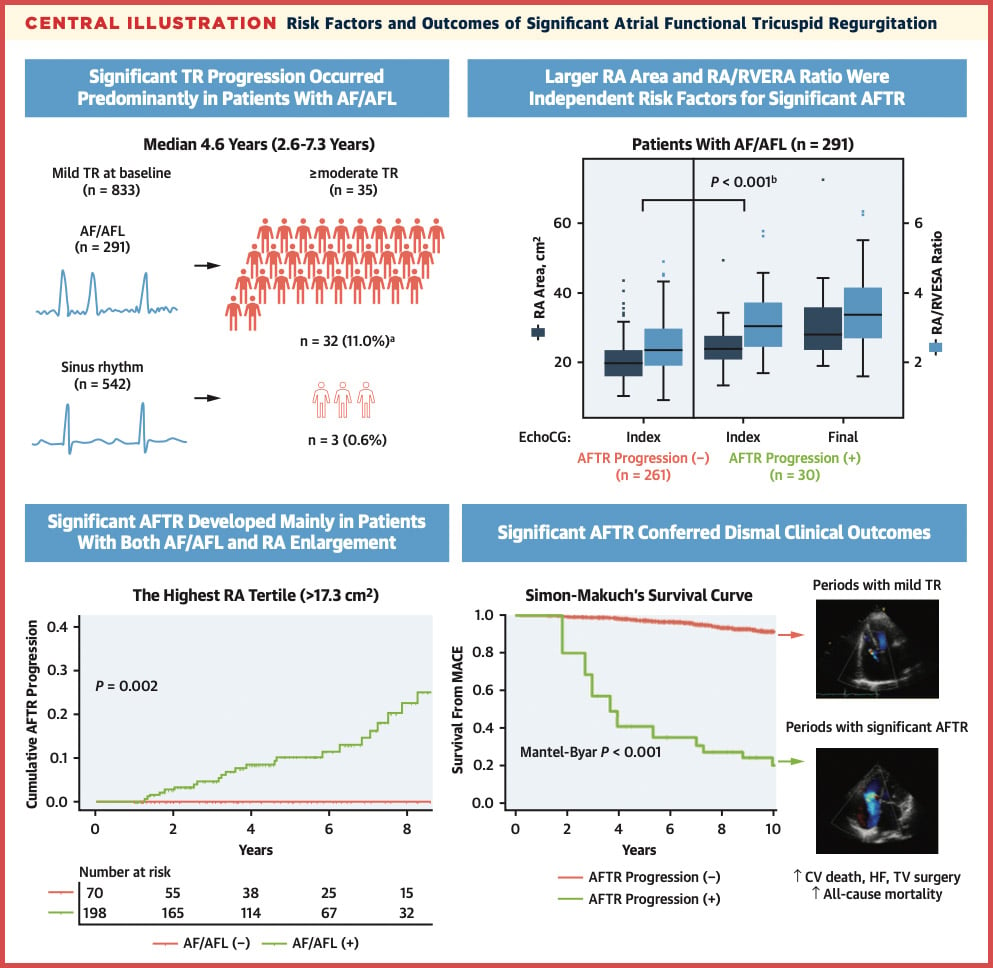
Central illustration
Source: JACC: Cardiovascular Imaging
How was it executed? - the methodology
The present study is a retrospective analysis of patients enrolled between 2007 and 2019 with mild TR. Patients were eligible based on the availability of 1-year TTE in the absence of confounding factor as CIED presence, Left side EF<50%, etc.
Study Endpoint
- The primary outcome was progression to significant TR, defined as moderate or greater TR on the final echocardiography. The outcome was compared among patients with and without AF-AFL
- The risks of major adverse cardiovascular events (MACEs) and all-cause mortality were compared ac- cording to the significant progression of AFTR. MACE was defined as a composite of cardiovascular death, heart failure, and surgery for TR.
What is the main result?
Of 833 patients with mild TR, (34.9%) had AF-AFL. Tricuspid annular diameters measured at end-diastole and end-systole and vena contracta width were higher in patients with AF-AFL (all P < 0.001).
During the 4.6 years, 35 patients developed significant TR (29 moderate and 6 severe). Of these cases, new-onset severe mitral regurgitation was identified in 2 patients, and 33 were identified as having AFTR. The progression rate of AFTR was significantly higher in patients with AF-AFL than in those without (P < 0.001).
AF-AFL was associated with a markedly higher risk of development of significant AFTR in all patients (P < 0.001). The increased age left atrium dimension, area and volume, RA area and volume, RA-RV end-systolic area ratio, tricuspid annular diameters, and vena contracta width were also significant risk factors for the progression of AFTR.
10-year cumulative MACE-free survival was significantly lower after the progression of AFTR (20.2%) than before or without the progression of AFTR (P < 0.001). All-cause mortality was also significantly higher after the progression of AFTR than before or without the progression of AFTR.
The development of significant AFTR predominantly occurred in patients with the highest tertile of RA area. Also, in patients with AF-AFL, RA enlargement was a significant risk factor for the progression of AFTR.
Critical reading and the relevance for clinical practice
The results of this study demonstrated that 4% of patients with mild TR developed significant progression of TR during 4.6 years of follow-up and the progression occurred in patients with AF-AFL. The development of significant AFTR predominantly occurred in patients with the highest tertile of RA area. Also, in patients with AF-AFL, RA enlargement, especially with a higher RA-RV end-systolic area ratio, was a significant risk factor for the progression of AFTR. Patients who developed significant AFTR exhibited markedly higher MACEs and deaths than those who did not.4
Three considerations have to be made:
- Very few previous studies4,5 have shown the impact of AF on TR progression in terms of risk factors. This can be seen also in some confounding factors like previous left-side valve surgery or intervention. The positive impact of the present study has been the patient selection as aforementioned.
- RA enlargement develops earlier (before RV) and this seems to characterize AF in the case of AFTR. This study underlined that RA was bigger in AF patients that developed later AFTR. Also, with the increase of TR, the RA area further develops its enlargement. This creates a severe vicious cycle in which TR progress further and all the RA and RV dimension continue to dilate.
- Several studies have shown a worse outcome in case of intervention in case of not severe AFTR6. This study showed that there is a negative progression of moderate TR in the context of AFTR and this reflects negatively also on clinical outcomes. More attention has to be posed to the right TEE/TTE analysis to better characterize the moderate/mild TR.
In conclusion:
In patients with mild TR, significant AFTR developed predominantly in those with AF-AFL. RA enlargement was a strong risk factor for the progression of AFTR in the presence of AF-AFL. Development of significant AFTR conferred poor cardiovascular outcomes. Closer echocardiographic surveillance may be advisable.
References
- Fender EA, Zack CJ, Nishimura RA. Isolated tricuspid regurgitation: outcomes and therapeutic interventions. Heart. 2018;104:798–806.
- Singh JP, Evans JC, Levy D, et al. Prevalence and clinical determinants of mitral, tricuspid, and aortic regurgitation (the Framingham Heart Study). Am J Cardiol. 1999;83:897–902.
- Guta AC, Badano LP, Tomaselli M, et al. The pathophysiological link between right atrial remodeling and functional tricuspid regurgitation in patients with atrial fibrillation: a three- dimensional echocardiography study. J Am Soc Echocardiogr. 2021;34:585–594.
- Shiran A, Najjar R, Adawi S, Aronson D. Risk factors for progression of functional tricuspid regurgitation. Am J Cardiol. 2014;113:995–1000.
- Mutlak D, Khalil J, Lessick J, Kehat I, Agmon Y, Aronson D. Risk factors for the development of functional tricuspid regurgitation and their population-attributable fractions. J Am Coll Car- diol Img. 2020;13:1643–1651.
- Axtell AL, Bhambhani V, Moonsamy P, et al. Surgery does not improve survival in patients with isolated severe tricuspid regurgitation. J Am Coll Cardiol. 2019;74:715–725.





No comments yet!